We report the first case, from the Indian subcontinent, of the failure of mesenchymal segmentation leading to the talocrural coalition.
Dr. Punit Tiwari, Department of Orthopaedics, Maharishi Markandeshwar Medical College and Hospital, Solan, Himachal Pradesh, India. E-mail: punit_tiwari28@yahoo.com
Introduction: Coalition is an abnormal, usually congenital, or developmental connection in between or the complete fusion of two bones that are otherwise separate. It is of three types, i.e., synostosis (bony connection), synchondrosis (cartilaginous connection), or syndesmosis (fibrous tissue). Its typical cause is the failure of mesenchymal segmentation and differentiation. Usually, it is seen in tarsal or carpal bones and very rarely in between other bones. Only a single case of a tibiotalar coalition has been reported previously in literature. Herein, we are reporting a case of the talocrural coalition, which is the first one from the Indian sub-continent.
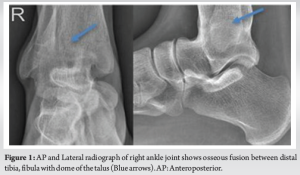
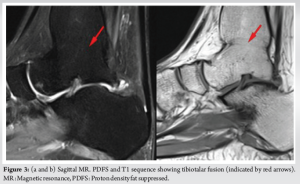
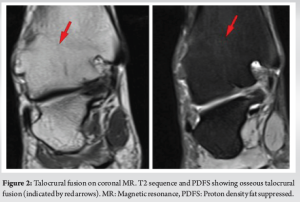
Case Report: A 16-year-old moderately built female patient of Indian origin presented with chronic pain of 1-year duration in the right foot and ankle region on weight bearing. The pain was dull aching type, mild-to-moderate in severity and worsened with activity or prolonged walking, and relieved on taking non-steroidal anti-inflammatory drugs. No relevant history was present. On local examination, diffuse tenderness was present in the ankle and the tarsal bones. Almost negligible dorsiflexion and about 15° plantar flexion of the foot were possible. An initial radiograph of the right ankle revealed osseous fusion between the distal tibia and fibula, as well as between the tibia, fibula, and the dome of the talus. Magnetic resonance imaging (MRI) revealed osseous fusion involving the distal tibia, fibula, and the dome of the talus (both medially and laterally), indicative of talocrural fusion. No edema or inflammation was appreciable in the adjacent tendons or synovium. The patient was explained regarding the pathology and the prognosis. She was managed conservatively and was satisfied.
Conclusion: Radiographs play a crucial role in evaluating patients suspected of having a coalition or ankylosis. Complementary tools such as computed tomography and MRI are valuable for a more in-depth assessment of the fusion and aid in surgical planning.
Keywords: Talocrural, tibiotalar, coalition, ankylosis, bony, osseous, fusion, synostosis, synchondrosis, syndesmosis.
From the osteology viewpoint, the coalition is an abnormal, usually congenital, or developmental connection in between, or the complete fusion of two bones that are otherwise separate in the normal majority population. It is categorized into three types based on the nature of bridging tissue in between the two bones, i.e., synostosis (bony connection), synchondrosis (cartilaginous connection), or syndesmosis (fibrous tissue) [1]. Its typical cause is the failure of mesenchymal segmentation and differentiation, in turn leading to failure of the formation of a normal joint between two bones. Usually, it is seen in tarsal or carpal bones and very rarely in between other bones. There is a discrepancy regarding the most common type of tarsal coalition. In some places, talocalcaneal and calcaneonavicular have been mentioned to be the most common types, with both occurring in an almost equal proportion and talonavicular being rare [2]. While Xiaojun Duan mentions talonavicular to be the most common one [3], on the other hand, Denning JR and skeletal radiology textbook Yochum and Rowe’s mention that calcaneo-navicular coalition is most common [4, 5]. Only a single case of a tibiotalar coalition has been reported so far by Clark et al. [6]. These coalitions are usually asymptomatic till the ossification of coalition in usually adolescent age leading to increased strain and subsequent degenerative changes at adjacent joints. A similar but different term is the ankylosis of joints which just denotes the stiffness of a joint preventing its motion. It is not congenital, rather it is acquired post-trauma, inflammatory, degenerative, or infective diseases of joints. In the adolescent age group, at times, it becomes difficult for the radiologist to differentiate between the two. Foot radiographs play a crucial role in evaluating patients suspected of having a coalition or ankylosis. Complementary tools such as computed tomography (CT) and magnetic resonance imaging (MRI)re valuable for a more in-depth assessment of the fusion and aid in surgical planning [7-9]. Herein, we are reporting a case of the talocrural coalition, which is the first one from the Indian subcontinent.
