The present case report highlights the benefits of using the simple and cost-effective technique of tension band wiring to achieve good reduction, fixation, and a good functional outcome while managing the gap non-union patella.
Dr. Vipin Sharma Prof and Head, Department of Orthopedics Surgery, Dr. Rajendra Prasad Government Medical College, Tanda, Himachal Pradesh, India. E-mail: drvikramadityarai@gmail.com
Introduction: Gap non-union patellas are challenging to treat for an orthopedic surgeon. We hereby report a case of a 22-year-old person with a 3 cm gap nonunion, its surgical management, functional outcome, and implications for clinical practice.
Case Report: A 22-year-old active male presented to us with a background of comminuted fracture patella left side that he suffered 1 year ago, following which he was treated by open reduction and internal fixation (ORIF) with Tension Band Wiring (TBW). One year post-surgery, the patient had another fall, following which he had pain swelling in his left knee and difficulty in his knee extension. The patient presented 6 months later with painful ambulation and a swelling left knee. A 3 cm gap nonunion along with underlying implants could be palpated. The patient underwent surgery in the form of previous implant removal, freshening and apposition of fracture ends, and single-staged reconstruction of the extensor mechanism using TBW. The patient had full range of motion at the 1-year follow-up.
Conclusion: The present case highlights the fact that small-gap non-union patella can be managed simply as a single-stage procedure with ORIF and TBW.
Keywords: Fracture patella, non-union, tension band wiring
Fracture patella rarely progresses into non-union as patella is a sesamoid bone and is managed mostly with early surgical intervention. The management of non-union patellas is still a challenge in orthopedic practice. The incidence of non-union patella as quoted in the literature is 2.7–12.5% [1]. The quadriceps muscle attached at the proximal end pulls the proximal fragment more proximally, resulting in a gap at the fracture site. This leads to failure of the quadriceps mechanism, which causes patients to seek treatment for patellar non-union. Various modalities of treatment of nonunion patella are available, e.g., apposition of fracture fragments and fixation with TBW Traction of the proximal fragment followed by definitive surgery-a two stage procedure, Quadricepsplasty followed by surgery – a single-stage procedure, Gradual docking using the Ilizarov apparatus– is a single-stage procedure and rarely a partial or total patellectomy. In the present case, a 3 cm gap non-union left patella was managed by open reduction and internal fixation (ORIF) with tension band wiring (TBW).
A 22-year-old active male presented to us with a background of comminuted fracture patella left side that he suffered 1 year ago, following which he had been treated by ORIF with TBW. The patient was ambulatory 2 months after this surgery and had achieved full range of motion in the knee by 8 months post-operative. One year after index surgery, he suffered another fall from the stairs, following which the patient had pain swelling in his left knee with difficulty in his knee extension. The patient continued to remain ambulatory, albeit with difficulty. He presented to us 6 months later with painful ambulation and a swelling left knee. On palpation of the knee anteriorly, a 3 cm gap along with underlying implants could be palpated. Inability to perform a straight leg raising test with an extensor lag of 45° was noted, indicating loss of function of the extensor mechanism, although active knee flexion up to 90° was evident. A plain radiograph of the left knee demonstrated a gap of 3 cm (Fig. 1 and 2). Implant removal, freshening, and apposition of fracture ends and single-stage reconstruction of the extensor mechanism using TBW were done (Fig. 2).
The release of the extensor mechanism was not required, as the apposition of non-union fragments was achieved with gentle traction on the proximal patella non-union fragment in a distal direction. Patient had full ROM at 1 year follow-up with a Knee Society score of 98 (Fig. 3-7).
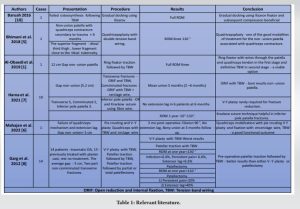
Management of gap non-unions of patella is a challenge to treat. Non-compliant patients, delayed patient care, previously failed surgery, geographical inaccessibility, and financial constraints are the various reasons why this rare condition is still commonly seen [2]. Non-operative management in the form of observation, activity modification, physical therapy, and local pain-relieving measures has been advocated in a select group of patients with low functional demand [3], but a torn extensor retinaculum or quadriceps contracture leading to a high-riding proximal patellar fragment makes surgical management mandatory [4]. Moreover, an intact extensor mechanism is a lever for knee extension; hence, its integrity is desirable in high-functional-demand patients. The aim of treatment for Gap Non-union Patella is to bring proximal and distal fragments together to achieve osteosynthesis. If there is associated quadriceps contracture, then a single-stage procedure like V-Y plasty [5], pie crusting of quadriceps [6], followed by TBW [7], and Ilizarov ring fixator are done. Otherwise, a two-stage procedure like pre-operative skeletal traction [1] to bring the proximal fragment to the desired level, followed by approximation, of fracture fragments and internal fixation at a later date, is also possible (Table 1).
