The coexistence of two distinct types of tumors in the same region of the body sheds light on a rare occurrence in the medical field. This rare occurrence serves as a reminder of the ongoing challenges and advancements in the field, highlighting the ongoing need for comprehensive and meticulous diagnostic methods.
Dr. Muhand Alkameshki, Department of Orthopaedics Surgery and Traumatology, Centre Hospitalier Régional Universitaire de Tours, Tours, France/Department of Orthopaedics Surgery, Suhar Hospital, Suhar, Oman. E-mail: dr.myyk@hotmail.com
Introduction: We encountered a unique case of a patient with two distinct tumors coexisting in the same thigh. To the best of our knowledge, this combination of tumors in the same anatomical region has not been previously described in the literature.
Case Report: This case report describes a 38-year-old Caucasian male with a painless mass in his right thigh, which was later diagnosed as a hybrid tumor composed of low-grade fibromyxoid sarcoma and sclerosing epithelioid fibrosarcoma, as well as a second tumor, which was diagnosed as a hibernoma. The patient underwent neoadjuvant chemotherapy and surgical excision, followed by adjuvant radiotherapy and treatment for metastatic recurrence.
Conclusion: The rarity of this case highlights the need for interdisciplinary collaboration and further investigations into the behavior and management of hybrid tumors. This case also underscores the importance of an accurate histological diagnosis aided by immunohistochemistry and molecular analyses.
Keywords: Evan’s tumor, fibromyxoid sarcoma, sclerosing epithelioid fibrosarcoma, metastasis, hibernoma, soft-tissue tumors, sarcoma.
Soft-tissue tumors are a highly heterogeneous group of neoplasms that present a diagnostic challenge for clinicians and pathologists. Of these, hybrid tumors are rare entities characterized by the coexistence of two or more distinct histological types [1]. One such hybrid tumor is low-grade fibromyxoid sarcoma/sclerosing epithelioid fibrosarcoma (LGFMS/SEF), a rare and aggressive neoplasm that typically affects young adults [1]. Another uncommon tumor that we noticed in our case was hibernoma. Hibernoma is a benign lipomatous tumor arising from brown adipose tissue [2]. The concomitant presence of multiple soft-tissue tumors within the same region of the body is an extremely rare phenomenon, with only a few cases reported in the literature [3-6]. In this case report, we describe a patient with LGFMS/SEF and hibernoma coexisting in the same thigh and discuss the clinical, radiologic, pathologic, and prognostic implications of this rare tumor association.
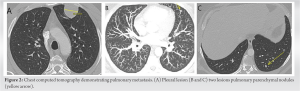
A 38-year-old male patient presented with a painless mass on his right thigh. He reported no significant medical history other than psoriasis and had no family history of cancer. Physical examination revealed a palpable non-tender mass measuring approximately 30 cm along its long axis. No overlying skin discolorations or ulcerations were observed. Imaging studies, including magnetic resonance imaging, showed a soft-tissue tumor in the right quadriceps, 22 cm long axis, heterogeneous, taking contrast, in contact with the femur on its external face. This was associated with a heterogeneous, 15-cm fat mass in the posterior compartment (Fig. 1).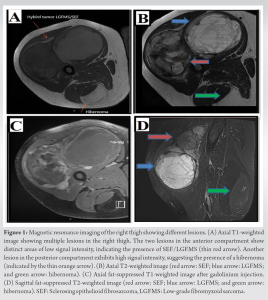
Pathological examination of the surgical biopsy of the anterior mass favored a LGFMS, whereas the histological characteristics of the posterior mass were that of a hibernoma. A biopsy of the pleural lesion revealed pleural metastatic localization of a LGFMS. Based on the biopsy findings of the subpleural mass, which revealed the presence of sarcoma metastasis alongside multiple metastatic pulmonary nodules, neoadjuvant chemotherapy with a six-cycle regimen of adriamycin was proposed.
