Holographic technology facilitates dynamic, three-dimensional visualizations of human anatomy, significantly enhancing surgical precision and providing surgeons with an interactive, immersive view of complex anatomical structures. This advancement represents a substantial shift from traditional 2D imaging techniques to a more sophisticated, interactive 3D approach.
Dr. Madhan Jeyaraman, Department of Orthopaedics, ACS Medical College and Hospital, Dr MGR Educational and Research Institute, Chennai, Tamil Nadu, India. E-mail: madhanjeyaraman@gmail.com
Orthopedic surgery, traditionally reliant on 2D imaging tools such as X-rays and magnetic resonance imagings (MRIs), is undergoing a revolutionary change with the introduction of holographic technology. Initially, a concept from science fiction used in entertainment and data representation, holography now offers groundbreaking applications in medicine, especially in orthopedics. Conceived by Dennis Gabor in 1948, holographic imaging has evolved significantly, providing real-time, three-dimensional visualizations of human anatomy, thereby aiding surgeons in complex procedures [1]. This technology enhances surgical precision through high-resolution, interactive representations of patient-specific anatomical structures, leading to more accurate planning and less invasive surgeries, crucial for better patient outcomes [2, 3]. This integration signifies a paradigm shift in surgical practices, equipping surgeons to visualize bones, joints, and tissues in unprecedented detail and immersion, similar to moving from radiographs to 3D computed tomography (CT) scans but with the added benefits of interactivity and real-time manipulation. However, challenges exist, including the cost of technology, the learning curve for professionals, extensive training requirements, and maintaining patient safety and medical standards in stringent regulatory environments [4]. This editorial provides an overview of the transformative potential of holographic technology in orthopedic surgery, discussing its historical evolution, current applications, challenges, and prospects, emphasizing the need for cautious optimism and sustainable integration to enhance patient care and surgical outcomes.
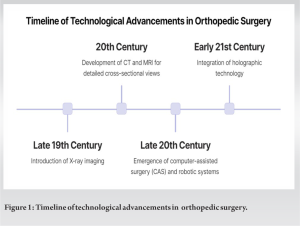
The evolution of orthopedic surgery is profoundly influenced by technological advancements. The timeline of technological advancements in orthopedic surgery is depicted in Figure 1. Initially reliant on manual skills and basic tools, the field was revolutionized in the late 19th century with the advent of X-ray imaging, allowing non-invasive bone and joint visualization [5]. The 20th century saw further advancements with the introduction of CT and MRI, providing detailed cross-sectional views of the musculoskeletal system, thereby enhancing diagnostic accuracy and pre-operative planning [3, 6]. A major transition occurred with the shift from conventional radiography to CT and MRI, offering more intricate musculoskeletal anatomy representations and moving toward a technology-assisted surgical approach [2]. The late 20th and early 21st centuries introduced computer-assisted surgery and robotic systems, significantly increasing precision, reducing human error, and promoting minimally invasive techniques, leading to shorter recovery times and fewer post-operative complications [3]. The latest innovation is the integration of holographic technology in orthopedics. Initially developed in other industries, holography provides a dynamic, three-dimensional anatomical view, enhancing surgical precision and immersion [4, 7]. This transition from basic imaging to advanced holography illustrates the continuous pursuit of innovation in orthopedics, aiming for greater precision, reduced invasiveness, and enhanced patient safety.
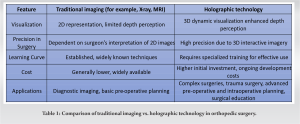
Holographic technology in medicine, particularly in orthopedic surgery, represents a notable advancement in surgeons’ ability to visualize and interact with patient anatomy. This technology, based on holography, produces dynamic three-dimensional images by recording and reconstructing light waves. In orthopedics, it provides an intuitive, immersive view of complex anatomical structures, surpassing traditional 2D imaging capabilities [7, 8]. Recent developments have significantly improved image clarity, user interfaces, and integration with real-time surgical navigation systems. These advancements enhance the resolution and interaction with holographic representations and facilitate their incorporation into surgical workflows, transitioning the technology from experimental to clinical use. This progress aids in pre-surgical planning and intraoperative guidance, leading to more precise, minimally invasive procedures, potentially improving outcomes and reducing recovery times [3, 6]. In orthopedic surgery, holographic technology is especially beneficial in complex cases requiring precision. It offers surgeons detailed 3D views of patient anatomy, aiding in accurate planning and execution of procedures. This enhanced visualization and spatial awareness are crucial for understanding tissue relationships, crucial for precise surgical planning and execution [1, 9, 10]. However, challenges remain, including ensuring the accuracy and reliability of holographic representations, integrating these systems into existing workflows, and overcoming cost and accessibility barriers [8]. Holographic technology holds transformative potential in orthopedic surgery. As it continues to evolve, its applications are expected to expand, enhancing surgical precision and patient outcomes. The technology goes beyond visualization to a comprehensive understanding of complex anatomy, essential in intricate surgical procedures [2, 3, 4, 5]. The comparison of traditional imaging vs. holographic technology in orthopedic surgery is tabulated in Table 1.
