Truama leading to ligamentous injury can lead to onset or exaggeration of rheumatoid arthritis symptoms in a joint and unusual synovitis pattern during arthroscopic surgery warrants further work up.
Dr Raghavendra Kembhavi, Consultant Arthroscopy Surgeon (Shoulder, Hip and Knee) KVC Superspeciality Hospital , Krishna Vilas Road, Near Ideal Jawa Rotary School, Mysore -570005 , India. E-mail: kembhavi.raghavendra@gmail.com
Introduction: The relationship between physical trauma and subsequent symptoms of rheumatoid arthritis (RA) has been described in the past though onset of newer disease of RA in apparently normal patient is doubtful. Trauma can cause precipitation of RA symptoms. Such trauma includes fractures, joint injuries, road traffic accidents, and also surgeries and deliveries. Although post-traumatic osteoarthritis following anterior cruciate ligament (ACL) injury is more common pathology, association of RA following ACL injury has not been reported in the literature. This case report highlights on one rare incidental diagnosis of RA postoperatively in a patient with traumatic ACL tear with previously no features of RA and how patient was managed successfully both by surgical and by medical management.
Case Report: A 30-year-old male patient presented to us with complaints of pain over right knee associated with recurrent swelling, instability, clicking sounds, and occasional locking episodes since 6 months following twisting injury with no other symptoms in other joints of the body. Based on clinicoradiological workup, the diagnosis of traumatic complete ACL tear with medial meniscus bucket handle tear of body and posterior horn with early osteoarthritic changes was made. The patient was operated with ACL reconstruction with quadrupled hamstring graft, partial medial meniscectomy and debridement + microfracture for cartilage defects. The patient was worked up for inflammatory arthritis post operatively considering unusual synovitis of knee. Based on histopathological and serological investigations (rheumatoid factor and anticitrullinated protein antibody), the patient was put on disease modifying antirheumatoid drugs for 1 year. At 1-year follow-up, the patient was back to his normal activities with full range of movements with Lysholm Knee Score of 89.
Conclusion: Traumatic ACL tear can result in onset of RA following trauma and needs to be worked up further when there are findings of unusual synovitis or cartilage damage arthroscopically. Such association is rare and concomitant diagnosis of RA or other inflammatory arthritis can be easily missed out if not addressed properly.
Keywords: Synovitis, inflammatory arthritis, meniscectomy, chondral, pannus.
Anterior cruciate ligament (ACL) injuries are one of the commoner ligament injuries and ACL reconstruction surgery is one of the widely performed surgeries by orthopedic surgeons around the world [1]. ACL is an important contributor of knee stability and therefore ACL injuries leading to secondary osteoarthritic changes are well documented [2]. Mechanism for the development of osteoarthritis following ACL injuries are multifactorial which include initial injuries to subchondral bone and hyaline cartilage at the time of trauma to chronic changes in cartilage and meniscus due to changes in the static and dynamic loading of the knee joint in absent ACL knees [3]. However, unlike osteoarthritis, development of rheumatoid arthritis (RA) following ACL injuries has not been studied previously. Furthermore, there has not been documented literature between ACL injuries and RA in the past. However, there are studies which show the correlation between physical trauma and RA symptoms. Brawer and Goel showed that physical trauma may exaggerate symptoms of RA in already known patient of RA but it cannot be concluded that physical trauma as a causative agent for initiation of RA [4]. Possible mechanism for initiation or accentuation of RA symptoms includes increased synovial infiltration of chronic inflammatory cells into the joint leading to synovitis and increased quantity of biomarkers like antibodies to Type II collagen inside the joint and serum. This case report highlights on one rare incidental diagnosis of RA in a patient with traumatic ACL tear who was apparently normal before trauma with no features of RA and how the patient was successfully managed with ACL reconstruction and medical management with disease modifying anti-rheumatoid drugs (DMRDs).
