Knowledge of the double squeeze reduction clamp technique by using one reduction clamp on a smaller reduction clamp to stabilize a fracture or plate offers the surgeon greater variability when approaching fracture fixation.
Dr. Bruce E Heck, Northwest Ohio Orthopedics and Sports Medicine, Findlay, Ohio, USA. E-mail: drbruceheck@gmail.com
Introduction: The double squeeze technique for fracture stabilization is a technique in which the surgeon uses a second reduction clamp to hold and stabilize a smaller reduction clamp that reduces a fracture or plate yet is too small to hold by itself. This technique greatly assists anatomic fracture reduction and stabilization and allows the surgeon to complete the operation when there is limited reduction instrumentation available, or the surgeon needs more excursion on a small clamp holding a fracture and does not want to change instruments and possibly lose a reduction. We present a case of the double squeeze clamp technique, which to our knowledge has not been reported, to facilitate limited open reduction percutaneous plate stabilization in a distal tibia fracture.
Case Report: This case report presents an 18-year-old male with a closed, oblique, displaced right distal tibia fracture following a crush injury to the extremity with a tree while using a chainsaw. He was initially seen in the emergency room and was discharged home in a splint to follow-up with the orthopedic surgeon on call. The family requested follow-up with our practice 3 days later and requested surgery at their rural local hospital secondary to insurance reasons. Patient requested plate fixation to treat his fracture. Due to limited reduction instrumentation in the facility, a double squeeze reduction clamp technique using a pointed reduction clamp on a serrated reduction clamp that was too small to hold the plate on the reduced fracture accomplished stabilization of the plate on the fracture while screws were placed.
Conclusion: The double squeeze reduction clamp technique using one reduction clamp on a smaller reduction clamp greatly increases the ability to successfully reduce and stabilize multiple variations of different fractures whether secondary to differences in sizes of the bones, different types of bones, or in our case limited fracture reduction tools available.
Keywords: Double squeeze technique, reduction clamp, fracture reduction, fracture stabilization, tibia fracture.
Distal tibia fractures are complex injuries as they are more difficult to reduce, have higher rates of malalignment and knee pain with intramedullary (IM) nailing yet higher rates of wound problems and infection with plate fixation [1-5]. Limited open reduction percutaneous plate osteosynthesis (LORPPO) has shown similar outcomes to minimally invasive percutaneous plate osteosynthesis (MIPPO) [6]. The literature suggests minimally invasive plate osteosynthesis (MIPO) locking IM nail stabilization and external fixation combined with limited open reduction and absorbable internal fixation techniques are all efficient methods for treating distal tibia fractures [7]. MIPPO for tibial diaphysis and distal tibia fractures demonstrates low complication and high union rates [8]. Since prolonged surgical time increases the risk of surgical site infection [9], MIPO techniques to reduce operative time, hospital stay, and infection rate should be utilized [10]. Although there have been many reduction techniques described to accomplish tibial fracture reduction including manual reduction, indirect reduction, traveling traction, percutaneous clamps, provisional plating, or blocking screws, there is consensus that the use of adjunctive reduction techniques during fixation of tibia fractures is associated with a lower incidence of malalignment when compared to manual reduction alone [1, 2]. This case report describes a novel adjunctive technique to aid tibial fracture reduction and plate stabilization during osteosynthesis in an 18-year-old male after a tree struck his leg. The report highlights the importance of the double-squeeze reduction clamp technique and the importance of the patient’s involvement in surgical decision-making.
