External rotation of the shoulder against resistance likely exaggerates deformity of the injured acromioclavicular joint.
Dr. Thomas Robertson, University of Adelaide and Queen Elizabeth Hospital, Adelaide, South Australia, Australia. E-mail: thomas.robertson@sa.gov.au
Introduction: Acromioclavicular joint (ACJ) injuries account for more than 40% of all sports-related shoulder injuries. Early and effective diagnosis is crucial with surgical intervention favored over non-operative management in high-grade injury. At present diagnosis is primarily by plain radiography with a clear lack of good clinical examination techniques. This study aims to describe external rotation against resistance (ERAR) as a means of ACJ injury assessment.
Case Report: This case report describes three patients who presented to a local tertiary hospital with sporting injuries. In all cases, plain radiography demonstrated ACJ injury. Patients performed ERAR with the elbow by the side and flexed to 90° to assess for increase in ACJ deformity and coracoclavicular (CC) distance. The cases reported include two acute and one chronic ACJ injury. In all cases, this physical examination technique resulted in increased ACJ deformity and CC distance. This examination technique was well tolerated in all patients. All three patients underwent operative fixation and achieved excellent clinical outcomes.
Conclusion: In our experience, external rotation of the shoulder against resistance is a well-tolerated examination technique which has demonstrated good clinical utility, aiding in the diagnosis of moderate to high-grade ACJ injury. While this clinical examination technique may aid in the diagnosis of high-grade ACJ injury, the authors strongly recommend further clinical and radiological confirmation before the diagnosis of acute traumatic shoulder injuries.
Keywords: Acromioclavicular joint, shoulder, sports.
Acromioclavicular joint (ACJ) injuries are a frequent cause for presentation to the emergency department, accounting for more than 40% of all sports-related shoulder injuries [1]. Early and effective diagnosis of ACJ injury is crucial, particularly in cases with a higher degree of separation wherein acute surgical management may be favored [2]. ACJ injury results from situations where downward force is applied to the superior acromion while the clavicle remains static resulting in disruption of ACJ integrity. The resultant ACJ deformity is due to the rupture of the acromioclavicular (AC) ligament, rupture of the coracoclavicular (CC) ligaments, and rupture of the joint capsule. This most commonly occurs due to direct superior acromion trauma or fall on an outstretched arm adducted across the body, both a common occurrence in contact sports globally [3]. The clinical diagnosis of ACJ injury is complicated by differentials that mimic history and presentation including distal clavicle fracture, rotator cuff pathology, and shoulder dislocation. Misdiagnosis may result in patients undergoing inappropriate investigation, intervention, and temporizing management with resultant discomfort and risk of further damage to surrounding structures. At present, there are few examination techniques utilized to identify and differentiate ACJ injury, rather investigation is largely undertaken by plain AP, lateral, and Zanca view radiographs [4]. Upon completion of radiographic investigation and identification of ACJ pathology, injuries are graded and managed according to Rockwood classification (Type I through to type VI) [5]. Type I and II injuries describe AC and CC ligamentous sprain and partial tear, while type III-VI describe complete AC and CC ligamentous rupture. The CC ligament comprises the medial conoid and the lateral trapezoid ligaments which are essential for vertical stabilization of the ACJ. While type I and II injuries are treated non-operatively, type IV-VI injuries often require operative management. Type III injuries remain controversial with decisions being based upon a balance of patient factors and clinician preference [6]. In assessing shoulders that had sustained an AC joint injury, the senior author (a specialist upper limb surgeon) has noted that on testing external rotation power against resistance (ERAR) with the elbow by the side of the body and flexed to 90°, there was a distinct increase in the CC distance and worsening of ACJ deformity. We believe that this simple clinical test aids in the clinical diagnosis of ACJ injuries, by highlighting the higher grade injuries and therefore facilitating early and appropriate management of this shoulder pathology.
