Tibial ganglion cysts may be a cause of persistent pain following TKA and revision arthroplasty is a viable option for symptomatic improvement with good post-operative outcomes.
Dr. Jacob Laperche, Total Joints Research Fellow, University Orthopedics, 1 Kettle Point Ave, East Providence, Rhode Island 02914. E-mail: jacoblaperche@gmail.com
Introduction: Intraosseous ganglion cysts are an uncommon variant found in the subchondral bone. We report here the development of an intraosseous ganglion cyst of the proximal tibia in the setting of a prior left total knee arthroplasty (TKA) with an all-polyethylene tibial component.
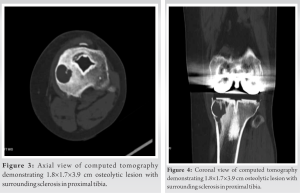
Case Report: The cyst was diagnosed on routine follow-up radiographs approximately 4 years status post-TKA. Although initially asymptomatic, 1 year later the patient presented with progressive knee pain and ambulation limitations, so revision TKA was indicated. Computed tomography confirmed an osteolytic lesion suggestive of a penetrating ganglion. Given the absence of malrotation or malalignment of the well-fixed femoral component, the decision was made to proceed with the revision of the stemmed tibial component cemented through a porous tantalum cone. Postoperatively, the patient had complete resolution of pain and instability with 0–120° of stable range of motion, which has persisted to the latest follow-up at over 6 months post-operative, with radiographic resolution of the cyst.
Conclusion: This case demonstrates a ganglion cyst surrounding total knee implants as a possible source of persistent pain following TKA. To our knowledge, this is the first report of such a case. This case demonstrates that refractory painful knee implants secondary to tibial ganglion cysts can be treated successfully with revision arthroplasty.
Keywords: Knee revision arthroplasty, ganglion cyst, porous cone, outcomes.
Intraosseous ganglion cysts are lesions located in the subchondral bone. Ganglion cysts found at the knee are typically located in periarticular soft tissues and may be multiloculated [1]. Patients typically present with a mass of variable size and persistent pain that worsens with increased usage of the knee joint. Intraosseous ganglia in the unreplaced native knee are relatively uncommon and usually occur among adults in the 4th and 5th decades of life, primarily in the proximal tibia [2]. These types of cysts are reported to not usually be associated with arthritis or meniscal tears but have been linked with cases of trauma in some studies [3]. The standard treatment for intraosseous ganglia is surgical excision of the lesion followed by bone grafting to prevent collapse of the bone around the removed lesion. Computed tomography (CT) and T2-weighted magnetic resonance imaging (MRI) are the best imaging methods for identifying lesion morphology [3]. Prior studies have reported intraosseous ganglion cysts requiring surgical excision and curettage, though to our knowledge, there are no reports describing the management of intraosseous ganglion cysts in the setting of a prior total knee arthroplasty (TKA). We present the case of an intraosseous ganglion cyst of the proximal tibia diagnosed 4 years after index TKA treated with surgical excision and revision of the tibial component using a porous metal bone substitute to fill the cyst defect.
A 53-year-old female with a history of an uncomplicated left TKA using a cemented, posterior-stabilized femur and all-polyethylene tibia implant in 2017 presented for her 4-year post-operative follow-up. Initial routine post-operative radiographs did not demonstrate any abnormality (Fig. 1). However, subsequent routine anterior-posterior (AP) and lateral radiographs revealed a large, expansile lesion in the medial aspect of the proximal tibia (Fig. 2).
Over the ensuing 6 months, the patient reported increasing pain and limited ambulation secondary to pain. Physical examination of the left knee demonstrated 0–120° of range of motion and stability to varus and valgus stress through the flexion-extension arc. Radiographs (AP and lateral views) showed progressive growth of the pre-existing cyst. An infection workup was initiated; the erythrocyte sedimentation rate was 12 mm/h (normal threshold is 0-20 mm/hr) and C-reactive protein was 1.89 mg/L ( normal threshold is 8-10 mg/L) [4]. The knee was aspirated yielding 100 nucleated cells with 9% neutrophils. Aspiration cultured for 14 days incubation did not yield any organisms. Based on Musculoskeletal Infection Society criteria the patient scored 0 which indicates low concern for infection [5]. After a discussion with the patient about the risks and benefits of revision TKA, the patient elected to proceed.
