The first metatarsal pronation rotation deformity of hallux valgus feet may be corrected without osteotomy or arthrodesis.
Dr. Daniel Yiang Wu, Department of Orthopaedic Surgery, Hong Kong Adventist Hospital, #40 Stubbs Rd, Hong Kong, SAR, China. E-mail: dymjwu@gmail.com
Introduction: If not corrected, the first metatarsal pronation rotation deformity is deemed responsible for the high hallux valgus (HV) deformity recurrence rate. Its correction method by osteotomy and arthrodesis has been recommended, just like the metatarsus primus varus (MPV) deformity correction. Since the pathogenesis of the first metatarsal pronation is not well understood, there may be other surgical approaches to correct it.
Case Report: A 53-year-old female’s HV feet presented with severe left hallux pronation, and positive radiological round head and inferior tubercle shift signs of the first metatarsal. She underwent a non-osteotomy non-arthrodesis soft-tissue procedure that was expected to correct the MPV deformity but not the pronation deformity. Post-operative hallux pronation was reversed, and round head and inferior tubercle signs were corrected.
Conclusion: The first metatarsal hypermobility and displacement of HV feet are probably in all three planes. Correction of MPV in the first metatarsal entirety in the transverse plane without osteotomy or arthrodesis can also induce a correction effect on its sagittal and frontal planes.
Keywords: Hallux valgus, metatarsus primus varus, pronation, syndesmosis procedure.
The first metatarsal instability and displacement are the well-known underlying causes of the valgus [1] and pronation deformities of the great toe [2]. It is a three-dimensional displacement happening simultaneously in transverse, sagittal, and frontal planes [3]. Their surgical corrections are equally important, although the pronation rotation displacement in the frontal plane has only been receiving more attention lately. Incorporation of rotational correction into osteotomy [4] and arthrodesis [5] procedures is presently strongly advocated in addition to sagittal and transverse plane corrections. However, what soft-tissue procedures can do to induce a derotation effect on the first metatarsal and also correct the metatarsus primus varus (MPV) deformity in the transverse plane is unknown. The syndesmosis procedure is a non-osteotomy non-arthrodesis soft-tissue procedure designed to correct the MPV deformity simply with 1–2 intermetatarsal cerclage sutures [6]. Its effects on the sagittal and frontal planes are still unclear. This case report was to share an unexpected observation that a soft-tissue realignment of the first metatarsal could spontaneously correct the pronation deformity of the first metatarsal. Similarly, the hallux pronation deformity could also be spontaneously corrected after the realignment of the first metatarsal by the 1–2 intermetatarsal cerclage sutures.
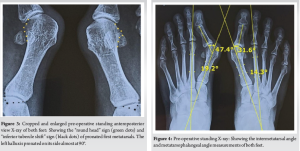
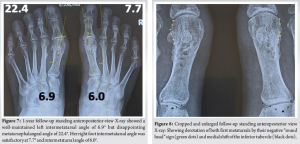
A 53-year-old woman with bilateral hallux valgus (HV) deformity complained of bunion pain, metatarsalgia, and spasms of the left second toe in walking. She noticed her balance was getting poorer and had to be very cautious in walking downstairs lest she lost her balance and fall. There was no history of rheumatoid arthritis. Her left big toe had obvious pronation deformity (Fig. 1), and her first metatarsals were hypermobile in transverse and sagittal planes. There were also mid-metatarsal calluses (Fig. 2). Standing anteroposterior (AP) X-ray of her feet revealed obvious rotational deformity of her left hallux lying on its side (Fig. 3 and 4). Both her feet had the positive round head sign for first metatarsal pronation according to Yamaguchi’s lateral edge shape of the first metatarsal head [7] and Eustace’s inferior tubercle shift sign [8] (Fig. 3). Her right hallux was not pronated because its lateral sesamoid had not turned around the lateral side of the metatarsal head. Her left foot metatarsophalangeal angle (MPA) was 47.4°, and intermetatarsal angle (IMA) was 19.2°. They were 31.6 and 14.3°, respectively, on her right foot (Fig. 4), all by Hardy’s mid-axial method [9].
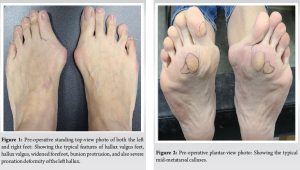
A straight 2-cm dorsal incision was made to expose the distal first intermetatarsal space. The contracted distal lateral soft tissues were released with an inverted “T” incision. The horizontal incision released the metatarsosesamoid ligament to facilitate fibula sesamoid realignment, and the vertical incision released the lateral collateral ligament of the metatarsophalangeal joint to facilitate hallux realignment. However, the adductor hallucis tendons were not released to prevent hallux varus complication. Four 2-mm drill holes were made in the distal half of the first metatarsal. Two double-strand no. 2 absorbable PDS and two 2-O non-absorbable Ethibond sutures were passed through drill holes and around the second metatarsal. They were tied with moderate compression force after the opposing cortices of the distal half of the first and second metatarsals were scarified in a fish-scale fashion with an osteotome. Through a medial incision, all feet had their redundant medial skin and capsuloligamentous tissues over the bunion protuberance excised along with exostectomy of the bunion. She was allowed and could walk with full weight-bearing on her 1st post-operative day but was limited to <5000 steps a day. A forefoot cast was applied on the 10th post-operative day for 3 months. She was allowed to walk back to normal, but no running and hiking until after the first 6 post-operative months. At her final 1-year post-operative examination, she had not had bunion pain since her surgery, and her balance was markedly improved. A photograph of her feet in standing revealed correction of hallux pronation satisfactorily (Fig. 5). Her mid-metatarsal calluses had disappeared (Fig. 6), and the first metatarsal was stable in the transverse and sagittal planes on examination. She was extremely pleased with her feet’ function being restored. Her standing AP X-rays showed a left foot MPA of 22.4° which was above the desired MPA of <15° although the IMA was 6.9° and within the normal upper range of 9°. Her right foot MPA was 7.7°, and IMA was 6.0° (Fig. 7). The slight right hallux varus appearance was not evident by X-ray examination. The radiological round head signs of both her first metatarsals were reduced to angular shape, and the inferior tubercles had shifted from 20° pronation preoperatively of both her first metatarsals to 0° and 5° of her left and right foot, respectively (Fig. 8), according to Eustace’s definition [8]. The left hallux radiological pronation was also corrected (Fig. 8).

