The challenge of diagnosing and managing of an uncommon fracture in children to avoid fonctionnal complications.
Dr. Amine El Khassoui, Department of Pediatric Orthopedic, Mother and Child Unit, University Hospital Mohamed VI of Marrakech, Faculty of Medecine and Pharmacy, Cadi Ayyad University, Marrakech, Morocco. E-mail: a.elkhassoui@uca.ma
Introduction: Hoffa fractures are uncommon fractures in adults and less common in children. They are defined as fractures of the femoral condyles that occur in the coronal planes. To this day, Hoffa fractures in children comprise only of case reports.
Case Report: Our case report is focused on a 12-year-old patient victim of a high-impact trauma causing a bicondylar Hoffa fracture. The diagnosis was based on an X-ray in front and lateral views and confirmed by a computed tomography scan and 3D reconstructions. A screw fixation truth open reduction with a lateral approach. We report the satisfactory results of our case after a 24-month follow-up with a good range of motion.
Conclusion: To avoid necrosis of the fragment, pain and stiffness at long-term follow-up make the management of this fracture a serious challenge, and in the pediatric population, the prevention of growth cartilage injuries is crucial to accurate management.
Keywords: Hoffa fracture, children, bicondylar, open reduction, rehabilitation.
Hoffa fractures are uncommon fractures in children. It is defined as fractures of the femoral condyles that occur in the coronal planes, unlike the sagittal plane fractures that are the most frequent. Mr. Hoffa first defined this fracture in 1904 [1]. On the day of writing this article, Hoffa fractures in children counted a few case reports in the literature. We report the case of a 12-year-old boy victim of high-impact trauma causing a bicondylar Hoffa fracture.
It is about a 12-year-old boy who presented to the emergency department with swelling of the left knee caused by a high-impact trauma. The patient was the victim, 3 h before his admission, of two motorcycle collisions with a flexed knee. The physical examination found a swollen knee and a few dermabrasions. There was tenderness over the lower end of the femur, and no movements of the left knee were possible. No neurovascular deficit in the affected limb and any other injuries in the rest of the physical examination were noted. The immediate treatment was immobilization with a knee posterior slab, and an X-ray associated with a computed tomography (CT) scan was then performed. On the anteroposterior and lateral X-rays of the knee, it was a bicondylar coronal plane fracture (Fig. 1). A CT scan with 3D reconstruction showed a sagittal bicondylar fracture of the left limb with a posterior displacement of the distal fragment associated with the dissociation of a small bone fragment inside the articulation. The fracture was classified as Letenneur type II (Fig. 2). Once the diagnosis has been made, the surgery schedule has been established. Since it is a bycondylar fracture, the choice between a medial or lateral approach of the knee was discussed, and we opted for a lateral approach given that the largest fragment on the scan images was the lateral condyl, which could allow us to have a more solid fixation. An open surgery has been decided with internal fixation, using an image intensifier, and on a plane orthopedic table without traction. The reduction was established and maintained with two 4 mm partially threaded cancellous screws to assure a satisfactory reduction; the screws were introduced in an anteroposterior direction, and with the distal thread allowing impact on the fracture site. We could not avoid going through the physis for better stability of the reduction (Fig. 3), then the knee was immobilized by a cast in 10° flexion. The immobilization was kept for 4 weeks and followed by progressive physiotherapy. Weight-bearing was allowed at 8 weeks. The 1-year follow-up showed a good range of motion of the left knee at 90°, absence of laxity, and absence of pain (Fig. 4). At 24-month follow-up, the flexion of the knee reached 110°, and no discomfort during daytime activities was noted. Given the age of our patient, we are considering that the screws can be removed after the closure of the growth plate if the patient presents implant-related symptoms, to avoid further damage during the removal.