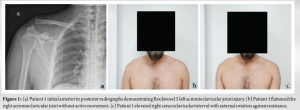
This study describes three patients that presented to a local tertiary hospital, two with acute and one with chronic sporting injuries. In all cases, the patients had AP radiographs of the shoulder which demonstrated ACJ injury. The acutely injured patients were triaged for rapid access clinical review in upper limb orthopedic clinic, while the patient with chronic injury was referred to the orthopedic clinic by their primary care practitioner. All patients underwent a thorough upper limb physical examination. As part of their physical examination, patients performed shoulder ERAR to assess the increase in prominence of ACJ injury. Images were obtained with written patient consent for use in scientific publication. A thorough search of the literature was performed investigating the existence of similar examination techniques with no such techniques existing. Two of the three cases were males with acute sporting injuries who presented to the emergency department of our tertiary hospital. As a result of their presentation and orthopedic consultation, these patients were triaged for rapid access clinical review in specialist upper limb orthopedic clinic. The third case was a female referred in by her primary health-care practitioner for consideration of operative management of her chronic ACJ injury. The first case is that of Patient 1, a 44-year-old male who sustained a right ACJ injury while playing cricket. The injury occurred when he fell onto an adducted right arm. He presented to the emergency department of our tertiary hospital where initial radiographs demonstrated a type III right ACJ injury (Fig. 1a). In the context of these radiology findings, a category one referral was made to the orthopedic outpatient clinic. At orthopedic clinic, Patient 1 was examined and noted to have increased ACJ injury prominence on shoulder ERAR (Fig. 1b and c). He underwent operative right ACJ stabilization as an emergency ambulatory case.
The second case is that of Patient 2, a 21-year-old male who sustained a left ACJ injury after falling onto his shoulder while wrestling. Initial radiographs demonstrated a Rockwood type III ACJ injury (Fig. 2a). As a result of his injury, a category one referral was made to the orthopedic outpatient clinic. At the orthopedic clinic, Patient 2 was examined and noted to demonstrate increased ACJ prominence with shoulder ERAR (Fig. 2b and c). Patient 2 underwent operative left ACJ stabilization.
The third case is that of Patient 3, a 49-year-old female who sustained a left ACJ injury in a cycling accident. At the time of injury, she presented to the emergency department of our tertiary hospital. She had a notable step deformity of the left ACJ and initial radiographs demonstrated a Rockwood type III ACJ injury (Fig. 3a). At the time of injury, the treating clinician deemed Patient 3 appropriate for non-operative management and she was discharged from ED. At 14 months, Patient 3’s GP referred her for orthopedic review and consideration of operative management due to persisting symptoms of instability and discomfort. She was triaged and reviewed in upper-limb orthopedic clinic. Despite these symptoms, Patient 3 did not report a significant inhibition in activities of daily living. Patient 3 was examined and noted to have a marked increase in CC distance and ACJ deformity with shoulder ERAR (Fig. 3b and c). Given the chronicity of injury, Patient 3 underwent elective surgical intervention.
In our upper-limb orthopedic clinic, all patients consented to photography of their ACJ at rest and while performing ERAR. The test of ERAR was performed with the shoulder adducted, elbow flexed to 90°, and against a medial rotational force applied at the wrist of the patient by the treating clinician. This clinical test was well tolerated without significant discomfort. In all patients, this maneuver resulted in increased CC interval and ACJ deformity as seen in Fig. 4.
This study indicates that shoulder ERAR is a well-tolerated clinical examination technique that may aid in the diagnosis of ACJ injury. In all cases, there was clinically evident widening of the CC interval and increased prominence of ACJ deformity (Fig. 4). In our experience, this clinical examination technique demonstrates good clinical utility when used to aid in the clinical diagnosis of moderate to high-grade ACJ injury. The authors of this paper propose two mechanisms by which widening of the CC interval and protrusion of the ACJ may occur. One proposed mechanism is due to external rotation the shoulder activating infraspinatus and teres minor muscles with resultant stretch and flattening of the overlying deltoid muscle causing a protrusion of the clavicle relative to the acromion. The other proposed mechanism is that rhomboid activation causes a retraction and stabilization of the scapula with resultant downward rotation and increase in ACJ deformity. It is however appreciable that multiple mechanisms could result in these findings and further investigation by means of dynamic imaging is required. On review of the literature, there are few previously described clinical examination techniques for use in ACJ injury. These include the O’Brien active compression test which has demonstrated utility in differentiating between ACJ injury and labral pathology. Despite its description in the literature, there is limited evidence supporting the clinical utility of the examination technique in differentiating between severity of ACJ injury [7]. The piano