A comprehensive assessment of the patient’s history, anatomical considerations, utilizing imaging techniques for accurately locating the fractured catheter within the epidural space, enabling a targeted and precise retrieval procedure in case of epidural catheter breakage is required.
Dr. Subith S, Department of Orthopaedics, Topiwala National Medical College and B.Y.L Nair Hospital, Mumbai, Maharashtra, India. E-mail: s.subith24@gmail.com
Introduction: The accidental breakage of an epidural catheter during placement or removal poses a rare but challenging situation in clinical practice. This case report presents the successful removal of a broken epidural catheter and highlights the management strategies employed.
Case Report: A 41-year-old male patient underwent a planned orthopedic implant removal surgery under epidural anesthesia. During catheter removal, a portion of the catheter fractured and remained lodged within the epidural space. The patient experienced persistent pain and concern regarding the retained fragment, necessitating immediate intervention. A multidisciplinary team comprising an orthopedic surgeon, neurosurgeon, anesthesiologist, and radiologists collaborated to develop a tailored retrieval strategy. Magnetic resonance imaging aided in localizing the fractured catheter fragment. Using a standard midline posterior approach, the catheter was safely removed without any complications. Post-retrieval monitoring revealed no adverse events, and the patient reported resolution of pain and improved satisfaction.
Conclusion: Retrieving a broken epidural catheter requires a systematic and individualized approach. This case report contributes to the existing literature by providing insights into managing this rare complication, highlighting the importance of a multidisciplinary team, appropriate imaging, and meticulous retrieval techniques to ensure patient safety and optimal outcomes.
Keywords: Epidural catheter, spine surgery, broken catheter, explorative laminectomy.
Epidural catheters play a pivotal role in modern health care, providing effective pain management solutions for patients undergoing various surgical procedures and experiencing chronic pain. These slender, flexible tubes are carefully inserted into the epidural space to deliver pain relief medications directly to the spinal cord. While epidural catheters are generally safe and efficient, complications can occasionally arise, including rare instances of catheter breakage. Retrieving a broken epidural catheter presents a complex and delicate challenge for health-care providers. In this article, we will delve into the intricate world of managing catheter breakage, exploring the potential causes, assessment methods, and the various techniques employed to successfully retrieve a fractured catheter. Understanding these intricacies is crucial for anesthesiologists, surgeons, and medical professionals to ensure the safety and well-being of their patients while navigating this uncommon but significant clinical scenario.
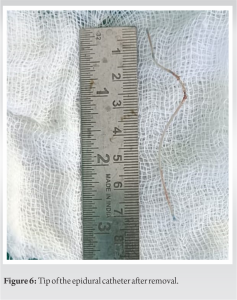
A 41-year-old male sustained fractures in the left-sided femur shaft, proximal tibia, and left calcaneum. The patient had initially been managed elsewhere and underwent intramedullary interlocking nail fixation for the femur fracture, anterolateral plating for the tibia fracture, and percutaneous screw fixation for the calcaneum fracture. After 1 year, the patient presented to our hospital for implant removal, as clinical and radiological examinations indicated that all fractures had successfully united. The patient was scheduled to remove all implants under spinal epidural anesthesia. Following sterile aseptic precautions, an 18G Tuohy epidural catheter (PORTEX Epidural Minipack System 1) was inserted. After several attempts, a space was identified at 4 cm, and the catheter was threaded through the needle on confirmation of the space. The placement of the catheter in the epidural space was confirmed by a meniscus sign and fixed at 10 cm. Subsequently, a 25G spinal anesthesia needle was inserted into the subarachnoid space at the L4-L5 level and 3 cc of 0.5% heavy bupivacaine and 60 µg injection buprenorphine injected as an additive after confirming the free flow of cerebrospinal fluid and negative aspiration of blood. The procedure began with removing the proximal tibia and calcaneum implants, followed by the femur implant. The surgery proceeded uneventfully. However, during the post-operative removal of the epidural catheter, it was observed that approximately 8 cm of the catheter was broken and missing (Fig. 1).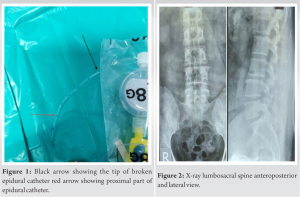