A 16-year-old moderately built female patient of Indian origin presented with chronic pain of 1-year duration in the right foot and ankle region on weight bearing. The pain was dull aching type, mild-to-moderate in severity and worsened with activity or prolonged walking, and relieved on taking non-steroidal anti-inflammatory drugs (NSAIDs). No history of trauma or any inflammatory pathology or pain or swelling in any other joint could be elicited. No relevant family history or consanguinity was present. There was no history suggestive of any inflammatory or auto-immune skin disease. On inspection, no redness, swelling, discharging sinus, prominent vessels, or deformity could be seen in the foot and ankle region. Local temperature was not raised on palpation and diffuse tenderness was present in the ankle (more toward the lateral side) and the tarsal bones. Almost negligible dorsiflexion and about 15° plantar flexion of the foot were possible. Complete blood counts, erythrocyte sedimentation rate, C-reactive protein, and anti-cyclic citrullinated peptide were unremarkable and within normal limits. An initial radiograph of the right ankle was sought by the clinician that revealed osseous fusion between the distal tibia and fibula, as well as between the tibia, fibula, and the dome of the talus (Fig. 1). The preliminary diagnosis was regarded as a congenital talocrural coalition.
Further detailed assessment of the deformity was carried out through a 3T MRI (SIEMENS MAGNETOM SKYRA) using a dedicated ankle coil. The MRI revealed osseous fusion involving the distal tibia, fibula, and the dome of the talus (both medially and laterally), indicative of talocrural fusion (Fig. 2 and 3). No edema or inflammation was appreciable in the adjacent tendons or synovium. The patient was explained regarding the pathology and the prognosis. She elected the conservative approach at this stage and is satisfied with 1-year follow-up.
Literature is replete with reports of single or multiple talar coalitions but to date, there has been only a single case report of a tibiotalar coalition reported by Clark et al. [6]. Coalitions are anomalous, congenital, or developmental unions occurring between two or more bones, either intraarticular or extraarticular, and complete or incomplete. The most prevalent forms of osseous coalitions are developmental. Common causes of post-infective ankylosis include septic arthritis, osteomyelitis, and post-traumatic infection. Other non-infective causes of ankylosis are inflammatory joint diseases such as rheumatoid arthritis, autoimmune conditions such as ankylosing spondylitis, and sometimes, even advanced osteoarthritis. In all these acquired conditions, the detected MR findings include bone marrow edema, periarticular erosions, osteolysis, geographic or permeative pattern of bone destruction, synovial proliferation, loose bodies, joint effusion, and soft tissue edema in acute presentation, while over time edema subsides and sclerosis predominates. [9-11]. None of these features were observed in our patient, effectively ruling out the possibility of this entity being an acquired condition. Its treatment involves addressing the underlying infection if it persists and managing the resulting joint deformity with an aim to achieve the alignment of the joint in a functional position. It may include antibiotics, joint debridement, physiotherapy, and surgical intervention. Physiotherapy can be instrumental in preventing additional stiffness and enhancing overall function. In a few cases, surgical procedures such as joint reconstruction or joint replacement may be considered to restore function and reduce pain. CT can characterize the coalitions better than X-rays, which is important for surgical planning. MRI is very adept at picking up the fibrous or cartilaginous bars and identifying early inflammatory or degenerative changes that may be missed in other imaging modalities. Coalitions alter the mechanics of the affected and the surrounding joints. As the natural movement between the two bones is absent, an unnatural stress is created at the nearby joints causing pain, sprains, and degenerative changes. The decision regarding the management of coalition or ankylosis is based on the site, type, and size of fusion, the presence of infection or degenerative changes in the affected or adjacent joints, deformity and limitation of movement, and the severity of pain. Usually, conservative measures are attempted first with NSAIDs, orthotics, and activity restrictions. If no relief, then coalition resection may be needed with/without deformity correction and arthrodesis is kept as the last option for those with failed resection or significant arthritis [12, 13].
