Arthroscopic repair of Anterior Cruciate Ligament reconstruction using bioabsorbable material.
Dr. T N Santhosh Kumar, Department of Orthopaedics Employee’s State Insurance Corporation MC, PGIMSR and Model Hospital, Bengaluru - 560 010, Karnataka, India. E-mail: tumakuru572102@gmail.com
Introduction: Arthroscopic anterior cruciate ligament (ACL) reconstruction is a very commonly done procedure in recent times. There is a need for a long-term outcome study of ACL reconstruction with a comparison between different types of fixation techniques. The graft fixation methods vary from aperture fixation (interference screws) to suspensory fixation methods (endobutton). Failure of graft incorporation and the development of tunnel widening (TW) after ACL reconstruction have been frequently reported in the long term in present literature. TW especially complicates revision ACL surgery. This is a prospective non-randomized clinical study of arthroscopic ACL reconstruction comparing the functional results between aperture fixation and suspensory fixation.
Materials and Methods: Two groups of 14 patients who underwent autogenous hamstring ACL reconstruction with a minimum of 2-year follow-up evaluation were included in the study. The first group underwent aperture fixation with bioabsorbable interference screw at tibial and femoral side. The second group underwent suspensory fixation with endobutton fixation on the femoral side and biointerference screw on the tibial side. Both group patients were examined clinically before surgery, and at 3 months, 6 months, 1 year, and at 2 years. They were compared for functional outcome with Tegner Lysholm knee score.
Observation and Results: There was a significant improvement in functional outcome in both the groups for base and at 3 months, also for 3 months and 6 months but for 6 months–1 year. Group 2 is almost significant. This improvement in outcome in Group 2 is consistent from 1 year to 2 years.
Conclusion: In our prospective study comparing the outcomes of functional outcomes of ACL reconstruction with aperture fixation versus suspensory fixation on the femur, which was evaluated using Tegner Lysholm knee score over a period of 2 years, suspensory fixation was found to be better. However, further studies involving a larger series of cases are required for a better evaluation of the outcome.
Keywords: Bioabsorbable material, anterior cruciate ligament, Tegner Lysholm knee score.
The importance of the anterior cruciate ligament (ACL) in knee function has been emphasized for not only athletes but also in young and middle-aged individuals who do not participate in sports. Arthroscopic ACL reconstruction is a very commonly done procedure in recent times [1]. The previous studies have shown that a hamstring graft is equivalent or superior to a bone-patellar tendon-bone (BPTB) autograft [2-5]. However, most orthopedic surgeons prefer using hamstring grafts. The two most widely used methods of fixation of hamstring graft include aperture fixation and suspensory fixation. ACL graft fixation has been proposed to exert an essential influence on the mechanical behavior of the graft, although the biomechanics of the final construct will be determined by multiple factors [6]. Femoral fixation of the quadrupled hamstring graft is the key element to a durable ACL reconstruction [6]. There are many options available to achieve it [6]. With interference screw fixation, the graft is compressed against the tunnel wall, allowing for fixation close to the joint [7]. However, endobutton fixation is away from the joint. Cortical button fixation allows for greater movement of the graft within the bone tunnel [8, 9]. The objective of this study was to compare the functional outcome after the bioabsorbable screw and suspensory fixation method on the femur and bioabsorbable screw on the tibial end in ACL reconstructions done using hamstring autograft in the middle socioeconomic, semiskilled population of south India.
Comparison of functional assessment of ACL reconstruction in two different femoral fixation methods using interference screw and endobutton versus hamstring autograft using Tegner Lysholm scoring system.
Twenty-eight patients were admitted at ESIC Medical College and Model Hospital, Bangalore, between 2016 and 2019 in a prospective, non-randomized comparative study. A continuous series of patients were operated for full-thickness ACL tear. In all the cases, hamstring graft was used for ACL reconstruction. The technique of reconstruction differed at the femoral side, that is, bioabsorbable interference screw fixation and endobutton fixation. All the patients were fixed with a bioabsorbable interference screw on the tibial side. The patients were operated by the same surgical team and the implants used in the case study were of the same company.