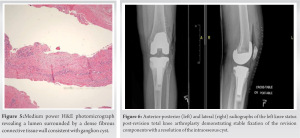
The surgery was performed through the previous midline incision, followed by a medial parapatellar arthrotomy. An extensive synovectomy was performed. The tibial implant component was removed, and a high-speed burr was used to remove retained cement from the proximal tibia. Examination of the tibial component did not demonstrate significant wear or damage. A cyst was identified in the medial tibia metaphysis, and the cyst wall was curetted and sent to pathology. Pathology confirmed a fibrous-lined cyst consistent with a ganglion cyst (Fig. 4). The femoral and patellar implants were found to be well-fixed and were left in place. A clean-up cut was made on the proximal tibia, and a trail tibial component and bearing were placed. The tibia was prepared for a porous tantalum cone (48–15 mm) using trials as a guide. The final cone was placed after trialing and intra-operative assessment. A final stemmed tibial component was cemented through the cone. A final PS polyethylene bearing was placed after trial optimization. Post-operative X-rays showed adequate initial fixation of the revision components with resolution of the intraosseous cyst (Fig. 5). The patient’s inpatient course was uncomplicated, and she was discharged home with services on hospital day 1. At latest office follow-up, at >6 months post-operative, she presented with resolved symptoms of pain and is walking unrestricted distances. On examination, her knee was stable from 0 to 120 to varus and valgus stress. Post-operative X-ray imaging demonstrated stable implants (Fig. 6).
We present a rare case of an intraosseous proximal tibial ganglion cyst in the setting of a previous TKA, which progressed in size and became symptomatic, necessitating tibial component revision. Intraosseous proximal tibia ganglion cysts in native knees are uncommon. In a case series of 54 patients with lower extremity ganglia by Rozbruch et al., knee-associated ganglia accounted for only 33% of patients with only three of those patients having intraosseous ganglia [6]. To our knowledge, there are no reports describing the management of proximal tibial ganglion cysts status post prior TKA. The standard management of intraosseous ganglion cysts requires a comprehensive history, physical examination, and imaging workup. Ultimately, symptomatic intraosseous ganglion cysts are treated with surgical excision and curettage with bone grafting [2]. There is limited literature on the reported resolution of symptoms and recovery time, which likely will vary based on the location of the cyst and surrounding anatomy. In one series of lower extremity ganglia, 86% of patients treated with excision and curettage had no pain at an average follow-up of 5.9 years [6]. Less is known specifically about patient outcomes after treatment of symptomatic tibia ganglion however in a case report of treatment of ganglion cyst of the distal tibia, the patient reported full weight-bearing after 2 months [3]. There is a low rate of recurrence or complications after surgery for lower extremity ganglion cysts with reports of only 6.1% of ankle and foot ganglion cysts recurring after curettage [7]. Maheshwari et al. describe a case of a ganglion cyst in the proximal tibio-fibular joint in association with a previous TKA requiring proximal fibulectomy. The cyst was previously present for 12 years but became symptomatic and expansive after the TKA. Similarly, the cyst observed in our patient only became symptomatic and expansile after the TKA. Maheshwari et al. proposed that increased mechanical stress and/or an inflammatory reaction to wear debris served as pathogenesis for cyst formation after TKA [1]. Periprosthetic cysts associated with osteolysis and implant polyethylene wear have been described in the literature [8]. The mechanism is thought to be due to abrasive wear of the surface of the tibial insert, which could produce small polyethylene particles that are associated with osteolysis and cyst development [8]. All-polyethylene tibial total knee replacements have an excellent long-term track record and are generally found to have less wear and osteolysis as they do not have a backside component to produce wear. Houdek et al. reviewed 31,939 patients undergoing a primary TKA over a 43-year period and found that all polyethylene total knee replacements had significantly improved implant survival, reduced rates of post-operative infection, fracture, and tibial component loosening compared to metal-backed designs [9]. This is thought to be due to the polyethylene designs being non-modular, and so do not suffer from the backside wear phenomenon [10]. In our case, there was no wear debris or significant evidence of wear on the explanted tibial component noted intraoperatively making a wear-related mechanism of cyst formation less likely. In similar cases to the one we report, we recommend a thorough history, examination, and imaging studies, to evaluate the chronology of symptoms and progression of the lesion. In patients with symptomatic lesions limiting ambulation, we recommend a thorough pre-operative evaluation including aspiration to risk stratify infection and CT for further understanding the size and extent of the lesion. In benign-appearing lesions, surgical excision and curettage for ganglion cysts have been shown to be effective. However, it is crucial to consider the fixation and stability of the knee replacement components. In our case, the proximity of the cyst to the implant required revision with a cemented stemmed tibial tray and porous tantalum cone to treat the defect left after cyst removal and for adequate fixation. Given the rarity of peri-implant ganglion cysts, and significant potential variability in cyst size, occurrence, and location in relation to implants, we recommend each case require a patient-specific surgical plan ideally in the care of a well-trained arthroplasty surgeon experienced in revision knee replacement.
