This is the only known case report of a successful closed reduction in an isolated distal fibula dislocation, as well as demonstrates a minimally invasive technique for definitive treatment with a dynamic syndesmosis fixation device for this rare Bosworth injury without fracture.
Dr. Daniel R Mesko, Department of Orthopaedic Surgery, Sparrow Hospital, Lansing, Michigan, USA/Michigan Orthopaedic Center, Lansing, Michigan, USA. E-mail: dmesko@michiganortho.com
Introduction: The Bosworth fracture-dislocation is a rare injury originally described as an irreducible dislocation of a distal fibula fracture where the proximal fibular fragment becomes incarcerated behind the distal tibia. There have since been a few cases described of an intact distal fibula with dislocation and similar difficulties in closed reduction attempts, typically seen with associated injuries to the ankle or proximal fibula. Regardless of the specific fracture or dislocation pattern, closed reduction attempts have consistently failed in the significant majority of these cases, which can lead to complications including soft-tissue compromise, severe post-traumatic arthritis, compartment syndrome, avascular necrosis of the talus, and neurovascular compromise. There is only one case in recent literature that describes an isolated distal fibula dislocation without associated fractures or dislocations of the lower extremity; however, it required an open reduction. Cases where a closed reduction was successful to achieve an anatomic reduction of a Bosworth-type injury are exceedingly rare.
Case Report: We present a rare case of a purely ligamentous, isolated distal fibula dislocation in a 21-year-old male who underwent a successful closed reduction upon initial presentation and later underwent surgical fixation with a syndesmosis repair system. We describe the technique used for a successful closed reduction for this injury and present a 1-year follow-up with excellent outcomes.
Conclusion: This is the only known case report of a successful closed reduction in an isolated distal fibula dislocation, as well as demonstrating a minimally invasive technique for definitive treatment with a syndesmosis repair system. Accurate diagnosis, early treatment, and anatomic reduction are imperative for good clinical outcomes and reducing complications for Bosworth injuries. This technique may improve the rates of successful closed reductions of Bosworth injuries upon initial presentation, leading to decreased complications and improved patient outcomes.
Keywords: Bosworth, fibula dislocation, reduction technique, syndesmosis repair.
Bosworth injuries are relatively rare fracture-dislocations of the ankle that are characterized by their difficulty in both diagnosis and anatomic reduction, leading to potentially severe consequences. Even more rare are Bosworth variant injury patterns with a dislocated, yet intact fibula. There have been a few cases in the literature over the past few decades of these injuries with a dislocated, intact distal fibula; however, most of these have had an associated fracture or dislocation in the ankle or proximal fibula [1-11]. Very few cases have been described where an anatomic reduction was achieved after a closed reduction attempt(s) [5, 7, 12-15]. To our knowledge, there is only one case in the literature that has documented an isolated distal fibula dislocation without associated fractures or dislocations in the leg, and it required an open reduction [4]. Delays in reduction or incomplete reduction can increase the chances of complications, which can further delay definitive treatment or lead to additional sequelae such as soft-tissue compromise, infection, post-traumatic arthritis, compartment syndrome, chronic pain, and loss of motion [1, 5, 6, 16]. There is a significant lack of literature regarding techniques for closed reduction to assist providers in managing these injuries [12, 13, 15]. We describe a technique used to successfully achieve a closed anatomic reduction in a patient with an isolated distal fibula dislocation, a variant of the originally described Bosworth fracture-dislocation. We also demonstrate the use of a new syndesmosis repair system to treat this injury in a minimally invasive fashion.
A healthy 21-year-old male presented to the emergency department with left ankle pain and an inability to weight bear after a fall from a motorcycle. He was driving at approximately 5 mph when he hit gravel and lost control, causing his motorcycle to tip over onto his left leg. The patient described catching his toe and a forced external rotation mechanism. He had immediate pain and swelling in his ankle and had been unable to bear weight. On presentation, he reported tingling across the top of his toes.
Clinical findings
On examination, he had mild deformity at the left ankle and was found to have diminished sensation in the distribution of the deep peroneal nerve at the first dorsal web space. Sensation was otherwise intact, motor function was limited due to pain but intact, and vascular function was intact. Severe edema was present localized at the medial ankle and moderate edema at the lateral ankle, with several small superficial abrasions across the medial ankle and foot. He reported mild tenderness over the lateral ankle and severe tenderness just distal and medial to the medial malleolus, with no tenderness at the medial malleolus itself or the proximal fibula.