Inclusion criteria
The following criteria were included in the study:
- Patients diagnosed to have complete ACL tear clinically and radiologically
- Age group 15–55 years
- Examined by a single surgeon
- ACL deficient knee confirmed radiologically by Magnetic resonance imaging (MRI)
- Associated menisci injuries
- Patients with significant symptoms of pain/instability
- Normal contralateral
Exclusion criteria
The following criteria were excluded from the study:
- Observed chondral lesions that could modify the post-operative rehabilitation protocol
- Collaterals and/or PCL injuries
- Chronic ACL insufficiency with osteoarthritis
- Bilateral knee injuries
- Associated tibial plateau fractures
- Previously operated
All the patients were assessed in the outpatient department for a history of instability in the form of the sense of knee giving away, difficulty in climbing down the stairs, and were evaluated for clinical signs such as positive Lachman’s test and anterior drawer test. The tear was confirmed radiologically using MRI. (Fig. 1-6) The patients who had a full-thickness ACL deficiency were considered for surgery. After detailed evaluation, a datasheet containing the mechanism of injuries and clinical and radiological examination (fig 8) findings with pre-operative Tegner Lysholm score was completed.
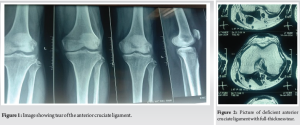
Detailed informed consent was taken from each patient, explaining the nature of the procedure and the complications associated with it. The operating limb was prepared preoperatively. All the patients were examined under spinal anesthesia. A positive Lachman’s test with soft end point and pivot shift test with glide or clunk was present in all patients. Initially, all the cases underwent diagnostic arthroscopy through the standard anterolateral portal and the ACL tear was confirmed under vision. Patients in Group 1-first fourteen patients received bioabsorbable interference screws both proximally and distally. Patients in Group 2-second fourteen received suspensory fixation (Endobutton) proximally and bioabsorbable screw distally. After visual confirmation of the deficient ACL, arthroscopic reconstruction with hamstring tendon graft was done. The graft was quadrupled in all the cases and was fixed proximally by bioabsorbable screw or endobutton and distally by bioabsorbable screws.
All patients underwent the surgery under epidural anesthesia. Using anteromedial and anterolateral portals, diagnostic arthroscopy was done and the full-thickness ACL tear was confirmed. The hamstring tendon was harvested (Fig 7) through a 4 cm long longitudinal incision, 3 cm distal to the joint line, and 2 cm medial to tibial tuberosity. Both the semitendinosus and gracilis were harvested from the ipsilateral side, prepared, and quadrupled on the graft board with whip stitch using No.2 Ethibond sutures. All were two portal technique single bundle ACL reconstruction with quadruple hamstring graft harvested from the same side. In the first 11 patients, fixation was achieved by both proximally and distally by bioabsorbable screws. In the second 11 patients, fixation was done proximally by endo button and distally by bioabsorbable interference screws. The femoral tunnel was made through the transportal technique. The tibial tunnel was done by an elbow aimer. The tibial side was fixed by bioabsorbable screws in all patients. Fig. 9.
Postoperatively, patients were immobilized with knee in full extension with a long knee brace. On the second post-operative day quadriceps strengthening exercises, foot and knee exercises were started. All patients underwent standardized rehabilitation protocol. Partial weight bearing with a long knee brace was allowed for 10–14 days and full weight bearing by 2–3 weeks with a range of motion and half squat. Stair climbing, cycling, and jogging were allowed progressively and they were regularly followed up at 3, 6, and at 12th months. In addition to clinical evaluation by anterior drawer test and Lachman radiological evaluations and functional outcomes were assessed by Tegner Lysholm score at 3 months, 6 months, and 1 year follow-up. The Tegner Lysholm knee score was calculated for 1. Limp, 2. Support, 3. pain, 4. instability, 5. locking, 6. swelling, 7. stair climbing, and 8. squatting.
