A unicompartmental knee replacement combined with a revision ACL reconstruction is a treatment option in younger patients with higher activity levels.
Miss. Sophia Hashim, Department of Orthopaedics, Charing Cross Hospital, Fulham Palace Road, London, England, United Kingdom. E-mail: sophia.hashim2@nhs.net
Introduction: Failure of anterior cruciate ligament (ACL) reconstructive surgery often presents alongside progressive mono-compartment tibiofemoral arthritis. Total knee arthroplasty (TKA) is the conventional treatment option for this scenario but is associated with high levels of dissatisfaction amongst this younger cohort.
Case Report: This case report outlines a 39-year-old male patient, who underwent revision ACL reconstruction plus a medial unicompartmental knee arthroplasty (UKA) replacement as a single-stage procedure.
Conclusion: This is the first reported ACL revision with a simultaneous medial UKA and provides an alternative solution to a TKA in this younger cohort of patients.
Keywords: Anterior cruciate ligament, unicompartmental knee arthroplasty, partial knee replacement, revision anterior cruciate ligament.
Anterior cruciate ligament (ACL) rupture is a common orthopedic injury, with a 12-fold increase in reconstructions performed in England over the past two decades [1]. The revision rate of primary ACL repairs is also increasing: 4.9% at 8.1 years [2] and 9% at 8 years for repeat revision ACL repairs [3]. Revision ACL reconstructive surgery may be indicated in patients who re-present with instability and high activity levels following another traumatic injury to the reconstructed ACL or atraumatic failure [4]. Patient risk factors for failure include age, level of activity, and gender [5], while surgical risk factors include tunnel malposition, meniscal tears, excessive tibial slope, and use of an allograft [6]. ACL rupture is associated with higher levels of meniscal damage and osteoarthritis in the patellofemoral and tibiofemoral joints. Indeed, the incidence of medial tibiofemoral compartment osteoarthritis following ACL injury is between 33% and 70%, with a tenfold increase in the risk of developing osteoarthritis compared to a matched uninjured population [7, 8]. There is no evidence yet that this risk is reduced following ACL reconstructive surgery. For patients presenting with instability following failure of an ACL reconstruction, together with established full-thickness tibiofemoral compartment osteoarthrosis, a total knee arthroplasty (TKA) is considered the gold standard treatment option. Indeed, the incidence of TKA in patients with ACL reconstruction is 7 times greater at 15-year follow-up than matched controls [9]. Unfortunately, in this younger group of patients, a TKA is associated with significant levels of dissatisfaction and revision rates [10]. Unicompartmental knee arthroplasty (UKA) is an attractive alternative in patients with isolated medial or lateral tibiofemoral compartment osteoarthrosis given that it preserves much of the patient’s bone stock, is associated with a faster recovery, and improves long-term functional results [11, 12]. It is also associated with fewer medical complications and lower mortality [13-15]. A combined UKA and primary ACL reconstruction is a recognized option in patients with unicompartmental tibiofemoral osteoarthritis and instability secondary to ACL rupture, with good results. We propose that this approach remains a viable option for young patients with a failed prior ACL reconstruction.
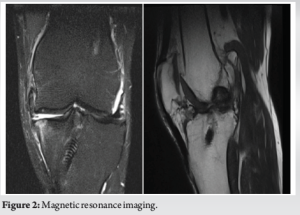
A 39-year-old male was seen in an orthopedic clinic with a background of a left hamstring tendon ACL transtibial primary reconstruction in 2012. He was otherwise fit and well, with no other past medical history, and remained very physically active, having returned to football and long-distance running following his primary ACL surgery. On the contralateral side, in 2019, he also had an ACL reconstruction and a medial partial meniscectomy. At the same time, he reported that his left knee felt unstable, and a rupture of his reconstructed ACL graft was confirmed on an MRI. This was managed non-operatively until the development of activity-related knee pain and intermittent knee swelling, which prompted a referral for a new orthopedic opinion in December 2022. On examination, range of motion was 4–120°, with evidence of quadriceps wasting. There was pain on palpation of the medial tibiofemoral compartment, with palpable osteophytes. There was a varus deformity of 8°, which was partially correctable to 5°. There was no patellofemoral-related pain. The knee was unstable in the sagittal plane, with Lachman and anterior drawer tests in Grade II. Radiographs demonstrated medial tibiofemoral compartment arthrosis, Ahlback grade 3 (i.e., complete loss of joint space with 1–5 mm of bone loss), with anterior subluxation of the tibia secondary to ACL deficiency. Joint space in the lateral and patellofemoral compartments was preserved (Fig. 1). An MRI scan confirmed these findings (Fig. 2).