A 30-year-old male patient presented to our outpatient department with complaints of pain over right knee associated with recurrent swelling, instability, clicking sounds, and occasional locking episodes since 6 months following injury and all the symptoms started following significant twisting injury over knee while playing kabaddi with no prior history of any symptoms. Following trauma, the patient had only bandages application with massage at local bonesetter. At presentation to us, examination revealed medial joint line tenderness. There was minimal effusion with no varus or valgus laxity. Anterior drawers test, Lachman’s test, and Pivot-Shift tests were positive. McMurray test for medial meniscus was positive. There was significant quadriceps wasting. Range of movements was terminally painful and restricted. Lysholm Knee Scoring showed a score of 31. However, there were no other symptoms in any parts of the body/joints. The patient was worked up with plain radiography which showed minimal arthritic changes with marginal osteophyte with fairly maintained joint space (Kellgren-Lawrence grade II) (Fig. 1) and magnetic resonance imaging showed complete ACL tear with bucket handle tear of posterior and body of medial meniscus with double posterior cruciate ligament sign with hyperintense signal in posterior medial femoral condyle suggesting possible cartilage damage (Fig. 2). The diagnosis of traumatic complete ACL tear with medial meniscus bucket handle tear of body and posterior horn with early osteoarthritic changes was made. We planned for arthroscopic surgery. Intraoperatively, we found complete tear of ACL with bucket handle tear of medial meniscus with cartilage defect of 3 cm × 3 cm at medial femoral condyle (Fig. 3). Cartilage defect was addressed with debridement and microfracture. Furthermore, we noticed extensive usual amount of synovitis in the knee which was debrided and was sent for histopathology and culture sensitivity (Fig. 4). ACL reconstruction was done with quadrupled hamstring graft and fixation with titanium screws with partial medial meniscectomy. Considering the unusual and extensive amount of synovitis noticed in the knee, we decided to work up for inflammatory arthritis postoperatively. Histopathological study revealed non-specific synovial proliferation with infiltration of chronic inflammatory cells including plasma cells, lymphocytes and occasional neutrophils (Fig. 5) and culture sensitivity was negative. However, there were no lymphoid follicles or pannus. Furthermore, we found that both rheumatoid factor and anticitrullinated protein antibody (anti-CCP) to be positive postoperatively and accordingly, the patient was put on DMRD’s with combination of tablet sulfasalazine 500 mg, tablet hydroxychloroquine 200 mg on daily basis, and tablet methotrexate 7.5 mg for 1 year alongwith folic acid supplementations. Furthermore, the patient was informed regarding further cartilage managing surgical procedures after surgery; however, the patient denied due to financial constraints. He was put on long knee brace for 6 weeks. Isometric knee exercises were started on day 1 postoperatively, knee range of movements after 2 weeks, and non-weight bearing for 6 weeks. The patient was followed up regularly at 3 weeks, 6 weeks, 12 weeks, 6 months, and 1 year. At 1-year follow-up, the patient was back to normal activities with no instability symptoms or pain or clicking sensations over knee with full range of movements (Fig. 6). Lysholm Knee Scoring had improved significantly to 89. However, radiological features showed osteoarthritic changes with Kellgren-Lawrence grade III (Fig. 7).


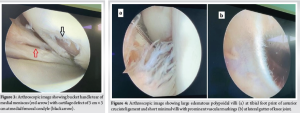
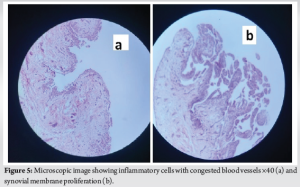

RA is essentially polyarticular disease although it can be monoarticular which is rare and can involve larger joints such as hip and knee [5]. Untreated cases eventually progress to polyarticular RA. Considering the rarity of monoarticular RA, it is often missed diagnosis in clinical practice and other commoner differential diagnosis is often emphasized in monoarticular disease like tuberculosis, gout, pseudo-gout, autoimmune diseases such as arthritis due to seronegative spondyloarthritis, pigmented villonodular synovitis, single joint osteoarthritis, and neuropathic arthropathy [6]. Furthermore, classical RA symptomatology involving morning stiffness and smaller joint involvement will not be seen in monoarticular RA disease and similarly our patient too did not have any of these symptoms before injury. Physical trauma leading to onset or exacerbation of already existing RA symptoms has been described previously [4, 7]. Al-Allaf et al., in their study, showed strong association with following type of physical injuries 6 months before onset of RA symptoms which included fractures, joint injuries, road traffic accidents, and also surgeries and deliveries [7]. It is unclear why certain proportion of population develops onset of RA or exacerbation of symptoms and others do not. This could be possibly due to genetic predisposition to autoimmune disorders in such group of population leading to symptoms. Our patient too had twisting injury to knee 6 months before onset RA symptoms over knee. Pattern of synovitis macroscopically during arthroscopic examination is suggestive of particular pathologies although it may not be conclusive in all cases since appearance of synovium differs in different stages of disease [8]. Therefore, diagnosis of particular pathology just on the look of synovium is difficult although it may give clue on particular pathology. In inflammatory arthritis, synovial villi are thick, edematous, and polypoidal whereas in reactive arthritis, it is only marked vascular formation without villi formation [9]. Considering mixed pattern of synovial proliferation with some areas of knee joint showing edematous villous hypertrophy with polypoidal mass and other areas showing minimal villi with prominent vascular markings, we decided to work up for inflammatory arthritis postoperatively with disease probably suggesting different stages of inflammatory arthritis. Microscopic evaluation of synovial tissue in RA gives us confirmatory clue on whether disease process early or late or established erosive type of RA. In early disease, histological features show synovial layer hypertrophy with infiltration of chronic mononuclear inflammatory cells with fibrin deposits and increased vascularity. These features can be seen as early as 6 weeks from the disease whereas chronic, established, and aggressive form of RA is diagnosed microscopically by the presence of lymphoid follicles and presence of pannus [10]. Cartilage or chondral damages are commonly seen in chronic ACL tear patients eventually leading to post-traumatic osteoarthritis (PTOA) [11]. Various mechanisms described in development of PTOA following ACL tear include structural, biological, mechanical, and neuromuscular factors. Similarly in RA patients too cartilage and bone erosions are more common end points in long-standing disease. Possible mechanisms in such patients leading to cartilage injury include direct erosions by pannus, erosive synovitis, and eventual cartilage damage by migrant inflammatory mediators from bone and subcortical bone ending up in joints, and angiogenesis over cartilage in RA patients because cartilage is essentially avascular in normal patients [12, 13]. Our patient too had chondral defect in medial femoral condyle which could be possibly due to both, that is, ACL deficiency and recent onset of RA disease. This case report highlights on need of high degree of suspicion in unusual cases of synovitis while doing ligament reconstruction and need for workup for the etiology in such cases as it can be missed out easily. Such findings of RA in a patient with traumatic ACL patient have not been mentioned previously according to our knowledge. Cartilage lesions are dreadful and not addressing such problems can lead to arthritic joint which needs to be followed up for longer duration and both the conditions are limitations of the study.