Diagnostic assessment
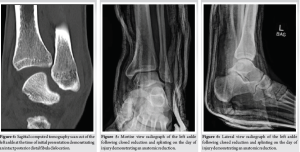
Initial radiographs of the left ankle in the emergency department demonstrated medial clear space widening of 8–9 mm. The lateral view demonstrated abnormal alignment of the ankle but was thought to be due to poor imaging, so repeat lateral films were ordered. Subsequent ankle films re-demonstrated abnormal alignment of the ankle, with the distal fibula appearing posteriorly translated (Fig. 1 and 2). Tibia-fibula radiographs were scrutinized and were negative for fractures at the proximal fibula. No fractures or other dislocations were present at the ankle, leg, or knee. A computed tomography (CT) scan was then performed that demonstrated a complete posteromedial dislocation of the distal fibula, with the distal fibula located posterior to the distal tibia and the talus subluxated approximately 25% laterally. There were no fractures present at the ankle or elsewhere in the tibia or fibula, indicating a purely ligamentous dislocation of the distal fibula behind the distal tibia (Fig. 3 and 4).

Reduction technique
A closed reduction was performed under conscious sedation using 25 mg ketamine and 50 mg propofol. The leg was held by an assistant in 90° of flexion at the hip and knee. The assistant also provided counterforce at the ankle with one hand on the anterior aspect of the distal tibia. The orthopedic provider then held the foot in plantar flexion, inversion, and a small amount of adduction. The other hand was placed with the fingertips wrapped posteriorly around the distal fibula. Once adequate sedation had been obtained, an anterolateral force was applied to the distal fibula, along with a small amount of internal rotation and a small amount of traction on the ankle. There was a palpable and visible snap as the fibula was reduced back into the incisura. The ankle was then placed in a well-padded, plaster short-leg splint and appropriately molded. Post-reduction radiographs demonstrated a reduced ankle in anatomic alignment (Fig. 5 and 6). The patient was neurovascularly intact upon re-examination, with resolution of his deep peroneal nerve paresthesia. He was made non-weight-bearing and was discharged home with plans for outpatient follow-up.
Follow-up and outcomes
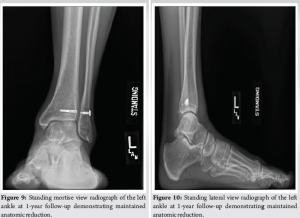
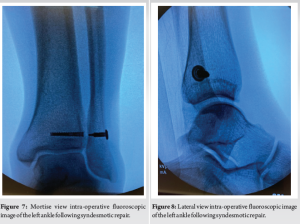
The patient followed up in the office 3 days after the injury, where repeat radiographs in the splint demonstrated a maintained reduction of the left ankle and syndesmosis. He then underwent a minimally invasive syndesmotic fixation using the FIBULINK® Syndesmosis repair system (DePuy Synthes, Monument, CO) 12 days after initial presentation (Fig. 7 and 8). After surgery, the patient was placed in a splint and made non-weight-bearing. He followed up 2 weeks after surgery for splint removal, radiographs, and an incision check, then was placed in a tall fracture boot. At that visit, he was cleared to start range-of-motion exercises out of the boot and continued non-weight-bearing restrictions for a total of 6 weeks. At the 6-week follow-up, the patient was allowed to start weight-bearing in the boot for 2 weeks, then transitioned to a lace-up brace out of the boot. He participated in 1 month of formal physical therapy, starting 6 weeks after surgery. At his 3-month follow-up, the patient had 0/10 pain and was walking without a boot or brace. Radiographs demonstrated the maintained alignment of his ankle joint. He was released to all activities at that time. At 1-year follow-up, the patient had 0/10 pain, maintained anatomic alignment of his ankle joint, and was participating in soccer as well as running for leisure without pain or difficulty (Fig. 9 and 10).
