Arthroscopic suture-assisted reduction and screw fixation provides a minimally invasive fail-safe management to treat acute bony Bankart, by preventing malrotation and facilitating early union.
Dr. Sreejith Thampy J, Department of Orthopaedics, Bangalore Shoulder Institute, Bengaluru, Karnataka, India. E-mail: drayyappanvnair@gmail.com
Introduction: Glenoid rim fractures with Bankart lesions are called bony Bankart lesions and are associated with persistent glenohumeral joint instability. Acute bony Bankart lesions can be treated by various arthroscopic techniques. Here, we present a technique of arthroscopic bony Bankart repair using suture-assisted reduction and screw fixation.
Discussion:The conventional suture anchor repair does not provide compression of the fractured fragment, and the bony piece may tilt because of the single-point fixation
Conclusion: This procedure can achieve firm compression between the bony fragments and prevent rotation of fragment during screw fixation to the glenoid. The capsular plication distributes the loads to the surrounding soft tissues. Hence, this procedure should be offered to all patients presenting acutely with a large bony Bankart of size >25% of glenoid width, as it is minimally invasive as well as provides excellent outcomes and anatomical union
Key words: Acute bony Bankart, shoulder dislocation, arthroscopic screw fixation, glenoid rim fracture, shoulder arthroscopy
Glenoid rim fractures with Bankart lesions are called bony Bankart lesions and are associated with persistent glenohumeral joint instability [1, 2]. The incidence of glenoid bone loss in anterior dislocation is 5.4%–44% [3]. Bony Bankart lesions can be treated by various arthroscopic techniques [4-9]. We present a technique of arthroscopic bony Bankart repair using suture-assisted reduction and screw fixation which can achieve firm compression between the bony fragment as well as prevent rotation of the fragment during screw fixation to the glenoid.
A 49-year-old man sustained a left shoulder fracture dislocation following a road traffic accident. Post-reduction radiograph showed a bony fragment and computed tomography (CT) revealed a bony Bankart lesion at the anteroinferior part of the glenoid articular surface along with an atypical Hill Sachs lesion and a non-displaced greater tuberosity fracture (Fig. 1). The size of the bony fragment was 35% of the glenoid surface area on the 3-dimensional CT (3D CT) and therefore, we decided to add screw fixation along with suture-assisted reduction by arthroscopic reduction and internal fixation of the bony Bankart lesion.
Indication and contraindication
This technique is indicated for all acute bony Bankarts/glenoid rim fractures occupying >25% glenoid width and contraindicated in recurrent dislocation (as the latter is associated with bony fragment erosion leading to insufficient coverage of glenoid track in which case additional bone grafting using coracoid or iliac crest is preferred).
Patient position
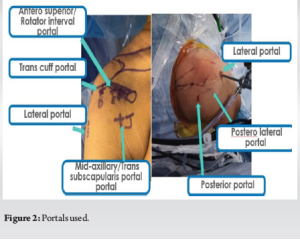
Patient was placed in the semi-beach chair position. The glenohumeral joint is set in neutral rotation and 30° of forward flexion with only 3 kg of distal traction. We used standard shoulder arthroscopic portals along with trans-subscapularis portal (Fig. 2).
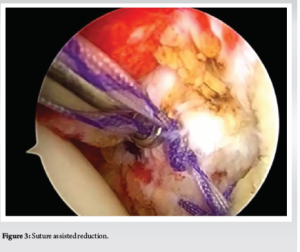
Standard posterior portal, the anterior skin incision was extended and an 8.25-mm twist-in cannula was placed into the glenohumeral joint to function as the primary working portal for repair. Further, a posterolateral portal was placed using a spinal needle perpendicular to the Hill Sachs lesion. Through the posterolateral portal, a triple-loaded all-suture anchor was put in the Hill Sachs lesion after thorough debridement with an arthroscopic shaver and burr. Multiple bites were taken using a bird beak through the tendinous part of infraspinatus over the Hill Sachs defect as part of remplissage. Through an anterosuperior portal, a periosteal elevator was used to mobilize the bony fragment. A 4.0-mm barrel burr was used to stimulate bleeding of the fragment and the native glenoid. Through an anterior-superior rotator interval portal, a 6-mm cannula is placed and an arthroscope is introduced al to provide a “bird’s-eye” view of the fragment and soft-tissue pathology. A large displaced bony fragment along with a ruptured capsulolabral structure was found medially. Adequate mobilization of fragment and capsulolabral tissue was achieved using 30° angled freer elevator. The footprint is then decorticated with an arthroscopic shaver. A posterolateral portal was used for suture passage into the inferior capsulolabral complex from 5 to 7 o’clock position. A single-loaded all-suture anchor was placed at a 6 o’clock position. Through the posterolateral portal, an angled suture-passing device (LASSO) is used to pass a suture shuttle (No. 1 polydioxanone suture) into the anterior band of the inferior glenohumeral ligament. Both sutures were retrieved through the posterolateral portal and provisionally tied through indirect reduction from the surrounding capsule. Through the trans-subscapularis portal, another double-loaded fiber tape anchor was placed at the 5 o’clock position (right shoulder), typically, providing an optimal angle for anchor insertion and the posterolateral portal used to retrieve sutures. Through the anterior portal suture, shuttle passer was introduced and passed around the whole bony fragment along with the capsulolabral complex (Fig. 3).
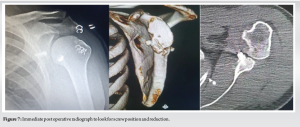
Once all sutures were passed, each pair of sutures were retrieved and tied in a sequential fashion beginning with the inferior-most sutures, working anterior-superiorly, thereby achieving anatomic reduction of the bony fragment. A cannula was inserted into the trans-subscapularis portal and a 3.5 mm × 34 mm cannulated cancellous Latarjet screw was used to fix and give compression to the bony fragment after confirmation of reduction of articular surface. The length of the screw was predetermined using preoperative CT scan (Fig. 4, 5, 6).