Potential limitations
This is a single case report meaning the success rate of similar treatment may have some differences when applied to other similar patients. In addition, while 6 months of follow-up is acceptable for establishing resolution of symptoms, longer-term follow-up is required to monitor for cyst recurrence.
To our knowledge, there are no reports of intraosseous proximal tibial ganglion cyst in the setting of a prior left TKA causing pain and requiring revision TKA. In situations where cystic lesions progress in size or become clinically symptomatic, treatment with tibial component revision and use of cemented stem through a porous metal bone substitute is recommended and was successful in our case. Further studies are necessary to examine the association between TKA and intraosseous proximal tibial ganglion cysts regarding incidence, symptom severity, and recovery, though the rarity of these cases would make this type of study challenging.
Persistent pain following TKA can be a complex issue with no clear cause at times. This case represents the importance of serial imaging to following the progression and find potential causes. This case represents a cause to suspect ganglion cysts around the implants as a potential cause for this persistent pain. Good results following revision arthroplasty for this knee pain are also useful for surgeons to report to their patients and feel comfortable performing these revisions will benefit their patients.
References
- 1.Maheshwari AV, Muro-Cacho CA, Temple HT. Aggressive proximal tibio-fibular joint ganglion cyst after a total knee arthroplasty--a case report. Knee 2008;15:411-5. [Google Scholar]
- 2.Daly PJ, Sim FH, Beabout JW, Unni KK. Intraosseous ganglion cysts. Orthopedics 1988;11:1715-9. [Google Scholar]
- 3.Mahvash M, Hashemi M, Maslehaty H, Doukas A, Petridis AK, Mehdorn HM. Post-traumatic extensive knee ganglion cyst. Clin Pract 2011;1:e61. [Google Scholar]
- 4.Alijanipour P, Bakhshi H, Parvizi J. Diagnosis of periprosthetic joint infection: The threshold for serological markers. Clin Orthop Relat Res 2013;471:3186-95. [Google Scholar]
- 5.Parvizi J, Tan TL, Goswami K, Higuera C, Della Valle C, Chen AF, et al. The 2018 definition of periprosthetic hip and knee infection: An evidence-based and validated criteria. J Arthroplasty 2018;33:1309-14.e2. [Google Scholar]
- 6.Rozbruch SR, Chang V, Bohne WH, Deland JT. Ganglion cysts of the lower extremity: An analysis of 54 cases and review of the literature. Orthopedics 1998;21:141-8. [Google Scholar]
- 7.Ferkel RD, Field J, Scherer WP, Bernstein ML, Kasimian D. Intraosseous ganglion cysts of the ankle: A report of three cases with long-term follow-up. Foot Ankle Int 1999;20:384-8. [Google Scholar]
- 8.Akisue T, Kurosaka M, Matsui N, Yamaguchi M, Hasuda K, Bauer TW, et al. Paratibial cyst associated with wear debris after total knee arthroplasty. J Arthroplasty 2001;16:389-93. [Google Scholar]
- 9.Houdek MT, Wagner ER, Wyles CC, Watts CD, Cass JR, Trousdale RT. All-polyethylene tibial components: An analysis of long-term outcomes and infection. J Arthroplasty 2016;31:1476-82. [Google Scholar]
- 10.Browne JA, Gall Sims SE, Giuseffi SA, Trousdale RT. All-polyethylene tibial components in modern total knee arthroplasty. J Am Acad Orthop Surg 2011;19:527-35. [Google Scholar]