There are few cases reported in the literature describing a Bosworth injury with an intact fibula, and even fewer without an associated fracture or dislocation. The only case report in recent literature that describes an isolated distal fibula dislocation is by Collins et al. in 1998, which describes an 18-year-old male who had an external rotation injury to his ankle while in-line skating. He was splinted in the emergency department, then followed up in the clinic, where he underwent a failed closed reduction attempt without anesthesia and another attempt at closed reduction in the operating room the following day, before requiring an open reduction internal fixation with syndesmotic screws and an anterior inferior tibiofibular ligament repair [4]. Lovell published a case report in 1968 of a 13-year-old boy who sustained a distal fibula dislocation with an associated distal tibia physeal injury when tobogganing. He performed a successful closed reduction under sedation at the time of the injury by curling the fingertips of both hands around the distal fibula and lifting it anteriorly. The patient was treated with a cast and had good outcomes with normal motion and a stable ankle at 3-year follow-up [7]. Fleming and Smith described a case of a bimalleolar equivalent ankle fracture dislocation where a first reduction attempt partially reduced the tibiotalar joint and the second reduction attempt was successful at reducing the fibula using a direct pulling force on the posterior aspect of the fibular shaft [12]. In 2020, Fan et al. described a similar two-closed reduction attempt with reduction first of tibiotalar, dislocation then reduction of the fibula on the second attempt using a direct anterolateral force on the fibular shaft with the foot held in dorsiflexion, supination, and internal rotation for a bimalleolar ankle fracture-dislocation [13]. Our reduction technique was based on these two previously described methods with modifications to account for the physiologic motion at the ankle. Supination of the foot (plantar flexion, inversion, and adduction) is associated with anterior glide of the distal fibula with normal physiologic motion, whereas dorsiflexion leads to posterior motion of the distal fibula [17]. Therefore, we chose to utilize a supinated position of the foot along with the anterolateral force of the fibula for our closed reduction. In 1978, Mayer and Evarts described a case series in which 3 out of 4 patients with Bosworth fracture-dislocation injuries were successfully treated initially with closed reductions utilizing traction, inversion, internal rotation of the foot, and a lateral force on the fibula [15]. In 2021, Ji et al. reported a successful closed reduction of an ankle fracture subluxation upon a second attempt that ultimately underwent non-operative treatment [14]. Bartoníček et al. published a case series in 2007 of six patients along with a literature review analyzing 60 cases of Bosworth injuries that showed a pattern of injury based on patient age, with young adults most prone to dislocation of the fibula without fracture. They divided patients into three groups, showing that pediatric patients demonstrate fibular dislocation with associated epiphysioloysis of the distal tibia, young adults demonstrate distal fibula dislocations without fibular fractures, and older adults demonstrate fracture-dislocations of the fibula [5]. Our patient fits this pattern as a young adult with a dislocation of the fibula without a fracture. In addition, a recent literature review by Lucenti et al. reports a 92.2% rate of unsuccessful closed reductions for Bosworth injuries and a 10.7% rate of post-traumatic arthritis; however, they did not include studies before 2002 [18]. The literature has shown a significant lack of successful closed reductions of these injuries, with only two successful anatomic closed reductions documented in the last 20 years besides this case report. We believe that because a supinated foot leads to anterior distal fibular glide with normal motion and positions the talus where the more narrow posterior aspect is under the tibia, this position further assists in the reduction of a posterior distal fibular dislocation along with an anterolateral force on the fibula. Our case, along with the others described above, demonstrates that closed reductions can be successful in these injuries utilizing appropriate sedation and technique. In addition, utilizing a minimally invasive syndesmotic repair system in cases with an intact distal fibula can lead to less soft tissue compromise. We recommend the use of fluoroscopy at bedside to promptly evaluate the reduction in an attempt to reduce the need for repeat sedations, especially in cases of associated tibiotalar dislocations.
Tips for closed reduction in Bosworth injuries:
- High level of suspicion when the clinical picture does not correlate with radiographs
- Have a low threshold to obtain advanced imaging with a CT scan
- Adequate full sedation
- An assistant holds the lower extremity in 90° of knee and hip flexion
- The assistant also helps to provide a counterforce during the reduction of the distal tibia from anterior to posterior
- The provider holds the foot in supination (plantar flexion, inversion, and adduction)
- With the other hand, the provider wraps their fingers around the posterior distal fibula
- Traction is applied to the supinated foot
- An anterolateral force is applied to the distal fibula
- A visible or audible snap often occurs when the fibula reduces
- Use fluoroscopy at beside to evaluate the reduction of the fibula and associated injuries at the ankle
- Apply a well-molded splint.