Management
The treatment options were discussed with the patient, including non-operative management (analgesia, physiotherapy, injections, or an off-loader brace), and operative management, which included a medial UKA with or without ACL reconstruction, or a total knee replacement. On balance, in view of the patient’s young age and high activity level, the patient decided to proceed with a medial fixed-bearing UKA plus revision ACL reconstruction. A medial parapatellar incision was used to access the existing tibial screw, which was removed, and the tunnel was reamed to 8 mm. The femoral screw, which had been placed using a transtibial technique, was difficult to locate, and the operating surgeon elected to retain it. Tibial osteophytes were removed from the anterior tibia and femoral notch. A cementless Smith and Nephew Journey II UK medial partial knee replacement was performed according to the manufacturers’ operative technique. Once the trial implants were in situ, the revision ACL reconstruction was performed under direct vision. A fresh-frozen allograft, 8 mm in diameter when folded, Was prepared under tension using Fibrewire whip sutures, 8 mm in diameter. A new 8 mm femoral tunnel was formed through the anteromedial arthroscopic portal, placed in the 2 o’clock position [16], and reamed to depth. The allograft was then passed and secured on the femoral side with a 20 mm Smith and Nephew closed-loop endobutton. Following graft cycling, tibial fixation was performed using a 10×30 mm Smith and Nephew RCI interference screw plus a staple. The final medial partial knee replacement components were then cemented in situ, and the wound was closed in a standard manner. Full range of motion and weight-bearing were permitted in a hinged-knee brace immediately post-operatively, with a standard physiotherapy-led ACL rehabilitation protocol on discharge from the hospital.
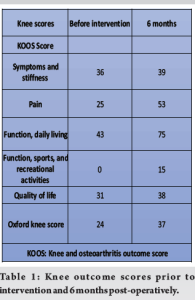
Knee and osteoarthritis outcome scores and Oxford Knee Scores were collected pre-operatively, and at 6 months post-operatively, and can be seen in Table 1. On clinical review at 6 months, the patient reported that his knee was pain free during daily activities with no symptoms of instability. The range of motion was 0–125°, Lachman’s 3 mm, with a negative pivot shift. The post-operative radiograph can be seen in Fig. 3. A return to football is expected 1 year post-operatively (Table 1).

Combined ACL reconstruction and partial knee replacement have been reported in the literature [17], with good outcomes [18, 19]. However, this is the first report of a partial knee replacement being performed together with a revision ACL reconstruction. The patient has made an excellent recovery, and it highlights that this combined procedure remains an option for young patients with high exercise demands, even in the setting of a failed prior ACL reconstruction. Compared to the alternative of a total knee replacement, the procedure is bone conserving, and associated with a number of benefits: faster recovery, fewer complications, lower mortality, and improved longer-term functional benefits. As is the case with all ACL revision surgery, it is important to identify the cause of failure [20], and in this particular case, a transtibial femoral tunnel was performed during the primary ACL reconstruction, and this was changed to a more anatomic tunnel position using the anteromedial portal technique [21].
This case report illustrates the use of a revision ACL reconstruction combined with a medial unicompartmental knee replacement, resulting in good post-operative outcomes.
A unicompartmental knee replacement combined with a revision ACL reconstruction is a treatment option for younger patients with higher activity levels.