An 18-year-old male was cutting down trees with a high school friend when a tree rolled back onto his right leg. His past medical history was unremarkable except for attention deficit hyperactivity disorder. He was on no medication. Family medical history was significant for parents with arthritis and knee complaints. The patient was a nonsmoker. He reported that he was pinned by the tree and felt an immediate crunch when he was smacked in the leg before falling to the wet, soft ground where he was imbedded. Fortunately, his friend was able to cut the tree back into smaller pieces and then was able to use tree branches as levers to roll the tree off the patient’s lower leg. The patient was taken to the emergency department where he was evaluated with radiographs which revealed a displaced, oblique distal tibia shaft fracture. He was splinted with fiberglass and had follow-up arrangements with the orthopedic surgeon on call. Instead, the patient’s father had previous surgical treatment with the corresponding author and scheduled follow-up 5 days after the initial injury. The patient reported pain quality as a dull ache. He stated the pain was 2–3 on a scale of 10. When describing the pain, he stated it was intermittent. He did not have pain wake him at night. On physical examination, the patient was a 6’0”, 172-lb male with healthy appearance. The right leg was noted to have contusion with ecchymosis of the skin at the point of contact on the pretibial skin overlying the distal one third of the tibia. The skin was intact. The right lower leg was more swollen than the non-affected left leg. The patient’s pain to palpation was localized to the site of the fracture and tibiotalar joint. Patient had no pain with passive extension of the toes or foot. The patient had no pain over the tarsal-metatarsal joints. All lower extremity compartments were soft. Patient had intact pulses and neurovascular function. Radiographs revealed a displaced, oblique, valgus angulated distal tibia shaft fracture in a skeletally mature patient. Computerized tomography scan of the ankle revealed no fracture extension to the joint. The patient and family were recommended to undergo IM nailing for this fracture; however, due to the patient’s concern over knee pain and scar, he requested open reduction and internal fixation with surgery at a rural hospital near his home. In the meantime, the patient was placed in a well-padded, long leg fiberglass splint with stirrup and instructed to ice and elevate before surgery. The patient was taken to surgery 7 days after initial injury once surgical preparation was complete. Preoperatively, the patient received Ancef 2 g intravenous (IV) and tranexamic acid 10 mg/kg IV. He had general laryngeal mask anesthesia in the supine position. Thromboembolic stockings and compression pumps were placed on the non-operative side. The patient had a tourniquet applied to the right thigh inflated to 300 mmHg at the time of the procedure. Initially, C-arm fluoroscopic images taken intraoperatively were utilized to localize the fracture site and images saved (Fig. 1). Manual traction maneuvers to accomplish MIPO were attempted but unsuccessful.
A curvilinear incision starting lateral to the tibial crest at the fracture site and curving medially, distally overlying the medial malleolus was made. 3.5-mm loupe magnification was used and meticulous protection of skin edges with minimally invasive dissection limited to the fracture site with visualization and protection of the saphenous vein and nerve was performed. The periosteum was preserved except at the fracture site where it was noted to be stripped. The fracture was noted to be impacted with multiple spikes of bony interdigitation malalignment and interposed soft tissue preventing reduction and requiring removal before open reduction. Two Smith and Nephew serrated reduction clamps were used on the proximal and distal fracture fragments to provide distraction and a counter-rotation maneuver to dis-impact the fracture spikes resulting in visual reduction. Another Smith and Nephew serrated reduction clamp was placed on the fracture while C-arm fluoroscopic images confirmed anatomic alignment (Fig. 2).
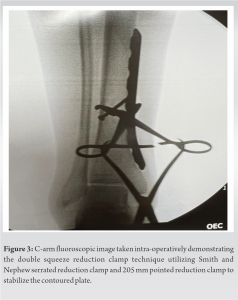
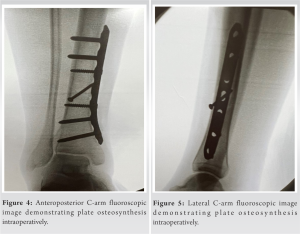
A 3.5-mm lag screw was then placed percutaneously resulting in limited fixation. A synthes 7-hole narrow 4.5 mm limited contact dynamic compression plate (LC-DCP) was contoured utilizing plate bender press and slid under the saphenous vein and nerve distally. Once the plate was contoured, there was no clamp available in the facility large enough to hold the plate stable to the distal tibia yet small enough to access a limited open fracture site. The serrated reduction clamp was barely large enough to get around the bone to stabilize the fracture without the plate but was not large enough to accommodate the 4.5 mm LC-DCP and the bone diameter. To overcome this in a facility where there were no other clamps available, a second clamp, Smith and Nephew 205-mm pointed reduction clamp, was then placed through the thumbholes of the serrated reduction clamp and then gently squeezed to hold the serrated reduction clamp firmly in place stabilizing the plate against the bone to allow for screw placement (Fig. 3). The patient then had compression screws placed proximally and distally to the fracture site followed by locking screws through soft tissue windows and percutaneously with fluoroscopic guidance (Fig. 4 and 5).