Bosworth injuries are relatively rare; yet, they can lead to significant complications if not appropriately managed. In addition, they can be easily overlooked during initial imaging. There should be a high degree of suspicion when ankle imaging appears inconsistent with normal fracture-dislocation patterns or the clinical picture does not match up with the radiographs. There should be a low threshold to obtain CT imaging to further evaluate the injury pattern and ensure appropriate initial management. These injuries can lead to significant early complications, such as compartment syndrome with a need for emergent surgery, as well as late sequelae such as post-traumatic arthritis, chronic pain, and loss of motion. We believe that, with appropriate technique, the rate of successful closed reductions can be improved upon.
Using this technique for Bosworth injuries, the success rate of closed reductions may improve, which may significantly reduce the risk of complications and the need for emergent operative interventions. Improving the success rate of closed reductions may also allow for better operative planning and timing, which could lead to improved patient outcomes.
References
- 1.Williams AD, Blue M, Douthit C, Caroom C. Bosworth dislocation without associated fracture. Case Rep Orthop 2018;2018:7284643. [Google Scholar]
- 2.Wenxian P, Mehta KV. Rare Bosworth fracture-dislocation variant of an irreducible distal fibula dislocation of the ankle without fibula fracture. Foot Ankle Orthop 2019;4:2473011418820903. [Google Scholar]
- 3.Karachalios T, Pearse MF, Sarangi P, Atkins RM. Dislocation of the intact fibula with fracture of the medial malleolus. J Bone Joint Surg Br 1993;75:833-4. [Google Scholar]
- 4.Collins RS, O’Connor D, Denton JR. An irreducible distal fibula dislocation while in-line skating. J Orthop Trauma 1998;12:364-6. [Google Scholar]
- 5.Bartonícek J, Fric V, Svatos F, Lunácek L. Bosworth-type fibular entrapment injuries of the ankle: The Bosworth lesion. A report of 6 cases and literature review. J Orthop Trauma 2007;21:710-7. [Google Scholar]
- 6.He S, Zhu J. Ankle arthroscopy-assisted closed reduction in Bosworth fracture dislocation. SAGE Open Med Case Rep 2020;8:2050313X20974525. [Google Scholar]
- 7.Lovell ES. An unusual rotatory injury of the ankle. J Bone Joint Surg 1968;50:163-5. [Google Scholar]
- 8.Olerud S. Subluxation of the ankle without fracture of the fibula. A case report. J Bone Joint Surg Am 1971;53:594-6. [Google Scholar]
- 9.Hockenbury RT, Friermood TG. Dislocation of the distal tibiofibular joint. J Orthop Trauma 1992;6:120-4. [Google Scholar]
- 10.Perry CR, Rice S, Rao A, Burdge R. Posterior fracture-dislocation of the distal part of the fibula. Mechanism and staging of injury. J Bone Joint Surg Am 1983;65:1149-57. [Google Scholar]
- 11.Ren W, Hu YC, Lu JK. Rare variants of Bosworth fracture-dislocation: Bosworth fracture-dislocation with medial malleolus adduction type fracture. Chin J Traumatol 2019;22:120-4. [Google Scholar]
- 12.Fleming JL, Smith HO. Fracture-dislocation of the ankle with the fibula fixed behind the tibia. J Bone Joint Surg Am 1954;36-A:556-8. [Google Scholar]
- 13.Fan J, Michelin RM, Jenkins R, Hwang M, French M. A novel technique for a successful closed reduction of a Bosworth fracture-dislocation of the ankle. Cureus 2020;12:e6632. [Google Scholar]
- 14.Ji WB, Xu YF, Lu Z. Case report: Bosworth fracture-dislocation managed by closed reduction and conservative treatment. Front Surg 2021;8:788575. [Google Scholar]
- 15.Mayer PJ, Evarts CM. Fracture-dislocation of the ankle with posterior entrapment of the fibula behind the tibia. J Bone Joint Surg Am 1978;60:320-4. [Google Scholar]
- 16.Bartoníček J, Rammelt S, Kostlivý K. Bosworth fracture complicated by unrecognized compartment syndrome: A case report and review of the literature. Arch Orthop Trauma Surg 2021;142:1435-41. [Google Scholar]
- 17.Savarese R. Lower extremities. In: OMT Review. Jacksonville: Robert G. Savarese; 2003. p. 74. [Google Scholar]
- 18.Lucenti L, Testa G, Nocera C, Culmone A, Dell’Agli E, Pavone V. Bosworth fractures of the ankle: A systematic literature review. J Pers Med 2023;13:713. [Google Scholar]