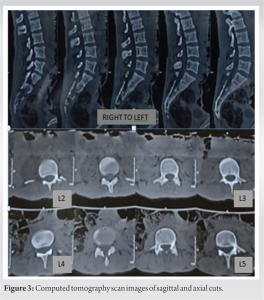
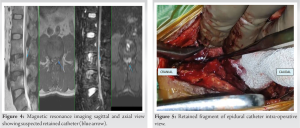
A routine practice in many surgical procedures is the placement of an epidural catheter in the epidural space to provide anesthesia. A rare complication is the breakage of the epidural catheter during its insertion or removal in the epidural space, with only a few reported cases. Faulty design, faulty insertion or withdrawal technique, and entrapment by bony or ligamentous tissues during removal have been associated with epidural catheter breakage [1]. García et al. [2] reported the presence of a knot at the tip of the catheter preventing withdrawal was the reason for breakage. Other reported causes include Nikhilesh et al. [3] multiple attempts; Reena and Vikram [4] excessive length of the catheter has been inserted. In our case, multiple attempts for insertion are the cause of the breakage of the catheter. Even though the catheter is radio-opaque, radiological imaging tests are not very helpful in locating it. Computed tomography, MRI, and ultrasonography have all been used with variable results among these radiographs [1]. In our case, X-ray and CT revealed nothing but MRI helped to find the probable location of the retained catheter. Complications related to the retained epidural catheter tip, other than infection, back pain, and neurological deficit; include radicular pain due to a retained fragment of the epidural catheter [5] and lumbar stenosis [6]. According to Sardana et al., [7] and Mitra and Fleischmann [8] the fragment may be left alone in most cases, arguing that any sequestered catheter fragment is inert and should produce no foreign body reaction, whereas surgical removal could do more harm than good. If a catheter fragment is retained within the spinal canal, Tarukado et al., [9] propose that surgery should be considered before adhesions advance, while Ugboma et al. [10] recommend aggressive surgical exploration and extraction, even in asymptomatic patients. In our case the patient experienced persistent pain and concern regarding the retained fragment, necessitating immediate intervention.
Adherence to standard guidelines for epidural insertion and removal is crucial to prevent such incidents. When the epidural catheter breaks, it presents an ethical dilemma for the anesthetist. In cases where this unfortunate event transpires despite taking precautionary measures, it is essential to promptly inform the patient. The approach to managing asymptomatic cases is conservative and involves utilizing imaging studies to pinpoint the location of the broken fragment. Regular follow-up is maintained to detect potential complications that may arise in the months or even years following the incident. Surgical intervention is considered for cases with symptomatic presentations.
There should be a comprehensive assessment of the patient’s history, and anatomical considerations, utilizing imaging techniques for accurately locating the fractured catheter within the epidural space, enabling a targeted and precise retrieval procedure.
References
- 1.Palaria U, Das A, Jakhwal C. Broken epidural catheter: What next to do? Indian J Clin Anaesth 2018;10:289-91. [Google Scholar]
- 2.García RA, Muñoz-Martínez AC, Hoyos-Pescador R, De la Torre-Espinosa R. Retained epidural catheter: A rare complication. Report of two cases. Colomb J Anesth 2017;45:4-7. [Google Scholar]
- 3.Nikhilesh B, Vadhanan P, Balakrishnan K. Epidural catheter catastrophe-breakages during procedure and outcome in three cases. Indian J Clin Anaesth 2020;7:719-21. [Google Scholar]
- 4.Reena, Vikram A. Fracture of epidural catheter: A case report and review of literature. Saudi J Anaesth 2017;11:108-10. [Google Scholar]
- 5.Blanchard N, Clabeau JJ, Ossart M, Dekens J, Legars D, Tchaoussoff J. Radicular pain due to a retained fragment of epidural catheter. Anesthesiology 1997;87:1567-9. [Google Scholar]
- 6.Staats PS, Stinson MS, Lee RR. Lumbar stenosis complicating retained epidural catheter tip. Anesthesiology 1995;83:1115-8. [Google Scholar]
- 7.Sardana DK, Panaych K, Samra T. Broken epidural catheter: An anesthesiologist’s dilemma. J Case Rep 2017;7:116-8. [Google Scholar]
- 8.Mitra R, Fleischmann K. Management of the sheared epidural catheter: Is surgical extraction really necessary? J Clin Anesth 2007;19:310-4. [Google Scholar]
- 9.Tarukado K, Oda T, Tono O, Suetsugu H, Doi T. A retained epidural catheter fragment treated by surgery. Asian Spine J 2015;9:461-4. [Google Scholar]
- 10.Ugboma S, Au-Truong X, Kranzler LI, Rifai SH, Joseph NJ, Salem MR. The breaking of an intrathecally-placed epidural catheter during extraction. Anesth Analg 2002;95:1087-9. [Google Scholar]