The pathogenesis of the first metatarsal pronation rotation of HV feet is still unclear [10]. Although destabilization and hypermobility may allow the first metatarsal displaced in sagittal and transverse planes, how it can be rotated is less understood. However, Ota et al. found a pronation force on full-weight-bearing of the first metatarsal in normal feet [11] and, thus, the pronation displacement of an unstable first metatarsal. Pronation of the first metatarsal can then precipitate pronation displacement of the lateral sesamoid and also the hallux through the displaced flexor hallucis brevis. How to correct it and maintain the correction has been reported with metatarsocuneiform fusion [5] and first metatarsal osteotomy [4] procedures. This case report demonstrated for the first time in literature that a simple MPV correction by a soft-tissue technique, the syndesmosis procedure, without osteotomy or arthrodesis, could also spontaneously reverse its pronation deformity. Its derotation also helped in the derotation of the lateral sesamoid and hallux. A long-term study of the syndesmosis procedure after an average of 8.4 years up to 14 years [6] has shown that it can satisfactorily realign the displaced first metatarsal with 1–2 intermetatarsal cerclage sutures from an average pre-operative IMA of 14.3° and also maintain it with the primary formation of a 1–2 intermetatarsal syndesmotic bonding to 6.7°. Our 1-year follow-up of the case demonstrated the first metatarsal MPV and pronation deformities correction could be satisfactorily maintained without any sign of either deformity recurrence. The first metatarsal pronation deformity has been described as intrinsic or extrinsic in origin. Osteotomy procedures are most suitable for intrinsic pronation correction and metatarsocuneiform derotational fusion for an extrinsic deformity. However, the soft-tissue syndesmosis procedure can only be expected to correct extrinsic rotation deformities. We will need future studies to understand and confirm this positive effect as to why a non-osteotomy non-arthrodesis MPV correction could de-rotate the first metatarsal.
It is possible that the first metatarsal instability and displacement of HV feet in all three planes are interrelated, and thus, correction in one plane can spontaneously correct alignment in the other two planes.
The syndesmosis procedure can correct the hallux and first metatarsal pronation deformity of HV feet and prevent recurrence without osteotomy and arthrodesis.
References
- 1.Myerson MS, Badekas A. Hypermobility of the first ray. Foot Ankle Clin 2000;5:469-84. [Google Scholar]
- 2.Dayton P, Kauwe M, Feilmeier M. Is our current paradigm for evaluation and management of the bunion deformity flawed? A discussion of procedure philosophy relative to anatomy. J Foot Ankle Surg 2015;54:102-11. [Google Scholar]
- 3.Najefi AA, Katmeh R, Zaveri AK, Alsafi MK, Garrick F, Malhotra K, et al. Imaging findings and first metatarsal rotation in hallux valgus. Foot Ankle Int 2022;43:665-75. [Google Scholar]
- 4.Yasuda T, Okuda R, Jotoku T, Shima H, Hida T, Neo M. Proximal supination osteotomy of the first metatarsal for hallux valgus. Foot Ankle Int 2015;36:696-704. [Google Scholar]
- 5.Dayton P, Carvalho S, Egdorf R, Dayton M. Comparison of radiographic measurements before and after triplane tarsometatarsal arthrodesis for hallux valgus. J Foot Ankle Surg 2020;59:291-7. [Google Scholar]
- 6.Wu DY, Lam EK. Radiological analysis of the syndesmosis concept in metatarsus primus varus and hallux valgus deformities recurrence prevention. J Foot Ankle Surg 2024;63:262-6. [Google Scholar]
- 7.Yamaguchi S, Sasho T, Endo J, Yamamoto Y, Akagi R, Sato Y, et al. Shape of the lateral edge of the first metatarsal head changes depending on the rotation and inclination of the first metatarsal: A study using digitally reconstructed radiographs. J Orthop Sci 2015;20:868-74. [Google Scholar]
- 8.Eustace S, O’Byrne J, Stack J, Stephens MM. Radiographic features that enable assessment of first metatarsal rotation: The role of pronation in hallux valgus. Skeletal Radiol 1993;22:153-6. [Google Scholar]
- 9.Hardy RH, Clapham JC. Observations on hallux valgus; Based on a controlled series. J Bone Joint Surg Br 1951;33B:376-91. [Google Scholar]
- 10.Lalevée M, Mansur NS, Dibbern K, Briggs H, Maly CJ, Mendes de Carvalho KA, et al. Coronal plane rotation of the medial column in hallux valgus: A retrospective case-control study. Foot Ankle Int 2022;43:1041-8. [Google Scholar]
- 11.Ota T, Nagura T, Yamada Y, Yamada M, Yokoyama Y, Ogihara N, et al. Effect of natural full weight-bearing during standing on the rotation of the first metatarsal bone. Clin Anat 2019;32:715-21. [Google Scholar]