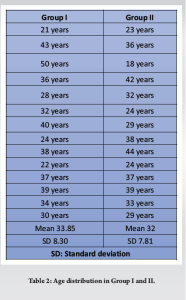
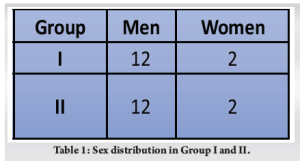
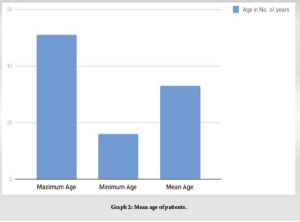
Of the 28 patients, there were 24 men (85.7%) and 4 women (14.3%) in the age group of 16–51. (Table 1). The mean age in group 1 was 33.85 and in the 2nd group was 32. (Table 2)
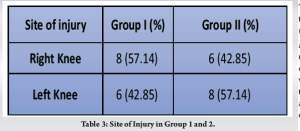
In group 1, 57.14% were right [10] and 42.85% were left knee [11] involved, whereas in group 2, 42.85% of right [11] knee was involved and in 57.14% of patients, it was left [10] knee (Table 3).
The mode of injury in the majority was twisting injury during activities 17 (60.17%)
and RTA 11 (39.83%). Most patients underwent surgery between 15 days and 60 days after surgery. There was one patient who presented later, almost 4 years after the injury. However, it did not have any adverse effect on his post-operative outcome.
There were some patients with additional injuries in both groups. Two had a medial meniscus tear and two had a lateral meniscus in Group 1. In Group 2, two had medial meniscus tear and one had lateral meniscus injury.
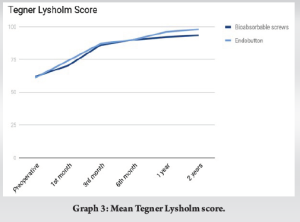
At follow-up Group 1 mean Tegner Lysholm knee scores at pre, 1, 3, 6, 12, and 24. Month follow-up were 62, 70.2, 86, 90, 92, and 93.42, respectively. Inpatients of Group 2, the mean Tegner Lysholm knee scores were 61, 74, 87, 90, 96, and 98, respectively.
Patients in both the groups had similar pre-operative comparable variables. Postoperatively( both the groups had significant improvement in the first 3 months, which progressed over successive follow-ups. Statistically, the functional outcomes as per Tegner Lysholm knee score were improved almost in a similar fashion for both groups. Although not statistically significant, the patients in Group 2 had better scores through each stage. (Graph 1-3).
ACL is an important structure to stabilize the knee joint. However, it is also the most vulnerable ligament in the knee joint and is most commonly involved in injuries. Twisting forces to the knee result in a tear in the ACL which causes knee joint instability. This not only affects the patient’s daily activities and sports but also causes further wear and tear of the joint. Therefore, to restore the structure and function of the knee joint, except for severe OA, all patients with ACL injury need surgical reconstruction [12]. ACL tear is commonly treated arthroscopically using a hamstring autograft or BPTB graft [13, 14]. Arthroscopic ACL reconstruction using central third BTB autograft and rigid fix femoral fixation gave good stability at 1–1.5-year follow-up. However, due to donor site morbidities such as patellar fracture, patellar tendon rupture, quadriceps weakness, and anterior knee pain assessment in patellar BPTB graft [15], the use of hamstring graft has become increasingly popular. Noyes et al. demonstrated that the stiffness of a hamstring graft is nearly equal to that of the ACL, while BPTB grafts are approximately 3.76 times stiffer than the ACL [13]. Thus, a four-strand hamstring graft appears to be stronger than comparable BPTB grafts and closer to linear stiffness of the ACL. Magnussen et al. [16], in 2010 found that a quadrupled hamstring tendon autograft was utilized in 44% of ACL reconstructions in the multicenter orthopedic outcomes network (MOON) cohort, which was more than patellar tendon auto grafts at 42% [17]. The Norwegian Knee Ligament Registry reported that a hamstring tendon autograft was used in 60% of ACL reconstructions [16, 17]. However, since then patellar tendon graft has given way in favor of hamstring tendon graft. There are mainly two types of fixation devices used in anterior cruciate ligament (ACLR) in bone tunnels: (a) Aperture fixation means the fixation of a graft at the opening of the bone tunnel like interference screws (intrafix) and (b) suspensory fixation of the graft that is remote from the intra-articular space. Aperture graft fixation device includes a screw, post, washer, etc., whereas suspensory fixation of graft is done using Endobutton (Smith and Nephew) or Transfix (Arthrex). These devices provide a secure fixation of the graft so that it can heal properly within the tunnel. Furthermore, the secure fixation enables early rehabilitation exercises and faster returns to pre-injury status of the patient, including early return to sports. The choice of fixation of the graft varies from aperture fixation techniques like interference screws to suspensory fixation techniques like cross pin fixation or endobutton. Most of these techniques