As neurofibromatosis is a disorder of multiple systems, the patient may present to the Orthopedic, Dermatology, Neurology, or any other OPD, making it important for all specialists to have basic knowledge of the same.
Dr. Ratnakar Ambade, Department of Orthopaedics, Datta Meghe Institute of Medical Sciences (Deemed To Be University), Wardha, Maharashtra, India. E-mail: drambade@hotmail.com
Background: Neurofibromatosis-1 (NF-1) is a neurocutaneous disorder, primarily affecting the skin and nervous system. Concomitant multi-system involvement is also seen. Orthopedic manifestations of NF-1 are one area that is understudied and underreported, highlighting the importance of this case report.
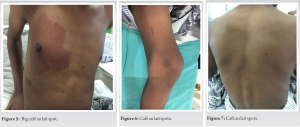
Case Report: A 16-year-old male presented with painless swelling on the posteromedial aspect of the lower right tibia, which was confirmed to be a dysplastic mass on biopsy. Physical examination also revealed cafe au lait macules and axillary freckling, leading to a diagnosis of NF-1.
Discussion: Bony lesions in NF-1 patients mainly include the spine and tibia. Congenital tibial dysplasia is commonly associated with NF-1 and may progress to pseudoarthrosis if early management is not started. Treatment modalities include excision, bracing, and fixation.
Conclusion: Further research is required to have a more comprehensive view of NF-1 and orthopedics, to diagnose and manage such bony complications.
Keywords: Neurofibromatosis-1, orthopedic manifestations, tibial dysplasia.
Neurofibromatosis-1 (NF-1) is a complex genetic disorder related to germline mutations in the NF-1 tumor suppressor gene. Almost all affected persons have pigmentary lesions and dermal neurofibromas. Some have skeletal abnormalities, brain and peripheral nerve tumors, learning disabilities, and behavioral issues. Skeletal system presentations include osteoporosis, pathological fractures, pseudoarthrosis in long bones, and structural deformities in the spine. It manifests at a young age, and hence, it is important to identify and manage the skeletal effects of NF-1 as early as possible to ensure proper development of the bones and a good quality of life. We report a case of a young adult with relatively uncommon tibial involvement and briefly review the skeletal manifestations of NF-1.
A 16-year-old male presented with a painless swelling on the posteromedial aspect of the lower one-third of the right tibia. The swelling had been present since he was 8 years old and had slowly progressed to the size of 8 × 5 cm. The overlying skin had numerous folds giving an elephantiasis-like appearance (Fig. 1). X-ray of the affected limb showed a deforming mass arising from the posteromedial aspect of the ankle and foot (Fig. 2 and 3).

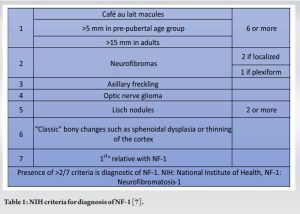
NF-1 is a neurocutaneous syndrome that can affect multiple organ systems and has diverse presentations. It is associated with a mutation in the long arm of chromosome 17, which codes for the protein neurofibromin and is inherited in an autosomal dominant pattern, hence having a relatively common incidence of 1 in 3000 live births [1]. The syndrome is named after the characteristic benign “neurofibromas” [2], consisting of Schwann cells, fibroblasts, endothelial cells, mast cells, etc. [3]. More than 80% of adults with NF-1 will develop neurofibromas by the age of 20 [1]. Neurofibromas are classified based on their anatomical distribution into localized, plexiform, and diffuse types. Plexiform neurofibromas, found in one extremity only, are typical of the syndrome, seen in 26% of the NF-1 patients [2], and have a 2–5% chance of malignant transformation [4]. Cutaneous manifestations include café au lait spots, which are hyper-pigmented flat lesions [3], which are the earliest and most common manifestation of NF-1, seen in 90–99% of patients [3]. The presence of freckles in NF-1 is in areas of skin folds such as the axilla, inguinal region, breast folds, and neck. Patients of NF-1 are predisposed to developing multiple neoplasms due to associated p53 gene mutation [5]. Neurofibrosarcoma, pheochromocytoma, leukemia, and melanoma are the commonly seen malignancies [1]. Optic nerve gliomas are seen in 6.6% of patients [1], while Lisch nodules are asymptomatic hamartomas of the iris. Up to 75% of NF-1 patients develop some sort of intellectual disability and developmental delay [5]. Lifestyle illnesses such as hypertension, stroke, and heart disease are also common [1]. Localized overgrowth of bone and soft-tissue gives an elephantiasis-like appearance [3], which is also attributed to lymphadenopathies presenting as edema [6]. The NIH, USA has given criteria for the diagnosis of NF-1 [7] (Table 1). The index patient had café au lait macules and axillary freckling and fulfilled two of these criteria.