Procedure details
The patient is placed under general anesthesia in the supine position; preventive antibiotic therapy is administered.
First Stage:
Sarcoma of the quadricipital compartment
A large anterior approach is made to carry out the biopsy path, moving to the outer edge of the rectus femoris. Passage through the vastus muscles, maintaining a safety plan regarding the tumor raising the tumor from distal to proximal. In Proximal and lateral, taking away part of the vastus aponeurosis and detached from the lateral subtrochanteric ridge. The excision is macroscopically complete and distant.
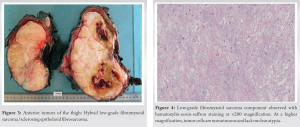
Weight of the tumor: 4 kg 300 (Fig. 3).
Second Stage:
Hibernoma in contact with the hamstrings.
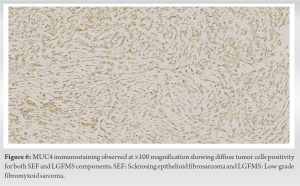
A longitudinal incision is made carrying the biopsy path, and the lesion is excised with a safety border corresponding to the tumor capsule. The hamstrings are preserved, and no sciatic nerve exposure occurs. The posterior mass (hibernoma) was resected, with a small safety border corresponding to the tumor capsule. Histological examination of the anterior mass revealed a well-limited intramuscular tumor associated with two distinct components, a LGFMS and a SEF, in approximately equivalent proportions. Areas of LGFMS had alternating low-to-moderate cellularity, and a fibrohyaline to fibromyxoid matrix, as well as monotonous spindle cells with regular nuclei which were arranged in short bundles or bands. A few collagen rosettes were observed (Fig. 4). The SEF contingent was mainly found in the proximal part of the tumor and was composed of monotonous epithelioid cells arranged in cords spanning the dense fibrous stroma (Fig. 5).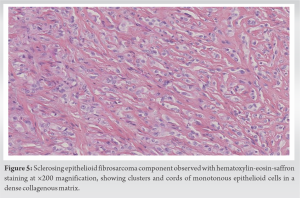
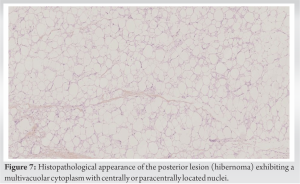
The posterior thigh mass revealed a well-differentiated adipose tumor consistent with a hibernoma. The tumor displayed a lobular architecture, with adipocytes exhibiting finely granular and eosinophilic multivacuolar cytoplasm and central or paracentral nuclei (Fig. 7). Complete tumor resection was performed, and adjuvant radiotherapy was administered. After 6 months, the patient underwent a left upper lobectomy. Eight months later, a right wedge resection of the middle lobe was performed due to the presence of pulmonary metastases. After 15 months, a recurrence of lung metastases was identified, and the patient was treated with pazopanib. At the 2-year post-operative follow-up after the surgical resection of the two tumors of the thigh, the patient had no other issues related to the tumors.