show excellent results. Several techniques are in use, with success rates of between 65% and 90% [11]. The use of interference screws for graft fixation is considered to provide higher fixation strength as compared with other devices such as staples or buttons [10, 18]. Barber et al. compared 7 mm PLLA bio screws to metal interference screws and had femoral breakage in six patients out of 42 with no adverse functional outcomes [19]. The authors hypothesized that breakage occurred due to inexperience with the device and smaller diameter screws (7 mm). Subsequent to this series, the core diameter of the screw was increased and a larger screw (8 mm) was made available. Following this, the reported screw breakage has become practically nil in further studies [7, 20]. The choice of fixation devices for ACLR is mostly surgeon –dependent [21]. Theoretically, both techniques have their own advantages. Aperture fixation increases the stiffness of the knee, if the elastic modulus of the graft is assumed to be constant over its length [22, 23]. This is supposed to be due to mitigation of the “bungee cord” effect [24-28]. Aperture fixation theoretically also has an advantage in mitigation against the “windshield wiper” effect. The sagittal movement that occurs in the suspensory fixation theoretically allows for the widening of the tunnel [24-26,29]. Hakimi et al. [21] found that in the UK, the hamstring femoral fixation was done with a suspension device in 79% and interference screw in 18%. Of those using a suspension device, the Endobutton was most common (48%), followed by transfix (26%) and rigid fix (19%). Tibial fixation was most commonly achieved by interference screw (57%) followed by intrafix (30%). The endobutton is commonly used and is relatively inexpensive. The point of fixation lies some distance from the joint. There is a nylon material present between the graft and the button. This suspensory fixation has been associated with high failure load and tunnel widening due to graft-related micro motions into the bony tunnel and anterior joint laxity [30]. However, it has some theoretical advantages as well. In laboratory analysis, it has been shown that the tibial and femoral insertions of the ACL cover a substantial surface area, or “footprint” [28, 31-35] which may be reproduced to a greater extent using suspensory fixation. This results in a more anatomical footprint, resulting in better restoration of joint mechanics [36]. Browning et al. [5], in 2017 did a meta-analysis on the comparison between suspensory and aperture fixation using a quadrupled hamstring tendon graft. They concluded that final laxity as measured with the KT-1000 arthrometer was significantly better in the suspensory group and also that the rupture rate was lower. However, there were no other differences in the clinical outcomes between the two fixation methods. A similar study by Kim et al. concluded that the type of graft fixation device did not affect the clinical outcome and stability [37]. In Ganga Hospital open injury Severity score, the use of MESS score has a lower predictive value compared to GHOISS in deciding amputation versus salvage. A GHOISS of 17 or more has the highest sensitivity and specificity to predict amputation.[38] Along with ACL tear if patient had olecranon fracture in trauma, surgical fixation for Olecranon fractures will helps in early mobility of joints and anatomical fixation of the fractures.[39] In our study, we have used bio interference screw and endobutton as fixation methods in ACL reconstruction. Both modes are associated with improved function and satisfaction of patients as indicated by Tegner Lysholm score and anterior drawer test after surgery. Although the overall absolute score is better in Group 2, that is, endobutton fixation group, it is not statistically significant in the first 6 months. Considering the Tegner Lysholm score magnitudes of both the groups we feel the Group 2 endo button fixation is better clinically as compared Group 1 because the score is statistically similar for base and at 3 month sand for 3 months and 6 months between the groups. However, when we compare the scores at the end of 1 year, patients in Group 2 did significantly better (P = 0.0278). The same trend followed at the end of the 2 year follow-up, with patients in Group 2 having a better score which was statistically significant (P = 0.0185). The study has some limitations like a smaller sample size, consisting of 28 patients, and a relatively shorter duration of study of 2 years.