Orthopedic surgeons should keep the possibility of talocrural coalition in young cases presenting with ankle pain without any history or features suggestive of traumatic or infective etiology and should not hesitate to rule out the same with advanced radiological imaging of the foot with CT or MRI.
Ankle and foot pain without any history of trauma or infection in adolescents could be indicative of tibiotalar, distal tibiofibular, or tarsal coalition.
References
- 1.Crim JR, Kjeldsberg KM. Radiographic diagnosis of tarsal coalition. AJR Am J Roentgenol 2004;182:323-8. [Google Scholar]
- 2.Ehrlich MG, Elmer EB. Saunders tarsal coalition. In: Jahss M, editor. Disorders of the Foot and Ankle. 2nd ed. Philadelphia, PA: W.B. Saunders; 1991. p. 921-38. [Google Scholar]
- 3.Duan X, Yang L. Treatment of isolated talonavicular coalition: Case report and literature review. J Int Med Res 2018;46:5322-30. [Google Scholar]
- 4.Denning JR. Tarsal coalition in children. Pediatr Ann 2016;45:e139-43. [Google Scholar]
- 5.Yochum TR, Rowe LJ. Essential of Skeletal Radiology. Vol. 1. Philadelphia, PA: Lippincott/Williams and Wilkins; 2005. p. 332-3. [Google Scholar]
- 6.Clark MJ, Murray J, Budhoo E, Metherall P, Highland A, Davies M. Tibio-talar coalition - a case report and review of the literature. Int J Anat Res 2019;7:7123-6. [Google Scholar]
- 7.Marth AA, Feuerriegel GC, Marcus RP, Sutter R. How accurate is MRI for diagnosing tarsal coalitions? A retrospective diagnostic accuracy study. Eur Radiol 2023 Oct 19. doi: 10.1007/s00330-023-10304-z. Epub ahead of print. [Google Scholar]
- 8.Lawrence DA, Rolen MF, Haims AH, Zayour Z, Moukaddam HA. Tarsal coalitions: Radiographic, CT, and MR imaging findings. HSS J 2014;10:153-66. [Google Scholar]
- 9.Newman JS, Newberg AH. Congenital tarsal coalition: Multimodality evaluation with emphasis on CT and MR imaging. Radiographics 2000;20:321-32; quiz 526-7, 532. [Google Scholar]
- 10.Weaver JS, Omar I, Mar W, Kauser AS, Mlady GW, Taljanovic M. Magnetic resonance imaging of rheumatological diseases. Pol J Radiol 2022;87:e93-112. [Google Scholar]
- 11.Alaia EF, Chhabra A, Simpfendorfer CS, Cohen M, Mintz DN, Vossen JA, et al. MRI nomenclature for musculoskeletal infection. Skeletal Radiol 2021;50:2319-47. [Google Scholar]
- 12.Catanzano AA Jr., Akoh CC, Easley ME, Mosca VS. Decision-making and management of tarsal coalition in the young adult patient: A critical analysis review. JBJS Rev 2023;11:6. [Google Scholar]
- 13.Shlykov MA, Minaie A, Schoenecker P, Hosseinzadeh P. Optimal surgical management of tarsal coalitions. Instr Course Lect 2020;69:371-80. [Google Scholar]