Successful fracture union and restoration of functional movement after a large femoral segmental bone loss may be obtained after the first stage of the Masqulet technique without bone grafting in select cases.
Miss. Megan Tersteeg, Saint Louis University School of Medicine, St. Louis, Missouri, United States. E-mail: megan.tersteeg@health.slu.edu
Introduction: The masquelet technique is a two-stage procedure used by orthopedic surgeons to treat large segmental bone defects secondary to infection, trauma, and tumor resection. This technique characteristically requires the placement of a temporary cement spacer and subsequent bone grafting for complete reconstruction. We describe a unique case of segmental bone loss reconstruction in which a patient successfully achieved fracture union after the first step of the masquelet technique without bone grafting.
Case Report: This is a case of a 21-year-old male who presented with an open femur fracture with 10 cm of segmental bone loss after a motorcycle collision. An antibiotic cement spacer was inserted according to the first stage of the masquelet technique. Due to considerable callus formation around the spacer, normal alignment, and pain-free ambulation at follow-up, further surgical intervention was not pursued, and the poly-methyl-methacrylate spacer was left in place. The fracture healed without infection, and the patient remained weight-bearing without pain.
Conclusion: This case identifies a unique instance of successful fracture union of a 10 cm segmental bone defect despite the completion of only the first step in the masquelet procedure. While the masquelet technique is believed to be a mandatory two-step procedure, this unique case of rapid bone growth and fracture union warrants further research on the possibilities of masquelet-induced regeneration without bone grafting.
Keywords: Masquelet technique, segmental bone loss, cement spacer, fracture.
The masquelet technique, also known as the induced membrane technique, is a procedure used by orthopedic surgeons to treat segmental bone defects, typically in the femur and tibia [1]. This technique utilizes a two-stage process in which, after definitive debridement, surgeons insert a custom cement spacer into the site of segmental bone loss [1, 2]. This spacer, most often bone cement or poly-methyl methacrylate (PMMA), is designed to act as a void filler and scaffold, inducing the development of a biologically active membrane during the early healing process [1-4]. The spacer is usually left in place for an average of 6–8 weeks to allow for the bioactive membrane to mature, setting the stage for the subsequent bone grafting procedure to promote fracture union [1]. This involves the removal of the cement spacer, with preservation of the bioactive membrane, and subsequent autologous bone grafting. The theory is that the autologous bone graft within the bioactive membrane will stimulate de novo bone formation [1]. The masquelet procedure is still a relatively new surgical technique and has a history of various complications, including superficial or deep surgical site infections [3]. In this case report, we highlight a unique instance in which a patient successfully achieved fracture union after the first step of the masquelet technique that did not require the second stage, leaving the cement spacer in place.
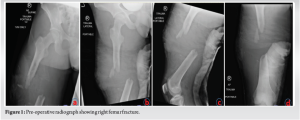
A 21-year-old male with a history of mild scoliosis, no previous fractures, and daily smoking for 2 years sustained multiple musculoskeletal injuries after a motorcycle collision. The injuries included a closed left femoral shaft injury and an open right Gutstilo and Anderson Type III A femur fracture with 10 cm of segmental bone loss (Fig. 1). On the night of the injury, the patient underwent emergent irrigation, debridement, and temporary stabilization of his fracture with external fixation. Tobramycin antibiotic cement with vancomycin powder was placed within the thigh wound with a negative-pressure wound vacuum to cover the wound.
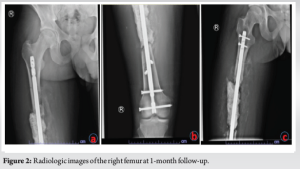
2 days later, once resuscitated, the right femur underwent another irrigation and debridement with an antibiotic bead and wound vacuum exchange. After multiple irrigation and debridement procedures of the lower extremity, the wound bed was amenable to definitive fixation of the femur. On day 5, the femur underwent intramedullary retrograde nailing with the placement of two proximal and two distal interlocking screws, revealing a 10-cm segmental bone defect. The defect was filled with tobramycin antibiotic cement mixed with vancomycin powder and underwent delayed primary wound closure. This was the first stage of a proposed masquelet technique treatment plan for this injury. He was made non-weight-bearing in his right lower extremity due to additional ipsilateral musculoskeletal injuries, but the patient was encouraged to range the knee from 0° extension to 140° flexion as often as possible. The remainder of his musculoskeletal injuries eventually underwent definitive fixation, with subsequent discharge to a rehabilitation center on hospital day 13. The patient was seen in clinic 1 month after his initial injury, at which time he was non-weight-bearing in his right lower extremity and receiving outpatient physical therapy. His X-rays demonstrated unchanged osseous alignment with early callus formation (Fig. 2). He was made to be a weight-bearing as tolerated and continued his home exercise program to improve his knee and ankle range of motion (ROM) until his subsequent follow-up.
At the 8-week follow-up visit, the patient’s pain was well controlled, and he was weight-bearing as tolerated on the right lower extremity up to his full bodyweight of 65.8 kg. There were no signs of infection, and his X-rays at the time showed abundant callus formation bridging the fracture site around the cement spacer (Fig. 3). At this time, the second stage of the masquelet technique with bone grafting was considered. However, due to significant callus formation and minimal pain with ambulation, the decision was made to continue to monitor his progress and reevaluate at his next visit.