We did a prospective comparative study of the functional outcomes in patients after ACL reconstruction by hamstring graft which was fixed using aperture fixation with bio interference screws and suspensory fixation with endobutton at the femur. Both the groups were fixed using a bioabsorbable screw at the tibia. Functional assessment was done on the basis of Tegner Lysholm score at 1, 3, 6, 12, and 24 months. The group fixed using the endobutton fixation (group II) had better results at the end of 2 years in terms of instant stability of the graft and functional outcome. The study results were statistically significant. However, a larger population study for a longer period of follow-up is recommended. We continue the study to evaluate the longer-term outcome in these patients.
In our study, we have used bio interference screw and endobutton as fixation methods in ACL reconstruction. Both modes are associated with improved function and satisfaction of patients as indicated by Tegner Lysholm score and anterior drawer test after surgery. We compared the scores at the end of 1 year, patients in Group 2 did significantly better (P = 0.0278). The same trend followed at the end of the 2 year follow-up, with patients in Group 2 having a better score which was statistically significant (P = 0.0185). The study has some limitations of the study like a smaller sample size, consisting of 28 patients, and a relatively shorter duration of study of 2 years.
References
- 1.Hughes G, Watkins J. A risk-factor model for anterior cruciate ligament injury. Sports Med 2006;36:411-28. [Google Scholar]
- 2.Maletis GB, Cameron SL, Tengan JJ, Burchette RJ. A prospective randomized study of anterior cruciate ligament reconstruction: A comparison of patellar tendon and quadruple-strand semitendinosus/gracilis tendons fixed with bioabsorbable interference screws. Am J Sports Med 2007;35:384-94. [Google Scholar]
- 3.Schimoler PJ, Braun DT, Miller MC, Akhavan S. Quadrupled hamstring graft strength as a function of clinical sizing. Arthroscopy 2015;31:1091-6. [Google Scholar]
- 4.Wagner M, Kaab MJ, Schallock J, Haas NP, Weiler A. Hamstring tendon versus patellar tendon anterior cruciate ligament reconstruction using biodegradable interference fit fixation: A prospective matched-group analysis. Am J Sports Med 2005;33:1327-36. [Google Scholar]
- 5.Browning WM 3rd, Kluczynski MA, Curatolo C, Marzo JM. Suspensory versus aperture fixation of a quadrupled hamstring tendon autograft in anterior cruciate ligament reconstruction: A meta-analysis. Am J Sports Med 2017;45:2418-27. [Google Scholar]
- 6.Frank CB, Jackson DW. The science of reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am 1997;79:1556-76. [Google Scholar]
- 7.Mayr R, Smekal V, Koidl C, Coppola C, Eichinger M, Rudisch A, et al. ACL reconstruction with adjustable-length loop cortical button fixation results in less tibial tunnel widening compared with interference screw fixation. Knee Surg Sports Traumatol Arthrosc 2020;28:1036-44. [Google Scholar]
- 8.Fauno P, Kaalund S. Tunnel widening after hamstring anterior cruciate ligament reconstruction is influenced by the type of graft fixation used: A prospective randomized study. Arthroscopy 2005;21:1337-41. [Google Scholar]