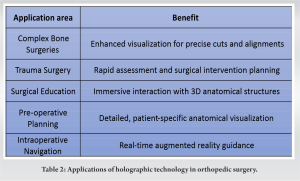
The integration of holographic technology in orthopedic surgery has significantly advanced the field, notably in complex bone surgeries, trauma surgery, surgical education, training, and preoperative and intraoperative planning as depicted in Table 2. In complex bone surgeries, particularly in spinal and joint replacement procedures, 3D holographic representations enable surgeons to visualize bone structures in high detail. This aids in making precise cuts and alignments, which are critical for the success of these intricate surgeries [6]. For trauma surgery, holography is instrumental in rapidly assessing injuries, allowing for the planning and simulation of surgical interventions. This pre-emptive strategy helps minimize complications during and after surgery, enhancing decision-making and surgical precision [1]. Holographic technology has transformed surgical education and training by providing an immersive experience in interacting with complex anatomical structures in three dimensions. This is crucial in orthopedics for understanding the spatial relationships of bones, muscles, and ligaments, essential for successful surgical outcomes [7]. Pre-operative planning has been revolutionized through holographic displays, offering a three-dimensional visualization of a patient’s anatomy, leading to more accurate and personalized surgical plans. This innovation improves understanding of anatomical complexities and relationships, thereby enhancing surgical precision [8].
Similarly, intraoperative navigation benefits from holography, providing surgeons with a real-time, augmented-reality view of the surgical site. This improves accuracy in procedures such as bone cuts or implant placements [3]. Holography also plays a role in the post-operative phase and patient education. It helps in elucidating surgical procedures to patients, increasing their understanding and involvement in their care. In addition, it aids in monitoring and rehabilitation through detailed visualizations of the healing process [9]. In joint replacement surgeries, holographic imaging is crucial for the precise alignment of implants, offering a level of precision beyond traditional methods, thus reducing post-operative complications and enhancing patient outcomes [5]. In spinal surgery, it assists in accurately placing screws and hardware, safely navigating complex spinal structures [2]. Furthermore, in complex fracture repairs, holographic imagery overlays the patient’s anatomy, aiding in visualizing fractures and planning repairs more effectively [3]. These applications highlight the potential of holographic technology to revolutionize orthopedic surgery, improving precision, outcomes, and streamlining surgical processes.
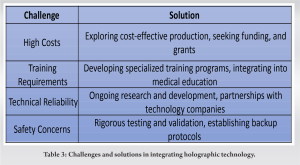
The integration of holographic technology into orthopedic surgery presents several multifaceted challenges. Economically, the high costs of implementation and maintenance are significant barriers, especially in resource-limited health-care settings. Hospitals must carefully weigh the cost-benefit ratio, considering the financial implications for the health-care system [3, 7, 8]. There is a steep learning curve associated with this technology. Surgeons and medical staff require specialized training to effectively utilize holographic systems in their practice, adding complexity and necessitating additional resources in the already demanding field of orthopedic surgery education [3, 4, 6]. Technical challenges are also notable. Ensuring the accuracy and reliability of holographic images for surgical precision is critical, yet maintaining consistency and real-time responsiveness of these systems is challenging. Integration with existing surgical workflows and tools is essential for maintaining safety and efficiency standards [2, 9].
Safety concerns extend to the technical reliability of holographic systems. Ensuring that these systems are fail-safe and have adequate backup protocols is crucial to prevent adverse outcomes during surgeries. In addition, potential interactions with other medical equipment necessitate rigorous testing and validation for patient safety [1]. Regulatory and ethical considerations are also key in integrating holographic technology. This involves navigating complex approval processes, ensuring compliance with health-care standards, and addressing patient privacy and data security issues. These considerations underscore the need for robust policy frameworks to manage the ethical implications and potential technological disparities across different health-care systems [5, 8]. The potential of holographic technology in enhancing surgical precision and patient care in orthopedic surgery is significant, but its integration faces economic, technical, educational, safety, regulatory, and ethical challenges. Addressing these challenges comprehensively is vital for the successful adoption of this technology in clinical practice. The challenges and solutions in integrating holographic technology are tabulated in Table 3.