Traumatic ACL tear can result in onset of RA following trauma and particularly needs to be worked up further when there are findings of unusual synovitis or cartilage damage arthroscopically. Such association is rare and concomitant diagnosis of RA or other inflammatory arthritis can be easily missed out if not addressed properly.
Monoarticular RA is rare diagnosis and several important differential diagnosis such as tuberculosis, gout, pseudo-gout, autoimmune diseases, pigmented villonodular synovitis, and neuropathic arthropathy should be kept in mind. Trauma leading to RA or exacerbation has been described in literature eventhough incidence is quite less. In such cases of traumatic ligamentous injury, concomitant diagnosis of RA can be easily missed particularly when patient does not show any symptoms of RA before injury. Pattern of synovitis, microscopic examination, and thorough careful work up with high degree of suspicion will help in achieving proper diagnosis and treatment accordingly.
References
- 1.Paschos NK, Howell SM. Anterior cruciate ligament reconstruction: Principles of treatment. EFORT Open Rev 2017;1:398-408. [Google Scholar]
- 2.Friel NA, Chu CR. The role of ACL injury in the development of posttraumatic knee osteoarthritis. Clin Sports Med 2013;32:1-12. [Google Scholar]
- 3.Andriacchi TP, Mundermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S, et al. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng 2004;32:447-57. [Google Scholar]
- 4.Brawer AE, Goel N. The onset of rheumatoid arthritis following trauma. Open Access Rheumatol 2016;8:77-80. [Google Scholar]
- 5.Douraiswami BT. Monoarticular rheumatoid arthritis of the wrist: A rare entity. OA Case Rep 2013;10:80. [Google Scholar]
- 6.Sarazin J, Schiopu E, Namas R. Case series: Monoarticular rheumatoid arthritis. Eur J Rheumatol 2017;4:264-7. [Google Scholar]
- 7.Al-Allaf AW, Sanders PA, Ogston SA, Marks JS. A case-control study examining the role of physical trauma in the onset of rheumatoid arthritis. Rheumatology (Oxford) 2001;40:262-6. [Google Scholar]
- 8.Kuzmanova SI, Zaprianov ZN, Solakov PT. Correlations between arthroscopic findings and synovial membrane histology in patients with rheumatoid synovitis of the knee joint. Folia Med (Plovdiv) 2003;45:60-5. [Google Scholar]
- 9.Goyal T, Paul S, Choudhury AK, Kalonia T. Monoarticular synovitis of knee: Dealing with the dilemma. SICOT J 2020;6:48. [Google Scholar]
- 10.Hitchon CA, El-Gabalawy HS. The synovium in rheumatoid arthritis. Open Rheumatol J 2011;5:107-14. [Google Scholar]
- 11.Wang LJ, Zeng N, Yan ZP, Li JT, Ni GX. Post-traumatic osteoarthritis following ACL injury. Arthritis Res Ther 2020;22:57. [Google Scholar]
- 12.Sudoł-Szopińska I, Zaniewicz-Kaniewska K, Warczyńska A, Matuszewska G, Saied F, Kunisz W. Pathogenesis of rheumatoid arthritis in radiological studies. Part II: Imaging studies in rheumatoid arthritis. J Ultrason 2012;12:319-28. [Google Scholar]
- 13.Ostrowska M, Maśliński W, Prochorec-Sobieszek M, Nieciecki M, Sudoł-Szopińska I. Cartilage and bone damage in rheumatoid arthritis. Reumatologia 2018;56:111-20. [Google Scholar]