- 9.Lee DH, Son DW, Seo YR, Lee IG. Comparison of femoral tunnel widening after anterior cruciate ligament reconstruction using cortical button fixation versus transfemoral cross-pin fixation: A systematic review and meta-analysis. Knee Surg Relat Res 2020;32:11. [Google Scholar]
- 10.Woo SL, Wu C, Dede O, Vercillo F, Noorani S. Biomechanics and anterior cruciate ligament reconstruction. J Orthop Surg Res 2006;1:2. [Google Scholar]
- 11.Emond CE, Woebler EB, Kurd SK, Ciccotti MG, Cohen SB. A comparison of the results of anterior cruciate ligament reconstruction using bioabsorbable versus metal interference screws: A meta-analysis. J Bone Joint Surg Am 2011;93:572-80. [Google Scholar]
- 12.Ding Y, Zhang Y, Jia H, Gu D, Chen L. [Mid-term effectiveness of arthroscopic anterior cruciate ligament reconstruction combined with meniscus allograft transplantation]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019 Sep 15;33(9):1071-1076. Chinese. doi: 10.7507/1002-1892.201904006. PMID: 31512445; PMCID: PMC8355850. [Google Scholar]
- 13.Noyes FR, Butler DL, Grood ES, Zernicke RF, Hefzy MS. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am 1984;66:344-52. [Google Scholar]
- 14.Eriksson K, Anderberg P, Hamberg P, Löfgren AC, Bredenberg M, Westman I, et al. A comparison of quadruple semitendinosus and patellar tendon grafts in reconstruction of the anterior cruciate ligament. J Bone J Surg Br 2001;83:348-54. [Google Scholar]
- 15.Kleipool AE, Van Loon T, Marti RK. Pain after use of the central third of the patellar tendon for cruciate ligament reconstruction. 33 patients followed 2-3 years. Acta Orthop Scan 1994;65:62-6. [Google Scholar]
- 16.Magnussen RA, Granan LP, Dunn WR, Amendola A, Andrish JT, Brophy R, et al. Cross-cultural comparison of patients undergoing ACL reconstruction in the United States and Norway. Knee Surg Sports Traumatol Arthrosc 2010;18:98-105. [Google Scholar]
- 17.Chen NC, Boykin RE, Millett PJ. Broken femoral cross pin after hamstring anterior cruciate ligament reconstruction: Case report. J Knee Surg 2007;20:245-8. [Google Scholar]
- 18.Kurosaka M, Yoshiya S, Andrishjt JT. A biomechanical comparison of different surgical techniques of graft fixation in anterior cruciate ligament reconstruction. Am J Sports Med 1987;15:225-9. [Google Scholar]
- 19.Barber FA, Elrod BF, McGuire DA, Paulos LE. Preliminary results of an absorbable interference screw. Arthroscopy 1995;11:537-48. [Google Scholar]
- 20.Ma CB, Francis K, Towers J, Irrgung J, Fu FH, Harner CH. Hamstring anterior cruciate ligament reconstruction: A comparison of bioabsorbable interference screw and endobutton-post fixation. Arthroscopy 2004;20:122-8. [Google Scholar]
- 21.Hakimi M, Anand S, Sahu A. ACL reconstruction-current UK practice. J Bone Joint Surg Br 2012,94B;42. [Google Scholar]
- 22.Morgan CD, Kalmam VR, Grawl DM. Isometry testing for anterior cruciate ligament reconstruction revisited. Arthroscopy 1995;11:647-59. [Google Scholar]
- 23.Scheffler SU, Südkamp NP, Göckenjan A, Hoffmann RF, Weiler A. Biomechanical comparison of hamstring and patellar tendon graft anterior cruciate ligament reconstruction techniques: The impact of fixation level and fixation method under cyclic loading. Arthroscopy 2002;18:304-15. [Google Scholar]
- 24.Hoher J, Livesay GA, Ma CB, Withrow JD, Fu FH, Woo SL. Hamstring graft motion in the femoral bone tunnel when using titanium button/polyester tape fixation. Knee Surg Sports Traumatol Arthrosc 1999;7:215-9. [Google Scholar]