References
- 1.Abram SG, Price AJ, Judge A, Beard DJ. Anterior cruciate ligament (ACL) reconstruction and meniscal repair rates have both increased in the past 20 years in England: Hospital statistics from 1997 to 2017. Br J Sports Med 2020;54:286-91. [Google Scholar]
- 2.Martin RK, Wastvedt S, Pareek A, Persson A, Visnes H, Fenstad AM. Predicting anterior cruciate ligament reconstruction revision: A machine learning analysis utilizing the Norwegian knee ligament register. J Bone Joint Surg 2022;104:145-53. [Google Scholar]
- 3.Vap AR, Persson A, Fenstad AM, Moatshe G, LaPrade RF, Engebretsen L. Re-revision anterior cruciate ligament reconstruction: An evaluation from the norwegian knee ligament registry. Arthroscopy 2019;35:1695-701. [Google Scholar]
- 4.Chen JL, Allen CR, Stephens TE, Haas AK, Huston LJ, Wright RW, et al. Differences in mechanisms of failure, intraoperative findings, and surgical characteristics between single-and multiple-revision ACL reconstructions: A MARS cohort study. Am J Sports Med 2013;41:1571-8. [Google Scholar]
- 5.Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, MOON Consortium, Spindler KP. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: Prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med 2015;43:1583-90. [Google Scholar]
- 6.Morgan JA, Dahm D, Levy B, Stuart MJ, MARS Study Group. Femoral tunnel malposition in ACL revision reconstruction. J Knee Surg 2012;25:361-8. [Google Scholar]
- 7.Gillquist J, Messner K. Anterior cruciate ligament reconstruction and the long-term incidence of gonarthrosis. Sports Med 1999;27:143-56. [Google Scholar]
- 8.McDaniel WJ Jr., Dameron TB Jr. The untreated anterior cruciate ligament rupture. Clin Orthop 1983;172:158-63. [Google Scholar]
- 9.Leroux T, Ogilvie-Harris D, Dwyer T, Chahal J, Gandhi R, Mahomed N, et al. The risk of knee arthroplasty following cruciate ligament reconstruction: A population-based matched cohort study. J Bone Joint Surg Am 2014;96:2-10. [Google Scholar]
- 10.Price AJ, Longino D, Rees J, Rout R, Pandit H, Javaid K, et al. Are pain and function better measures of outcome than revision rates after TKR in the younger patient? Knee 2010;17:196-9. [Google Scholar]
- 11.Ghomrawi HM, Eggman AA, Pearle AD. Effect of age on cost-effectiveness of unicompartmental knee arthroplasty compared with total knee arthroplasty in the U.S. J Bone Joint Surg Am 2015;97:396-402. [Google Scholar]
- 12.Jones GG, Kotti M, Wiik AV, Collins R, Brevadt MJ, Strachan RK, et al. Gait comparison of unicompartmental and total knee arthroplasties with healthy controls. Bone Joint J 2016;98 (10 Supp B):16-21. [Google Scholar]
- 13.Burn E, Liddle AD, Hamilton TW, Judge A, Pandit HG, Murray DW, et al. Cost-effectiveness of unicompartmental compared with total knee replacement: A population-based study using data from the National Joint Registry for England and Wales. BMJ Open 2018;8:e020977. [Google Scholar]
- 14.Willis-Owen CA, Brust K, Alsop H, Miraldo M, Cobb JP. Unicondylar knee arthroplasty in the UK National health service: An analysis of candidacy, outcome and cost efficacy. Knee 2009;16:473-8. [Google Scholar]
- 15.Liddle AD, Judge A, Pandit H, Murray DW. Adverse outcomes after total and unicompartmental knee replacement in 101, 330 matched patients: A study of data from the National Joint Registry for England and Wales. Lancet 2014;384:1437-45. Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty: A ten-year survival study. J Bone Joint Surg Br 1998;80:983-9. [Google Scholar]
- 16.Edwards A, Bull AM, Amis AA. The attachments of the anteromedial and posterolateral fibre bundles of the anterior cruciate ligament: Part 2: Femoral attachment. Knee Surg Sports Traumatol Arthrosc 2008;16:29-36. [Google Scholar]
- 17.Volpin A, Kini SG, Meuffels DE. Satisfactory outcomes following combined unicompartmental knee replacement and anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2018;26:2594-601. [Google Scholar]
- 18.Ventura A, Legnani C, Terzaghi C, Macchi V, Borgo E. Unicompartmental knee replacement combined to anterior cruciate ligament reconstruction: Midterm results. J Knee Surg 2019;33:1152-6. [Google Scholar]
- 19.Weston-Simons JS, Pandit H, Jenkins C, Jackson WF, Price AJ, Gill HS, et al. Outcome of combined unicompartmental knee replacement and combined or sequential anterior cruciate ligament reconstruction: A study of 52 cases with mean follow-up of five years. J Bone Joint Surg Br 2012;94:1216-20. [Google Scholar]
- 20.Samitier G, Marcano AI, Alentorn-Geli E, Cugat R, Farmer KW, Moser MW. Failure of anterior cruciate ligament reconstruction. Arch Bone Joint Surg 2015;3:220. [Google Scholar]
- 21.Bird JH, Carmont MR, Dhillon M, Smith N, Brown C, Thompson P, et al. Validation of a new technique to determine midbundle femoral tunnel position in anterior cruciate ligament reconstruction using 3-dimensional computed tomography analysis. Arthroscopy 2011;27:1259-67. [Google Scholar]