Soft-tissue sarcomas are rare, malignant tumors with an incidence rate of approximately 5 cases/100,000. These malignancies can be further categorized into 70 subtypes, each with a distinct morphology that can influence clinical behavior and specific treatments [1]. In our case report, we present a remarkable and rare occurrence of a hybrid tumor composed of two distinct types of sarcomas: LGFMS and SEF, simultaneously existing with a hibernoma within the same region in the right thigh. It is noteworthy that there are limited data available on individuals with two concurrent tumors coexisting within the same location, making this a particularly exceptional case [4-6]. Although the previous studies have reported the coexistence of two sarcomas using both synchronous and metachronous cases, they did not involve the same anatomical location [3]. This highlights the importance of further investigation to gain a better understanding of the prevalence and implications of multiple sarcomas in a single individual [3]. Our findings provide valuable insights into the unique characteristics and complexities of hybrid tumors, as well as the need for further investigation into their behavior and management. LGFMS was first described by Dr. Evans in 1987 [7]. LGFMS is a rare tumor that affects young individuals, appearing equally in men and women. It is characterized by a slow-growing, well-circumscribed mass in the deep soft tissues, presenting as a painless lump or nodule. LGFMS is challenging to diagnose, as it resembles a benign fibroblastic lesion on histological examination. However, its tendency to recur and metastasize confirms its malignant nature [8]. SEF is a rare and distinctive variant of fibrosarcoma that typically manifests in adults. Its existence was first described in 1995 and has since been confirmed in various studies [9]. The hallmark histological characteristics of SEF include nests and cords of uniform, small epithelioid cells embedded in a dense sclerotic matrix. Ultrastructural examinations have established its fibroblastic nature, which is characterized by a dense collagenous matrix that is indistinguishable from osteoids and showed spindle-shaped areas ranging from benign fibroma-like to malignant fibrosarcoma-like zones, cysts, and calcification that may be evident in SEF; these tended to be minimal. Recent research has focused on the morphological, immunohistochemical, and molecular similarities between SEF and LGFMS, leading to the conclusion that these tumors are closely related. However, recent studies have shown that SEF is genetically distinct from LGFMS, with the predominant presence of EWSR1::CREB3L1 fusion and complex secondary genomic alterations [10]. Concurrent occurrences of LGFMS and SEF in the same tumor, known as hybrid tumors, are rare, with only a few cases reported in the literature [11]. LGFMS and SEFs demonstrated histological dissimilarities and are typically confined, although they commonly infiltrate surrounding tissues microscopically. These tumors display spindle cells that grow in brief fascicular or whorled patterns intertwined with fibrous stroma and an abundance of extracellular myxoid matrix. They generally exhibit low-to-moderate cellularity, scarce-to-no mitotic figures, and occasional nuclear pleomorphism. Calcification and fat deposits were typically absent [7, 12]. On the other hand, SEFs are similarly contained but can be distinguished histologically by uniform spherical to ovoid epithelioid cells arranged in nests and cords within a background of prominent hyaline sclerosis. These tumors may have calcifications and areas of myxoid material with cyst formation. Mitotic figures and necrosis are infrequent [9, 10]. In our case, LGFMS and SEF occurred in equal proportions. Both tumor types show increased MUC4 expression, making it a crucial marker for distinguishing LGFMS from other spindle cell neoplasms and SEF from other neoplasms with epithelioid morphology. LGFMSs commonly exhibit FUS:: CREB3L1 or FUS::CREB3L2 fusions [8, 11], whereas pure SEF tumors tend to have EWSR1 gene rearrangements [13]. Similar to pure LGFMS-SEFs, FUS translocations are commonly observed in hybrid LGFMSs [11]. However, rare cases of EWSR1 rearrangements have been reported in hybrid LGFMS-SEFs [14]. Our patient showed strong and widespread MUC4 staining. In the present case, the patient had a hybrid tumor of LGFMS and SEF in the thigh, and a second tumor (hibernoma) in the posterior aspect of the same thigh. Hibernomas are rare benign tumors originating from brown fat cells. It is a small, lobulated, and non-tender lesion most often found in the interscapular area of the back, followed by the neck, axillae, thigh, and intrathoracic area. Tumors usually cause tenderness and compression of surrounding structures as they grow. It is essential to consider hibernoma in the differential diagnosis due to its similarities, both clinically and radiographically, to malignant tumors. Distinguishing between the two can be difficult, highlighting the importance of proper diagnosis and management.
We presented a rare case of a patient with different tumors: A hybrid tumor composed of LGFMS and SEF and a second tumor, which was a hibernoma, highlighting the importance of interdisciplinary collaboration for the management of rare and complex soft-tissue tumors. The diagnosis of a hybrid tumor requires a high index of suspicion based on histology, aided by immunohistochemistry. Surgical resection remains the mainstay treatment. Long-term surveillance is crucial to monitor recurrence and metastasis.