The literature is ambiguous regarding the best option to bring the high-riding proximal patellar to a normal level for apposition with the distal fragment. Some studies have reported good results with quadricepsplasty [5], while others have preferred skeletal traction to proximal fragment patella over quadricepsplasty, as quadricepsplasty may lead to extensor lag and quadriceps contracture [8]. Mahajan et al. [6] have mentioned pie crusting of quadriceps or V-Y plasty followed by fixation with encerclage wire or TBW gives a good functional outcome in gap non-union patella, while other studies have advocated pre-operative patellar traction followed by TBW as a better alternative to either V-Y plasty or patellectomy [8]. Once the proximal and distal fragments of the patella are in apposition, TBW is a cheap and effective way to achieve osteosynthesis. Another treatment modality, i.e., patellectomy, as a treatment option for gap non-union patella has also been mentioned [9]. TBW and patellectomy have been compared in a study for gap non-union of the patella. Out of twenty-two patients with neglected fractures of the patella, TBW was done in 16 cases, TBW with cerclage in three cases, and patellectomy in three cases [9]. Patellectomy procedures are best avoided as the efficiency of the extensor mechanism is reduced by 30% in patellectomy patients [9], leading to extension lag and poor functional outcomes [5]. Moreover, the length of the lever arm of the external apparatus mechanism is also compromised, causing excessive stress on the knee joint during extension, leading to subsequent degeneration of the knee joint [5]. Two-ring ilizarov has emerged as a popular single-stage procedure that does not require quadricepsplasty but works on the principal of a gradual quadriceps stretch and subsequent docking of patellar fragments. Definitive fixation is achieved with these devices after the gradual docking of fracture fragments [10]. Above is a brief review of the many approaches mentioned in the literature to address the gap non-union of the patella. While the present patient had a gap non-union of 3 cm, no proximal fragment traction or quadricepsplasty was required. The patient was managed by apposition of fracture fragments and TBW.
The simple technique of single-staged TBW with extensor mechanism repair for the management of non-union patella fractures is a simple and cost-effective way of restoring the extensor mechanism in a select group of patients. Our case shows that a good functional outcome is achievable without the need for a V-Y quadricepsplasty or a patellectomy, provided there is no quadriceps contracture.
Treatment of Gap non-union patella remains a challenge in orthopedic practice. The present case will help orthopedic surgeons consider TBW, a simple and cost-effective technique, as a viable treatment option for these injuries.
References
- 1.Al-Obaedi O, Thakrar RR, Kundra R, Iqbal MJ. Gap non-union patella fractures: Case report and review of the literature. J Orthop Case Rep 2019;9:69-71. [Google Scholar]
- 2.Singhal V, Mittal D, Lal H, Khare R, Sharma S. Gap non-union patella: A treatment dilemma Pb. J Orthop 2010;12:8-11. [Google Scholar]
- 3.Nathan ST, Fisher BE, Roberts CS, Giannoudis PV. The management of nonunion and delayed union of patella fractures: A systematic review of the literature. Int Orthop 2011;35:791-5. [Google Scholar]
- 4.Carpenter JE, Kasman RA, Patel N, Lee ML, Goldstein SA. Biomechanical evaluation of current patella fracture fixation techniques. J Orthop Trauma 1997;11:351-6. [Google Scholar]
- 5.Bhimani R, Singh P, Bhimani F. Double-tension wire management of nonunion patella with severe quadriceps contracture. Case Rep Orthop 2018;6:1364129. [Google Scholar]
- 6.Mahajan NP, Kondewar P, Ghoti S, Chaudhari K, Gund A. Management of a gap non-union patella fracture using encirclage wire and tension band wiring with Quadriceps V-Y Plasty in an elderly patient: A rare case report and review of literature. J Orthop Case Rep 2022;12:95-8. [Google Scholar]
- 7.Harna B, Gupta P, Singh J, Rousa S, Gupta A. Surgical management of non-union patella fracture: A case series and review of the literature. Arch Bone Jt Surg 2021;9:554-8. [Google Scholar]
- 8.Garg P, Sahoo S, Satyakam K, Biswas D, Garg A, Mitra S, et al. Patellar nonunions: Comparison of various surgical methods of treatment. Indian J Orthop 2012;46:304-11. [Google Scholar]
- 9.Uvaraj NR, Mayil Vahanan N, Sivaseelam A, Mohd Sameer M, Basha IM. Surgical management of neglected fractures of the patella. Injury 2007;38:979-83. [Google Scholar]
- 10.Baruah RK. Modified ilizarov in difficult fracture of the patella. A case report. J Orthop Case Rep 2016;6:26-8. [Google Scholar]