Orthopedic manifestations
A “PubMed” search was conducted using the search terms “NF-1” and “orthopedics.” There were 568 case reports, out of which 43 reported orthopedic manifestations of NF-1, while only 4 reports were about tibial pathologies or dysplasia. Tibial pathologies have been rarely reported in NF-1. NF-1 of the musculoskeletal systems has many facets. Since neurofibromin is a regulator of bone development, mutations of its gene affect bone metabolism. Bone mineral density met the criteria for osteopenia in 48% and for osteoporosis in 25% of NF-1 patients in one study [8]. Generalized weakness, osteomalacia, short stature, and macrocephaly are also observed [9]. Osteolysis may be seen uncommonly [10]. Classical sphenoidal changes and primary bone dysplasia are also reported [11]. NF-1 of the bones has a strong affinity for the spine and tibia. Spinal deformities are the most common orthopedic manifestation of NF-1, seen in 10–30% of diagnosed cases [9]. The vertebrae may be non-dystrophic or may show dystrophic changes such as scalloping, wedging, or external rotation [1, 5]. Scoliosis can be of the dystrophic or non-dystrophic type. Dystrophic scoliosis is classically seen in NF-1, while non-dystrophic scoliosis is more common and bears a close resemblance to adolescent idiopathic scoliosis [3]. It has a poor prognosis and has a tendency to progress to dystrophic type, a process called “modulation” [1]. Cervical deformity in NF-1 is seen in the form of kyphosis [12]. It presents with neck pain and often there is some degree of neurological deficit.
Tibial involvement
Congenital dysplasia of the tibia (CDT) is the second most common orthopedic complication of NF-1. A rare occurrence in the general population, only 1 in 140,000 live births have CDT, while 84% of CDT patients fulfill the criteria for NF-1 [12]. CDT presents as unilateral or bilateral, antero-lateral [9], or antero-medial [13] tibial bowing. Limb length inequality and skin changes such as dimpling and ring constrictions can be seen due to the deformity [9]. Our index patient presented with tibial dysplasia, which was unique in that the swelling was posteromedial and was noticed at 8 years of age, a relatively late presentation. Evaluation is done through plain X-ray. The spectrum of radiologic appearances of CDT includes simple bowing, dystrophic bone, and narrowed medullary cavity [1, 12]. These bones are prone to developing pathological fractures and pseudoarthrosis. Cortical thickening may also be seen, though it is inconsistent with the NIH criteria of “thinning of bony cortex” [1]. Due to a lack of literature, no conclusive line of management has been agreed on for CDT. It appears that treating CDT without fracture with bracing as a prophylactic measure is beneficial. Ankle-foot orthosis and propylene knee-ankle-foot orthosis may be used to be worn till the skeletal maturity is achieved [5]. In case of fracture, external fixation may be employed using the Ilizarov apparatus. It is advantageous because of its ability to rectify limb-length inequality, angular deformity, and ankle valgus [3]. Dysplastic lesions may be surgically excised to rectify the deformity while maintaining the cosmetic appearance of the affected part. Other rare orthopedic manifestations of NF-1 include cystic lesions of long bones and subperiosteal bone proliferation. Soft-tissue masses causing deformity of joints predisposed to the development of subluxation or dislocation, especially in hip bones [4]. Recurrent subluxations are a risk factor for secondary osteoarthritis [8]. Neurofibromatosis-2 is also an autosomal dominant disease but rarer, affecting 1 in 40,000 live births, and affects the long arm of chromosome 22 [3]. It also presents multiple schwannomas. It can be differentiated from NF-1 from its affinity for central nervous tissue, hence presenting with characteristic bilateral vestibular acoustic neuromas, ependymomas, and meningiomas. Spinal cord involvement can be seen in the form of intradural tumors and intramedullary masses [11], but there are no known orthopedic manifestations of NF-2 [8, 14].