This case report highlights the rare coexistence of a hybrid tumor and hibernoma in the same thigh, emphasizing the importance of accurate diagnosis and individualized strategies for such a complex tumor presentation.
References
- 1.Sbaraglia M, Bellan E, Dei Tos AP. The 2020 WHO classification of soft tissue tumours: News and perspectives. Pathologica 2021;113:70-84. [Google Scholar]
- 2.Furlong MA, Fanburg-Smith JC, Miettinen M. The morphologic spectrum of hibernoma: A clinicopathologic study of 170 cases. Am J Surg Pathol 2001;25:809-14. [Google Scholar]
- 3.Lex JR, Aoude A, Stevenson JD, Wunder JS, Evans S, Ferguson PC, et al. Multiple soft tissue sarcomas in a single patient: an international multicentre review. Sarcoma 2018;2018:5392785. [Google Scholar]
- 4.Schiffman R. Epithelioid sarcoma and synovial sarcoma in the same knee. Cancer 1980;45:158-66. [Google Scholar]
- 5.Isaza LF, Garner HW, Edgar MA, Attia S, Wilke BK. A case report of 2 distinct primary sarcomas arising in an extremity in rapid succession. Radiol Case Rep 2023;18:70-4. [Google Scholar]
- 6.Kramer SP, Bowman CJ, Wang ZJ, Sheahon KM, Nakakura EK, Cho SJ, et al. Hybrid low-grade fibromyxoid sarcoma and sclerosing epithelioid fibrosarcoma of the pancreas. J Gastrointest Canc 2020;51:1025-9. [Google Scholar]
- 7.Evans HL. Low-grade fibromyxoid sarcoma. A report of two metastasizing neoplasms having a deceptively benign appearance. Am J Clin Pathol 1987;88:615-9. [Google Scholar]
- 8.Matsuyama A, Hisaoka M, Shimajiri S, Hayashi T, Imamura T, Ishida T, et al. Molecular detection of FUS-CREB3L2 fusion transcripts in low- grade fibromyxoid sarcoma using formalin-fixed, paraffin-embedded tissue specimens. Am J Surg Pathol 2006;30:1077-84. [Google Scholar]
- 9.Meis-Kindblom JM, Kindblom LG, Enzinger FM. Sclerosing epithelioid fibrosarcoma. A variant of fibrosarcoma simulating carcinoma. Am J Surg Pathol 1995;19:979-93. [Google Scholar]
- 10.Warmke LM, Meis JM. Sclerosing epithelioid fibrosarcoma: A distinct sarcoma with aggressive features. Am J Surg Pathol 2021;45:317-28. [Google Scholar]
- 11.Prieto-Granada C, Zhang L, Chen HW, Sung YS, Agaram NP, Jungbluth AA, et al. A genetic dichotomy between pure sclerosing epithelioid fibrosarcoma (SEF) and hybrid SEF/low-grade fibromyxoid sarcoma: A pathologic and molecular study of 18 cases. Genes Chromosomes Cancer 2015;54:28-38. [Google Scholar]
- 12.Folpe AL. Low-grade fibromyxoid sarcoma: A review and update. Pathol Case Rev 2002;7:139-45. [Google Scholar]
- 13.Rekhi B, Folpe AL, Deshmukh M, Jambhekar NA. Sclerosing epithelioid fibrosarcoma - a report of two cases with cytogenetic analysis of FUS gene rearrangement by FISH technique. Pathol Oncol Res 2011;17:145-8. [Google Scholar]
- 14.Mok Y, Pang YH, Sanjeev JS, Kuick CH, Chang KT. Primary renal hybrid low-grade fibromyxoid sarcoma- sclerosing epithelioid fibrosarcoma: An unusual pediatric case with EWSR1-CREB3L1 fusion. Pediatr Dev Pathol 2018;21:574-9. [Google Scholar]