- 25.Nebelung W, Becker R, Merkel M, Ropke M. Bone tunnel enlargement after anterior cruciate ligament reconstruction with semitendinosus tendon using endobutton fixation on the femoral side. Arthroscopy 1998;14:810-5. [Google Scholar]
- 26.Brand J Jr., Weiler A, Caborn DN, Brown CH Jr., Johnson DL. Graft fixation in cruciate ligament reconstruction. Am J Sports Med 2000;28:761-74. [Google Scholar]
- 27.Fu FH, Bennett CH, Ma CB, Menetrey J, Lattermann C. Current trends in anterior cruciate ligament reconstruction. Part II. Operative procedures and clinical correlations. Am J Sports Med 2000;28:124-30. [Google Scholar]
- 28.Lubowitz JH, Schwartzberg R, Smith P. Cortical suspensory button versus aperture interference screw fixation for knee anterior cruciate ligament soft-tissue allograft: A prospective, randomized controlled trial. Arthroscopy 2015;31:1733-9. [Google Scholar]
- 29.Wilson TC, Kantaras A, Atay A, Johnson DL. Tunnel enlargement after anterior cruciate ligament surgery. Am J Sports Med 2004;32:543-9. [Google Scholar]
- 30.Ishibashi Y, Rudy TW, Livesay GA, Stone JD, Fu FH, Woo SL. The effect of anterior cruciate ligament graft fixation site at the tibia on knee stability: Evaluation using a robotic testing system. Arthroscopy 1997;13:177-82. [Google Scholar]
- 31.Hwang MD, Piefer JW, Lubowitz JH. Anterior cruciate ligament tibial footprint anatomy: Systematic review of the 21st century literature. Arthroscopy 2012;28:728-34. [Google Scholar]
- 32.Lubowitz JH, Akhavan S, Waterman BR, Aalami-Harandi A, Konicek J. Technique for creating the anterior cruciate ligament femoral socket: Optimizing femoral footprint anatomic restoration using outside-in drilling. Arthroscopy 2013;29:522-8. [Google Scholar]
- 33.Piefer JW, Pflugner TR, Hwang MD, Lubowitz JH. Anterior cruciate ligament femoral footprint anatomy: Systematic review of the 21st century literature. Arthroscopy 2012;28:872-81. [Google Scholar]
- 34.Siebold R, Ellert T, Metz S, Metz J. Tibial insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: Morphometry, arthroscopic landmarks, and orientation model for bone tunnel placement. Arthroscopy 2008;24:154-61. [Google Scholar]
- 35.Siebold R, Ellert T, Metz S, Metz J. Femoral insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: Morphometry and arthroscopic orientation models for double-bundle bone tunnel placement--a cadaver study. Arthroscopy 2008;24:585-92. [Google Scholar]
- 36.Lubowitz JH, Poehling GG. Watch your footprint: Anatomic ACL reconstruction. Arthroscopy 2009;25:1059-60. [Google Scholar]
- 37.Kim HS, Seon JK, Jo AR. Current trends in anterior cruciate ligament reconstruction. Knee Surg Relat Res 2013;25:165-73. [Google Scholar]
- 38.Kumar, K. Naveen; Shivanna, Harish Y. S.; Kumar, T. N. Santhosh; Pratheeksh, . Assessment of Ganga Hospital Open Injury Severity Score of Limbs. Journal of Emergencies, Trauma, and Shock 13(4):p 317-318, Oct–Dec 2020. | DOI: 10.4103/JETS.JETS_68_20. [Google Scholar]
- 39.Shivanna AH, Shivanna HY, Narayanapp SKT, H G, Sriharsha B. Clinical Study of Surgical Management of Olecranon Fracture. J Orthop Case Rep. 2023 Jan;13(1):5-11. doi: 10.13107/jocr.2023.v13.i01.3494. PMID: 37143566; PMCID: PMC10152949. [Google Scholar]