key sign, while utilized for injuries at other locations, has also been described for use in ACJ injuries. This elevation of the clavicle with ACJ injury will be compressible, rebounding on the removal of downward clavicular force [8]. Similarly, to O’Brien’s test, the utility of the piano key technique is poorly described across sources and is of questionable clinical utility. In addition, the Paxinos sign may be assessed and demonstrated by applying an anterior-superior compressive force across the injured ACJ. Positive assessment is demonstrated by symptomatology on examination [9]. Despite the numerous techniques described, there is no clear consensus regarding the isolated utility over another [10]. Despite the findings of this investigation, the authors do recognize the limitations of the results presented. In all cases, the patients had a diagnosis of ACJ injury before clinical examination. As such, investigation into whether ERAR could pre-radiographically diagnose ACJ injury or severity was unable to be performed. Furthermore, this was a limited case series of three patients who were not obese and already had clinically evident deformity of their affected shoulder. There was also no formal photographic imaging protocol and as such quantitative analysis was not able to be performed. Despite the limitations of this study, the described clinical examination technique of ERAR resulted in clinically an evident increase ACJ deformity and CC interval across all patients. With further investigation, it is possible that ERAR may demonstrate greater clinical utility when differentiating significance and grading of ACJ injuries. While the three cases in this series were radiographically diagnosed as type III ACJ injuries, it is possible that other injuries of the same grade may not have demonstrated as significant a CC interval widening with ERAR. As such greater increases in CC interval with ERAR may act as a surrogate marker of residual ACJ stability post-injury, guiding operative management and clinical decision-making. A larger cohort would be required to confirm the clinical utility of this test across patient populations, particularly in those of elevated body mass. The authors of this paper also believe that dynamic imaging studies, including ultrasound, would have utility in demonstrating the mechanism by which this examination technique works. Furthermore, plain radiography while performing ERAR may demonstrate quantifiable increase in CC distance, not only further assisting in clinical and operative decision-making, but also having the potential to offer a new means of ACJ injury classification.
This case series presents three patients, all who were not obese and already had clinically and radiologically obvious ACJ deformities. All patients underwent physical examination by ERAR which demonstrated worsening of ACJ deformity and increase in CC interval. While this clinical examination technique may aid in the diagnosis of ACJ injury, the authors strongly recommend further clinical and radiological confirmation before the diagnosis of acute traumatic shoulder injuries. Despite this, ERAR is a safe well-tolerated examination technique that may be utilized by orthopedic or sports clinicians for immediate assessment and diagnosis of high-grade ACJ injuries.
ERAR exaggerates the deformity of ACJ injury. The authors propose that, in the absence of radiological assessment, increased ACJ deformity on ERAR may act as a surrogate marker of instability and therefore requirement for surgical fixation. Further large cohort radiological investigations are required to formally establish its relationship with grade of injury and its utility in acting as a surrogate marker of ACJ stability.
References
- 1.Mazzocca AD, Arciero RA, Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med 2007;35:316-29. [Google Scholar]
- 2.Berthold DP, Muench LN, Dyrna F, Mazzocca AD, Garvin P, Voss A, et al. Current concepts in acromioclavicular joint (AC) instability - a proposed treatment algorithm for acute and chronic AC-joint surgery. BMC Musculoskelet Disord 2022;23:1078. [Google Scholar]
- 3.Sirin E, Aydin N, Mert Topkar O. Acromioclavicular joint injuries: Diagnosis, classification and ligamentoplasty procedures. EFORT Open Rev 2018;3:426-33. [Google Scholar]
- 4.Tauber M, Koller H, Hitzl W, Resch H. Dynamic radiologic evaluation of horizontal instability in acute acromioclavicular joint dislocations. Am J Sports Med 2010;38:1188-95. [Google Scholar]
- 5.Rockwood C. Injuries to the acromio-clavicular joint. Fract Adults 1984;1:860-910. [Google Scholar]
- 6.Gorbaty JD, Hsu JE, Gee AO. Classifications in brief: Rockwood classification of acromioclavicular joint separations. Clin Orthop Relat Res 2017;475:283-7. [Google Scholar]
- 7.O’Brien SJ, Pagnani MJ, Fealy S, McGlynn SR, Wilson JB. The active compression test: A new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. Am J Sports Med 1998;26:610-3. [Google Scholar]
- 8.Kiel J, Kaiser K. Acromioclavicular joint injury. In: StatPearls. Treasure Island, FL: StatPearls Publishing LLC; 2021. [Google Scholar]
- 9.Walton J, Mahajan S, Paxinos A, Marshall J, Bryant C, Shnier R, et al. Diagnostic values of tests for acromioclavicular joint pain. J Bone Joint Surg Am 2004;86:807-12. [Google Scholar]
- 10.Krill MK, Rosas S, Kwon K, Dakkak A, Nwachukwu BU, McCormick F. A concise evidence-based physical examination for diagnosis of acromioclavicular joint pathology: A systematic review. Phys Sportsmed 2018;46:98-104. [Google Scholar]