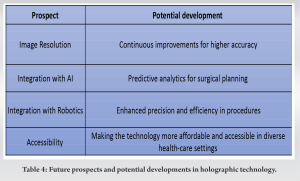
The advancement of holographic technology in orthopedic surgery is a rapidly evolving field. Central to this progress is the improvement in image resolution and accuracy, driven by computational and algorithmic advancements, essential for precise surgical execution [6]. This technology is increasingly being integrated with robotic surgery and artificial intelligence, creating advanced surgical platforms that promise greater precision and efficiency in orthopedic procedures [1]. The technology’s growing accessibility and cost-effectiveness suggest broader adoption in diverse health-care settings, even in regions with limited medical facilities [7]. Collaboration among technologists, surgeons, and educators is crucial for optimizing the use of holographic technology in orthopedics, ensuring it meets evolving medical needs [6]. Future developments in imaging resolution and interactivity are expected to enhance anatomical accuracy, while artificial intelligence integration could revolutionize surgical planning with predictive analytics [8]. Addressing current limitations, such as affordability, ease of operation, and seamless integration into surgical workflows, are essential for its widespread use in orthopedic surgery [3]. Multidisciplinary collaboration is emphasized to ensure that technological advancements align with the practical needs of orthopedic surgery [9]. Holographic technology’s evolution in orthopedic surgery holds immense potential for revolutionizing the field, enhancing surgical precision and patient outcomes. Overcoming challenges and fostering innovations are key to its successful integration into orthopedic practices [2, 3, 5]. The future of this technology, shaped by multidisciplinary insights, is set to redefine orthopedic surgery, making it more efficient, precise, and patient-centered as tabulated in Table 4 [4].
The integration of holographic technology into orthopedic surgery marks a significant leap forward in medical science and patient care. This technology transcends traditional imaging techniques, providing surgeons with dynamic, three-dimensional representations of anatomical structures, thus enhancing surgical precision and patient outcomes. While its potential is immense, challenges such as cost, training, technical reliability, safety concerns, and regulatory considerations must be addressed to fully harness its benefits. The future of orthopedic surgery, enriched by holographic technology, promises a shift toward more accurate, minimally invasive procedures, heralding a new era of medical innovation and patient care.
Holographic technology is revolutionizing orthopedic surgery by providing precise anatomical representations, improving outcomes, and reducing invasiveness.
Challenges include high costs and specialized training, with future directions focusing on affordability and integration with AI and robotics.
Successful adoption relies on multidisciplinary collaboration among technologists, surgeons, and educators for patient-centered surgical practices.
References
- 1.Haleem A, Javaid M, Vaishya R. Holography applications for orthopaedics. Indian J Radiol Imaging 2019;29:477-9. [Google Scholar]
- 2.Meulstee JW, Nijsink J, Schreurs R, Verhamme LM, Xi T, Delye HH, et al. Toward holographic-guided surgery. Surg Innov 2019;26:86-94. [Google Scholar]
- 3.Wong KC, Sun YE, Kumta SM. Review and future/potential application of mixed reality technology in orthopaedic oncology. Orthop Res Rev 2022;14:169-86. [Google Scholar]
- 4.Gupta A, Ambade R. From diagnosis to therapy: The role of virtual and augmented reality in orthopaedic trauma surgery. Cureus 2022;14:e29099. [Google Scholar]
- 5.Yinglong Z, Junsong W, Zhen B, Yanan W, Wei W. The application of holographic navigation guidance technology in malignant bone tumor surgery. Intell Surg 2022;2:14-21. [Google Scholar]
- 6.Thivagar M. Hologram opens a new learning door for surgical residents- an academic view point. In: HMAM2. Switzerland: MDPI; 2023. p. 21. [Google Scholar]
- 7.Lu L, Wang H, Liu P, Liu R, Zhang J, Xie Y, et al. Applications of mixed reality technology in orthopaedics surgery: A pilot study. Front Bioeng Biotechnol 2022;10:740507. [Google Scholar]
- 8.Teatini A, Kumar RP, Elle OJ, Wiig O. Mixed reality as a novel tool for diagnostic and surgical navigation in orthopaedics. Int J Comput Assist Radiol Surg 2021;16:407-14. [Google Scholar]
- 9.El‐Hariri H, Pandey P, Hodgson AJ, Garbi R. Augmented reality visualisation for orthopaedic surgical guidance with pre‐ and intra‐operative multimodal image data fusion. Healthc Technol Lett 2018;5:189-93. [Google Scholar]
- 10.Jeyaraman M, Nallakumarasamy A, Jeyaraman N. Industry 5.0 in orthopaedics. Indian J Orthop 2022;56:1694-702. [Google Scholar]