Although well recognized as a development of NF-1, tibial dysplasia is still sparsely reported, making this case study an important part of the discourse on orthopedics in NF-1. CDT in association with NF-1 can be diagnosed early provided some degree of suspicion of neurofibromatosis is present. Thorough history taking and examination are important, especially to ensure early commencement of management so that complications due to neglect do not arise.
A patient with neurofibromatosis can be diagnosed based on any type of presentation. Thorough clinical examination of all patients is imperative, irrespective of the department they present to. Common syndromes and disorders should be kept in mind while treating patients with multiple complaints.
References
- 1.Feldman D, Jordan C, Fonseca L. Orthopaedic manifestations of neurofibromatosis type 1. J Am Acad Orthop Surg 2010;18:346-57. [Google Scholar]
- 2.Bano S, Prasad A, Yadav S, Chaudhary V, Sachdeva N. Elephantiasis neuromatosa of the lower limb in a patient with neurofibromatosis type-1: A case report with imaging findings. J Paediatr Neurosci 2010;5:59-63. [Google Scholar]
- 3.Crawford A, Schorry E. Neurofibromatosis in children: The role of the orthopaedist. J Am Acad Orthop Surg 1999;7:217-30. [Google Scholar]
- 4.Saibaba B, Sen R, Sharma M, Nahar U. Pathological fracture dislocation of the acetabulum in a patient with neurofibromatosis-1. Indian J Orthop 2016;50:103. [Google Scholar]
- 5.Vitale M, Guha A, Skaggs D. Orthopaedic manifestations of neurofibromatosis in children: An update. Clin Orthop Related Res 2002;401:107-18. [Google Scholar]
- 6.Finsterer J, Stubenberger E, Tschakoschian S, Stoellberger C. Lymphangiopathy in neurofibromatosis 1 manifesting with chylothorax, pericardial effusion, and leg edema. Int J Gen Med 2013;743-6. [Google Scholar]
- 7.NIH Diagnostic Criteria for NF1. Available from: https://arup.utah.edu/database/SPRED1/NIH_criteria.html [Last accessed on 2021 Oct 11]. [Google Scholar]
- 8.Patel J, Whiting J, Jones D. Secondary knee osteoarthritis due to neurofibromatosis type 1 treated above the knee amputation: A case report. Case Rep Orthop 2013;2013:782106. [Google Scholar]
- 9.Available from: https://emedicine.medscape.com/article/1260124-print [Last accessed on 2021 Sep 19]. [Google Scholar]
- 10.Shen Y, Chen F. Unusual form of the distal bone defect of ulna with neurofibromatosis type 1. Medicine 2019;98:e17226. . [Google Scholar]
- 11.Egelhoff JC, Bates DJ, Ross JS, Rothner AD, Cohen BH. Spinal MR findings in neurofibromatosis types 1 and 2. AJNR Am J Neuroradiol 1992;13:1071-7. [Google Scholar]
- 12.Mladenov K, Spiro A, Krajewski K, Stücker R, Kunkel P. Correction to: Management of spinal deformities and tibial pseudarthrosis in children with neurofibromatosis type 1 (NF-1). Childs Nerv Syst 2021;Oct;37(10):3281. [Google Scholar]
- 13.Johnston C, Birch J. A tale of two tibias: A review of treatment option for congenital pseudarthrosis of the tibia. J Child Orthop 2008;2:133-49. [Google Scholar]
- 14.Kashif S. Neurofibromatosis induced hip arthritis. An unusual presentation. Am J Case Rep 2014;15:79-81. [Google Scholar]