The patient had release of the tourniquet, irrigation, and closure of wounds with short leg fiberglass splint application. He was transferred to the recovery room in stable condition. Due to the lateness of the case being an add on surgery, the patient was observed overnight without problems, received IV first-generation cephalosporin antibiotics 24 h postoperatively, and was discharged home the next day. In follow-up, the patient had an uneventful recovery and was elated to not have any knee pain.
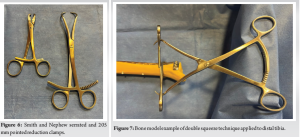
The double-squeeze reduction clamp technique is a straightforward, easy to use procedure utilizing a serrated reduction clamp and pointed reduction clamp (Fig. 6) to facilitate either fracture reduction or stabilization of the plate to the bone to free the surgeon’s hands and allow for precise placement and anatomic reduction of the plate and fracture (Fig. 3) when a reduction clamp of proper size is not available. This technique greatly assists anatomic fracture reduction and stabilization and allows the surgeon to complete the operation when there is limited reduction instrumentation, or the surgeon needs more excursion on a small clamp holding a fracture and does not want to change instruments and possibly lose the reduction. Although there have been many reduction techniques described to accomplish tibial shaft fracture reduction including manual reduction, indirect reduction, traveling traction, percutaneous clamps, provisional plating, or blocking screws, there is consensus that the use of adjunctive reduction techniques during fixation of tibia fractures is associated with a lower incidence of malalignment when compared to manual reduction alone [1, 2]. Our patient chose MIPO after extensive discussion regarding the risks and benefits of various forms of treatment. The patient and family requested to avoid the associated risk of knee pain associated with IM nailing, which was the recommended procedure to him, due to the family history of arthritis and knee pain, in a meta-analysis of 28 studies, evaluating IM nailing versus plating for distal tibia fractures without articular involvement, similar fracture to our patient’s injury, evidence suggests that both IM nailing and plating are appropriate treatments as IM nailing shows lower rate of delayed wound healing and superficial infection and plating may avoid malunion and knee pain [3]. Chronic anterior knee pain is the most common problem associated with IM nailing of the tibia, particularly younger patients that have a prominent nail tip, with an incidence of knee pain after tibia nailing to be as high as 91.8% with kneeling [4, 5].
In retrospect, LORPPO was the ideal fixation for this patient in view of the multi-interdigitated spikes of bone and interposed soft tissue in the displaced fracture site noted at the time of reduction and patient desire to avoid knee pain. LORPPO has shown similar outcomes to MIPPO [6]. In recent years, there have been many studies demonstrating that the MIPO technique is a safe and effective method of managing such fractures while avoiding some of the complications associated with conventional open-plating methods [7, 8]. Certainly, in our case, there was extensive planning, phone calls, and communication for 2 days before surgery with the instrumentation representatives, operating room director, and operating team to ensure all necessary equipment was available to accomplish fracture reduction and stabilization in a timely manner to minimize operating room time and surgical risks. Prolonged operative time has been shown to increase the risk of surgical site infection [9]. MIPO technique has been shown to be beneficial for the treatment of distal tibia fractures with reduced hospital stay, cost-effectiveness, and infection rate [10]. Despite our planning, there were limited surgical reduction clamps available at the facility during our case and no other clamps available that would accommodate the diameter of the bone with the plate. Fortunately, the knowledge of this technique provides an easy to administer solution to accommodate fracture reduction and stabilization in a variety of bone sizes and shapes within the same bone, different types of bone, or in our case limited reduction tools available. The same serrated reduction clamp and pointed reduction clamp has been utilized for fracture reduction and plate stabilization on both the tibia (Fig. 7) and femur (Fig. 8) due to the versatility of this technique. Furthermore, as there are increasing demands from hospitals to provide trauma care for patients at smaller hospitals and insurance providers dictating care to certain hospitals, there will be times when surgeons must operate at a facility that may not provide an unlimited resource of fracture reduction equipment. On the contrary, a surgeon may be at a larger institution, trauma center, or in a mass trauma casualty situation where resources could be depleted and the technique could be useful.