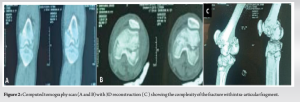
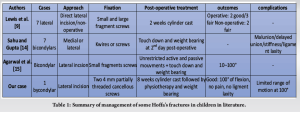
Hoffa fractures are uncommon in the distal femoral; it represents <1% of cases [2-5], and it was described by Hoffa for the 1st time in 1904 [6]. This fracture is often uni-condylar; the bi-condylar variety is rarer, especially in children. These fractures are mostly resulting from direct high-energy trauma, which causes a shear force on the posterior femoral condyle. The usual cause of Hoffa’s fracture is motorcycle accidents [7]. When a Hoffa fracture is suspected, an X-ray must be planned first, and for better evaluation of the lesion, a CT scan must be performed or sometimes even magnetic resonance imaging. Letenneur et al. [2] provided a classification with three types of fracture: Type I is a vertical fracture involving the entire condyle parallel to the posterior cortex of the femur. Type II is a fracture of variable size, horizontal to the base of the condyle. Type III is a fracture oblique to the femur and has the worst results. Surgical treatment is the reference to recover anatomic articular surfaces; open reduction associated with internal fixation using screws seems almost necessary given the absence of a soft tissue ensuring fixity at the level of the femoral condyles or when other injuries are associated as the extensor system considering mechanism [8]. A variety of techniques have been discussed in the literature, and according to the location and type of the fracture, a surgical approach can be chosen. Many studies have utilized a general lateral or medial parapatellar incision to access the anterior femur [9, 10]. The less frequently reported arthroscopic approach for the treatment of Hoffa fractures is one of the least invasive approaches. It is beneficial for acute Hoffa’s fractures with large fragments and minimal communication [11]. It minimizes soft-tissue damage, blood loss, infection rate, and operative time [12]. The few studies that used a non-operative approach reported both successful and unsuccessful results [13]. Post-operative outcomes depend on the severity of the injury, the technical approach, and fixation, and they also depend on early mobilization, which is encouraged by most studies to stimulate bone healing and avoid joint stiffness [1]. Some reports allowed weight bearing 2-day postoperatively; however, most preferred a more slowly progressive approach. A summary of some of the cases described in the literature [9, 14, 15] and differences in management, results, and complications between bicondylar and unicondylar Hoffa fractures is presented in Table 1.
The challenge with Hoffa fractures in children is to make an early diagnosis to make a good choice of treatment; this one has the objectives of establishing the articular anatomy to avoid necrosis of the fragment, growth cartilage injuries, pain, and stiffness at long-term follow-up.
The challenge in managing a Hoffa fracture is based on an accurate diagnosis based on X-rays and 3D CT scans.
References
- 1.Patel PB, Tejwani NC. The Hoffa fracture: Coronal fracture of the femoral condyle a review of literature. J Orthop 2018;15:726-31. [Google Scholar]
- 2.Letenneur J, Labour PE, Rogez JM, Lignon J, Bainvel JV. Hoffa’s fractures. Report of 20 cases. Ann Chir 1979;32:213-9. [Google Scholar]
- 3.Payne R, Clark D, Wall S. Union after delayed presentation of a Hoffa fracture. Injury Extra 2005;36:289-91. [Google Scholar]
- 4.Somford MP, van Ooij B, Schafroth MU, Kloen P. Hoffa nonunion, two cases treated with headless compression screws. J Knee Surg 2013;26:S89-93. [Google Scholar]
- 5.Bartonícek J, Rammelt S. History of femoral head fracture and coronal fracture of the femoral condyles. Int Orthop 2015;39:1245-50. [Google Scholar]
- 6.Ul Haq R, Modi P, Dhammi IK, Jain AK, Mishra P. Conjoint bicondylar Hoffa fracture in an adult. Indian J Orthop 2013;47:302-6. [Google Scholar]
- 7.AlKhalife YI, Alshammari AN, Abouelnaga MA. Hoffa’s fracture of the medial femoral condyle in a child treated with open reduction and internal fixation: A case report. Trauma Case Rep 2018;14:20-6. [Google Scholar]
- 8.Julfiqar, Huda N, Pant A. Paediatric conjoint bicondylar Hoffa fracture with patellar tendon injury: An unusual pattern of injury. Chin J Traumatol 2019;22:246-8. [Google Scholar]
- 9.Lewis SL, Pozo JL, Muirhead-Allwood WF. Coronal fractures of the lateral femoral condyle. J Bone Joint Surg Br 1989;71:118-20. [Google Scholar]
- 10.Holmes SM, Bomback D, Baumgaertner MR. Coronal fractures of the femoral condyle: A brief report of five cases. J Orthop Trauma 2004;18:316-9. [Google Scholar]
- 11.Harna B, Goel A, Singh P, Sabat D. Pediatric conjoint Hoffa’s fracture: An uncommon injury and review of literature. J Clin Orthop Trauma 2017;8:353-4. [Google Scholar]
- 12.Lal H, Bansal P, Khare R, Mittal D. Conjoint bicondylar Hoffa fracture in a child: A rare variant treated by minimally invasive approach. J Orthop Traumatol 2011;12:111-4. [Google Scholar]
- 13.Nork S, Segina D, Aflatoon K, Barei DP, Bradford Henley M, Holt S, et al. The association between supracondylar-intercondylar distal femoral fractures and coronal plane fractures. J Bone Joint Surg Am 2005;87:564-9. [Google Scholar]
- 14.Sahu RL, Gupta P. Operative management of Hoffa fracture of the femoral condyle. Acta Med Iran 2014;52:443-7. [Google Scholar]
- 15.Agarwal S, Giannoudis PV, Smith RM. Cruciate fracture of the distal femur: The double Hoffa fracture. Injury 2004;35:828-30. [Google Scholar]