Another anchor was placed over the 4 o’clock position through the anterior rotator interval portal, and the rest of the capsulolabral tissue was plicated using a lasso loop as used for previous anchors. Following which the sutures passed through the tendinous part of infraspinatus over the Hill Sachs defect was knotted over the tendon and the remplissage was completed.
Post-operative protocol and follow-up
For immediate post-operative period, patient was started on shoulder shrugs, scapular retraction, elbow, and wrist range of motion exercises along with isometric shoulder strengthening exercises. After 2 weeks, passive range of motion was started till forward elevation of 90° and external rotation with the elbow at the side to 30°. Sling was discontinued at 4 weeks after which active-assisted and active range of motion exercises were started. Shoulder abduction and external rotation were avoided till 6 weeks. After 6 weeks, active external rotation to 45° and abduction to 90° was initiated. At week 12, full active range of motion was allowed and strengthening started. Return to sports was initiated at 6 months, after regaining sufficient strength determined by the physiotherapist and clinician.
Bony Bankart lesions have been generally treated by open reduction and internal fixation [1]. A 21% bony defect can cause instability as well as limit shoulder joint range of motion even after a Bankart repair [10]. Recently, arthroscopic reduction and internal fixation of bony fragments using cancellous screws or suture anchors have resulted in successful outcomes in terms of the recurrence rate and function in shoulders [4-6]. A firm compression can be achieved between the fragment and glenoid using a cancellous screw as in our technique as evidenced by the post-operative X-ray (Fig. 7).
The conventional suture anchor repair does not provide compression of the fractured fragment, and the bony piece may tilt because of the single-point fixation [5]. Along with the same adding another screw provides better compression. We chose the Latarjet screw of 3.5 mm, which is a cannulated cancellous screw as the fragment was of size >25% of glenoid width, whereas a smaller fragment has risk of being crushed with same and hence should be managed with 2 or 3 suture anchors in different constructs as already described in literature [4-9]. The screw fixation mentioned here provided us with sufficient compression to the fracture site promoting bony union (Fig. 7). Sano et al. reported an arthroscopic treatment using the double-threaded Japan screw along with suture anchors resulting with good clinical results [7]. In our technique, placing an additional screw to the fragment also facilitates stability of the bony fixation by providing compression between fragments and the capsular plication distributes the loads to the surrounding soft tissues. Our technique is different as, when conventional suture anchors prevent malrotation the screw provides compression, neither of which if done alone can provide both. Thus, this procedure is an amalgamation of the best available evidence applied at each step in performing this deceptively simple procedure in a bid to offer the most successful outcome to the patient.
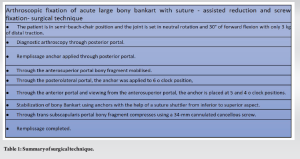
The surgical steps are summarised below (Table 1).
This procedure can achieve firm compression between the bony fragment as well as prevent rotation of fragment during screw fixation to the glenoid as well as the capsular plication distributes the loads to the surrounding soft tissues. Hence, this procedure should be offered to all patients presenting with a large bony Bankart of >25% of glenoid width in acute setting, as it is minimally invasive and provides excellent outcomes and anatomical union.
Arthroscopic management provides a minimally invasive way to treat acute bony Bankart and by placing suture anchors over fragment malrotation is prevented and the additional screw to the fragment facilitates early union by providing compression between fragments and the capsular plication distributes the loads to the surrounding soft tissues.
References
- 1.Kim SJ, Kim TW, Moon HK, Chang WH. A combined transglenoid and suture anchor technique for bony Bankart lesions. Knee Surg Sports Traumatol Arthrosc 2009;17:1443-6. [Google Scholar]
- 2.Cooke SJ, Starks I, Kathuria V. The results of arthroscopic anterior stabilization of the shoulder using the Bio knotless anchor system. Sports Med Arthrosc Rehabil Ther Technol 2009;1:2. [Google Scholar]
- 3.Griffith JF, Antonio GE, Yung PS, Wong EM, Yu AB, Ahuja AT, et al. Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patients. AJR Am J Roentgenol 2008;190:1247-54. [Google Scholar]
- 4.Cameron SE. Arthroscopic reduction and internal fixation of an anterior glenoid fracture. Arthroscopy 1998;14:743-6. [Google Scholar]
- 5.Kim KC, Rhee KJ, Shin HD. Arthroscopic three-point double-row repair for acute bony Bankart lesions. Knee Surg Sports Traumatol Arthrosc 2009;17:102-6. [Google Scholar]
- 6.Millett PJ, Braun S. The “Bony Bankart Bridge” procedure: A new arthroscopic technique for reduction and internal fixation of a Bony Bankart Lesion. Arthroscopy 2009;25:102-5. [Google Scholar]
- 7.Sano T, Matsuoka H, Nakayama K. Arthroscopic treatment of an anterior glenoid fracture with a cannulated, headless screw and suture anchors: A case report. Knee Surg Sports Traumatol Arthrosc 2009;17:539-41. [Google Scholar]
- 8.Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A. Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. J Bone Joint Surg Am 2005;87:1752-60. [Google Scholar]
- 9.Tauber M, Moursy M, Eppel M, Koller H, Resch H. Arthroscopic screw fixation of large anterior glenoid fractures. Knee Surg Sports Traumatol Arthrosc 2008;16:326-32. [Google Scholar]
- 10.Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: A cadaveric study. J Bone Joint Surg Am 2000;82:35-46. [Google Scholar]