This case report highlights the importance of informed consent during the surgical process and emphasizes the need to discuss the risk and benefits of various treatment options for fracture care with a patient. The 18-year-old patient in our case did not want the risks of knee pain with IM tibial nailing and chose plate fixation. The double squeeze reduction clamp technique was a useful procedure to facilitate fracture reduction and plate stabilization osteosynthesis.
The double-squeeze reduction clamp technique is a straightforward, easy to use procedure that provides another tool in the surgeons’ arsenal that significantly increases the ability to successfully reduce and stabilize multiple variations of different fractures whether secondary to differences in sizes of the bones and plates applied, different types of bones, or limited fracture reduction tools available.
References
- 1.Behlmer RJ, Whiting PS, Kliethermes SA, Wendt L, Simske NM, Sato EH, et al. Reduction techniques for intramedullary nailing of tibial shaft fractures: A comparative study. OTA Int 2021;4:e095. [Google Scholar]
- 2.Dong WW, Shi ZY, Liu ZX, Mao HJ. Indirect reduction technique using a distraction support in minimally invasive percutaneous plate osteosynthesis of tibial shaft fractures. Chin J Traumatol 2016;19:348-52. [Google Scholar]
- 3.Mao Z, Wang G, Zhang L, Zhang L, Chen S, Du H, et al. Intramedullary nailing versus plating for distal tibia fractures without articular involvement: A meta-analysis. J Orthop Surg Res 2015;10:95. [Google Scholar]
- 4.Court-Brown CM, Gustilo T, Shaw AD. Knee pain after intramedullary tibial nailing: Its incidence, etiology, and outcome. J Orthop Trauma 1997;11:103-5. [Google Scholar]
- 5.Soraganvi PC, Anand-Kumar BS, Rajagopalakrishnan R, Praveen-Kumar BA. Anterior Knee pain after tibial intra-medullary nailing: Is it predictable? Malays Orthop J 2016;10:16-20. [Google Scholar]
- 6.Sah S, Bikash KC, Dangi SJ, Rai RK, Yadav R. Limited open reduction and percutaneous plate osteosynthesis-alternative option to minimally invasive plate osteosynthesis in management of distal tibia fractures. JNMA J Nepal Med Assoc 2017;56:456-60. [Google Scholar]
- 7.Li Y, Jiang X, Guo Q, Zhu L, Ye T, Chen A. Treatment of distal tibial shaft fractures by three different surgical methods: A randomized, prospective study. Int Orthop 2014;38:1261-7. [Google Scholar]
- 8.Aksekili MA, Celik I, Arslan AK, Kalkan T, Uğurlu M. The results of minimally invasive percutaneous plate osteosynthesis (MIPPO) in distal and diaphyseal tibial fractures. Acta Orthop Traumatol Turc 2012;46:161-7. [Google Scholar]
- 9.Cheng H, Chen BP, Soleas IM, Ferko NC, Cameron CG, Hinoul P. Prolonged operative duration increases risk of surgical site infections: A systematic review. Surg Infect (Larchmt) 2017;18:722-35. [Google Scholar]
- 10.Gülabi D, Bekler Hİ, Sağlam F, Taşdemir Z, Çeçen GS, Elmali N. Surgical treatment of distal tibia fractures: Open versus MIPO. Ulus Travma Acil Cerrahi Derg 2016;22:52-7. [Google Scholar]