Early surgical intervention aimed at drainage or stabilization of infectious lesions is crucial to disease control in cases with ankylosing spinal disorders.
Dr. Satoshi Kawaguchi, Department of Orthopaedic Surgery, Asahikawa Kosei General Hospital, 24 Chome-111, 1 Jodori, Asahikawa 078-8211, Japan. E-mail: kawaguch@sapmed.ac.jp
Introduction: Ankylosing spinal disorders present significant challenges in cases of trauma, and the treatment of ankylosed spine infections may also be challenging. However, to the best of our knowledge, only one study to date has addressed this topic, reporting a mortality rate of 62%.
Case Report: Our patients were four men and one woman with a mean age of 72 years. Treatments consisted of intravenous antibiotics, a hard brace, and surgical interventions including percutaneous pedicle screw fixation in two patients, laminectomy and evacuation of the epidural abscess in one, and percutaneous lavage of the affected disc in two. The time from referral to intervention averaged 16 days. The mortality rate was 0% with healing of the infection with segmental bony fusion in four patients.
Conclusion: This is the second reported case series of ankylosed spine infections. Early surgical intervention aimed at drainage or stabilization of the infectious lesions is crucial to disease control.
Keywords: Ankylosing spinal disorders, infection, spondylodiscitis, percutaneous pedicle screw fixation.
Ankylosing spinal disorders (ASDs) such as ankylosing spondylitis and diffuse idiopathic skeletal hyperostosis are chronic conditions with major symptoms of reduced mobility and deformity of the trunk [1, 2]. They present significant challenges in cases of trauma, given the unstable configuration of ankylosed spine fractures [3-5]. Likewise, the treatment of ankylosed spine infections may also be challenging due to the destructive nature of the infectious processes. However, information is scarce as, to the best of our knowledge, only one study has addressed this topic, reporting 13 patients with ankylosed spine infection [6]. Here, we report five cases of ankylosed spine infection and discuss treatment outcomes and the significance of surgical intervention.
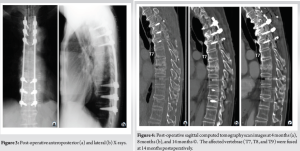
Case 1 was a 70-year-old male with a history of urethral cancer treated with total cystectomy. He was referred for severe back pain with destructive lesions of the mid-thoracic vertebrae. At referral, the patient had difficulty moving due to back pain. Physical examination found no motor weakness or sensory disturbance. Computed tomography (CT) scans showed destruction of the T7, T8, and T9 vertebrae with paravertebral soft-tissue swelling (Fig. 1a and b). In addition, ankylosis of the spine was noted from T2 to T7 and from T9 to L1 with ossification of the anterior longitudinal ligament. CT scans taken 1 year earlier demonstrated ankylosis from T7 to T9 (Fig. 1c), indicating the formation of ankylosis from T2 to L1 before the present examination. Magnetic resonance imaging showed discovertebral signal changes in the T7-T9 vertebrae with putative formation of an intradiscal abscess at the T8/9 intervertebral disc level (Fig. 2a, b, c). Laboratory test results revealed a white blood cell count of 9300/μL and C-reactive protein (CRP) of 16.03 mg/dL. Blood cultures confirmed methicillin-resistant Staphylococcus aureus (MRSA). On the diagnosis of infectious spondylodiscitis in the T7, T8, and T9 vertebrae within the ankylosed thoracolumbar segment (T2-L1), intravenous antibiotic therapy was initiated, followed by percutaneous posterior instrumentation from T4 to T12 at 1 week (Fig. 3a and b). CRP normalized 1 week after the surgical treatment. Follow-up CT scans confirmed fusion of the T7, T8, and T9 vertebrae at 14 months postoperatively (Fig. 4a, b, c).
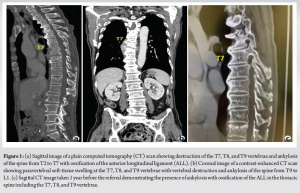
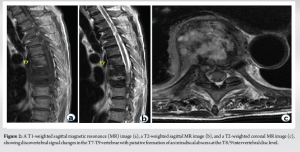
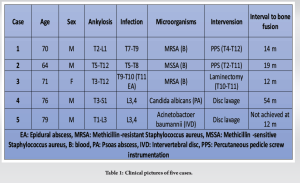
Table 1 summarizes the clinical features of the five cases. There were four men and one woman with a mean age of 72 years (range: 64–79 years). Levels of ankylosis included the thoracic (T5-T12), thoracolumbar (T1-L3, T2-L1, and T3-L2), and thoracolumbosacral (T3-S1) spine. Four patients had infection in the ankylosed spine (T5-T8, T7-T9, T9-T10, and L3-L4), and one patient had infection at the end of the ankylosed spine (ankylosis: T1-L3; infection: L3-L4). The patient with spondylodiscitis of the T9-T10 vertebrae had an epidural abscess at the T11 level. The causative organisms were MRSA in two patients and methicillin-sensitive S. aureus, Acinetobacter baumannii, and Candida albicans in one patient each. The present treatments consisted of intravenous antibiotics and a hard brace. In addition, two patients with thoracic spine infections underwent percutaneous pedicle screw (PPS) fixation. The patient with the epidural abscess at T11 underwent laminectomy and evacuation of the epidural abscess for progressive paraplegia. The remaining two patients with lumbar spine infections received percutaneous needle biopsy and lavage of the affected disc. The time from referral to intervention averaged 16 days (range: 7–29 days). In the two patients who underwent PPS fixation and the patient who underwent laminectomy, the infection healed with bony fusion in about 1 year with no recurrence. In the two patients who underwent disc lavage, CRP levels returned to normal within 4 months. However, the disease flared up following the discontinuation of intravenous antibiotic therapy. One case ultimately required 4 years until the infected vertebrae fused. The other patient had failed to achieve fusion of the affected vertebrae at the final follow-up at 1 year.
In this report, we present five cases of bacterial or fungal infections of an ankylosed thoracolumbar spine segment. To the best of our knowledge, the literature includes only one other study addressing the same topic [6]. Therefore, we compare these two reports in our discussion of the treatment courses and outcomes of the patients. A significant finding in the study by Yamada et al. [6] reporting 13 patients with ankylosed spine infections is their poor life expectancy, with a mortality rate of 62% (eight patients). In contrast, the mortality rate was 0% in our five patients during follow-up periods from 12 months to 54 months. In Yamada’s study, one patient died of heart failure at 2 year after treatment, and all of the remaining seven patients died within 0.9 year [6], suggesting that the short follow-up periods of our study almost certainly did not affect the difference in mortality rates. The difference in mortality rates between the two studies may be due to the management of the patients, including surgical interventions. In Yamada’s et al. study [6], only 3 of the 13 patients underwent surgical intervention (posterior drainage in two and anterior debridement and fusion in one). In contrast, in our series, all five patients underwent surgical intervention within an average of 16 days, suggesting the importance of early surgical intervention. In support of this interpretation, a current meta-analysis [7] and a binational comparative study [8] have demonstrated that early surgical intervention significantly outperformed conservative management in mortality rates in patients with pyogenic spondylodiscitis. As in the case of patients with fractures of the ankylosed spine, the pre-existing frailty of this population of patients, who are typically older and have medical morbidities, is a major obstacle to surgical intervention. To address this issue, the authors used percutaneous techniques including PPS and percutaneous disc lavage in cases of infection, based on our previous experience of percutaneous techniques in trauma cases [9, 10].
This is the second reported case series of ASD-related spinal infections. Early surgical intervention aimed at drainage or stabilization of the infectious focuses may play a more important role in disease control in cases with ASDs than in those without.
The treatment of ankylosed spine infections may be as much challenging as that of ankylosed spine fractures. However, information is scares as only one study to date has addressed this topic, reporting a mortality rate of 62%. Early surgical intervention aimed at drainage or stabilization of the infectious lesions is crucial to disease control and better clinical outcomes in cases with ASDs.
References
- 1.Konopka J, Fogel HA, Diwan A. Inflammatory arthritis. In: Truumees E, Prather H, editors. Orthopaedic Knowledge Update Spine 6. Rosemont, IL: Wolters Kluwer Health; 2022. p. 507-21. [Google Scholar]
- 2.Mader R, Verlaan JJ, Eshed I, Bruges-Armas J, Puttini PS, Atzeni F, et al. Diffuse idiopathic skeletal hyperostosis (DISH): Where we are now and where to go next. RMD Open 2017;3:e000472. [Google Scholar]
- 3.Child ZA, Bransford RJ. Chapter 12. Fractures in ankylosing conditions. In: Vialle LR, Bellabarba C, Kandziora F, editors, AOSpine Masters Series. Vol. 6. Thoracolumbar Spine Trauma. New York: Thieme Medical Publishers, Inc.; 2016. p. 141-51. [Google Scholar]
- 4.Bernstein DN, McCalla DJ, Molinari RW, Rubery PT, Menga EN, Mesfin A. An analysis of patient and fracture characteristics and clinical outcomes in patients with hyperostotic spine fractures. Global Spine J 2020;10:964-72. [Google Scholar]
- 5.Lakomkin N, Mikula AL, Pinter ZW, Wellings E, Alvi MA, Scheitler KM, et al. Perioperative risk stratification of spine trauma patients with ankylosing spinal disorders: A comparison of 3 quantitative indices. J Neurosurg Spine 2022;27:1-7 [Google Scholar]
- 6.Yamada K, Ieguchi M, Takahashi S, Nakamura H. Life expectancy is poor in patients with diffuse idiopathic skeletal hyperostosis-related pyogenic vertebral osteomyelitis. Spine Surg Relat Res 2022;6:654-63. [Google Scholar]
- 7.Thavarajasingam SG, Vemulapalli KV, Vishnu KS, Ponniah HS, Vogel AS, Vardanyan R, et al. Conservative versus early surgical treatment in the management of pyogenic spondylodiscitis: A systematic review and meta-analysis. Sci Rep 2023;13:15647. [Google Scholar]
- 8.Neuhoff J, Kramer A, Jorger AK, Berkulian O, Thavarajasingam SG, Davies BM, et al. Conservative or surgical treatment of pyogenic spinal infection. A retrospective multicenter binational retrospective cohort study. Brain Spine 2023;3:101836. [Google Scholar]
- 9.Fukushi R, Kawaguchi S, Watanabe G, Horigome K, Yajima H, Yamashita T. Repetitive vertebral fractures in patients with ankylosing spinal disorders: A report of two cases. Spine Surg Relat Res 2018;3:188-92. [Google Scholar]
- 10.Fukushi R, Kawaguchi S, Horigome K, Yajima H, Yamashita T. Standalone percutaneous vertebroplasty for hyperextension injuries of the ankylosed thoracolumbar spinal kyphosis. Asian Spine J 2023;17:1132-8. [Google Scholar]