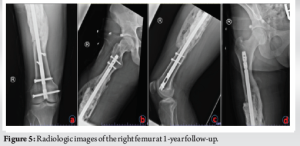
Six-month post-injury, he was weight-bearing without assistive devices, without any gait abnormalities, and with no pain. Radiographs revealed the interval progression of callus formation (Fig. 4). At the last follow-up, 1 year after definitive fixation, the patient reported no complaints regarding his right lower extremity. He had full ROM of knees, a normal, non-antalgic gait, and had fully returned to work in construction. Radiographs demonstrated bridging callus formation in three out of four cortices and unchanged alignment (Fig. 5). The patient was subsequently lost to follow-up due to incarceration.

The Masquelet technique is a two-stage procedure to treat critical bone defects and promote union. The bone defect is filled with a spacer, such as PMMA or cement, which serves as a void filler but, by inducing an inflammatory response with white blood cells and edema, stimulates the development of a bioactive membrane to form around the cement, thereby providing a scaffold for future de novo bone growth [1-5]. The spacer is left in place for 6–8 weeks to allow for the inflammatory reaction to develop and the bioactive membrane to mature. At the second stage, the membrane is incised, the spacer is removed, and the cavity is filled with an autologous bone graft [1]. The bone graft placed within the bioactive membrane has good stem cell and vascular activity, which promotes the recruitment of endogenous growth factors in an attempt to simulate de novo bone growth and achieve fracture union [1]. However, our patient presented with rapid callus formation around the spacer, which negated the need for the proposed second stage. In this case, the patient’s fracture healing was robust and encased the cement space, bridging the fracture gap. This amount of bone growth around the spacer was unexpected due to factors such as the patient’s smoking history and the size of the critical bone defect. While the reason for this growth is not clear, it may have occurred due to changes in signaling factors around the site of injury within the soft tissues that increased bone remodeling. It can be hypothesized that it may be a result of the femur’s significant muscle mass providing a soft-tissue envelope with an excellent blood supply [6, 7]. Alternative treatment options for segmental bone defects include vascularized autologous bone grafting, distraction osteogenesis, and bone graft substitutes. Further research into the indications for each of these options is warranted; however, it has been suggested that an induced membrane has improved therapeutic effects over distraction osteogenesis in the setting of larger segmental bone defects [8], as is the case here. It is worthwhile to note that the masquelet technique was originally described for the treatment of osteomyelitis [2, 5]. Therefore, especially in cases of infection, two stages were nearly always necessary to remove all contaminated tissues and facilitate infection treatment [2]. Now, however, considering that masquelet is not only used for cases of infection, considerable efforts have been made to streamline the process to make it applicable for various other orthopedic pathologies [1, 9]. Such is the case here, where, in light of this patient’s remarkable bone growth around the spacer, the decision was made to permanently leave the spacer in and to forgo the secondary procedure. A wide array of studies have been conducted in an attempt to improve upon the masquelet technique in general, including experimentation with different spacer materials, but it is currently unclear if leaving the cement spacer in place has any long-term implications [1, 6, 9, 10]. The possibility certainly exists though to allow future patients to also undergo a one-step procedure, as research has even shown that using a biodegradable spacer such as calcium sulfate encourages the formation of a membrane and creates a one-stage reconstruction of bone defects [11]. This does not mean to advocate for the replication of single-stage masquelet, but rather to appreciate the unique circumstances, such as this case, in which such accelerated union was achieved without bone grafting and retention of cement spacer.
This case identifies a unique instance of successful fracture union of a 10-cm segmental bone defect despite the completion of only the first step in the masquelet procedure. This warrants further research on the mechanisms behind masquelet-induced regeneration without bone grafting and consideration of circumstances in which fracture union can be obtained following stage one of the masquelet procedures.
Masquelet is a useful technique for the reconstruction of large segmental bone loss defects. In select circumstances, considerations could be made regarding the use of a single-stage procedure for fracture union without bone grafting.
References
- 1.Alford AI, Nicolaou D, Hake M, McBride-Gayi S. Masquelet’s induced membrane technique: Review of current concepts and future directions. J Orthop Res 2021;39:707-18. [Google Scholar]
- 2.Chadayammuri V, Hake M, Mauffrey C. Innovative strategies for the management of long bone infection: A review of the Masquelet technique. Patient Saf Surg 2015;9:32. [Google Scholar]
- 3.McBride-Gagyi S, Toth Z, Kim D, Ip V, Evans E, Watson JT, et al. Altering spacer material affects bone regeneration in the Masquelet technique in a rat femoral defect. J Orthop Res 2018;36:2228-38. [Google Scholar]
- 4.Shen Z, Lin H, Chen G, Zhang Y, Li Z, Li D, et al. Comparison between the induced membrane technique and distraction osteogenesis in treating segmental bone defects: An experimental study in a rat model. PLoS One 2019;14:e0226839. [Google Scholar]
- 5.Morelli I, Drago L, George DA, Gallazzi E, Scarponi S, Romano CL. Masquelet technique: Myth or reality? A systematic review and meta-analysis. Injury 2016;47:S68-76. [Google Scholar]
- 6.Klein C, Monet M, Barbie V, Vanlaeys A, Masquelet A, Gouron R, et al. The Masquelet technique: Current concepts, animal models, and perspectives. J Tissue Eng Regen Med 2020;14:1349-59. [Google Scholar]
- 7.Ley P, Gosselin R, Villar R. The Masquelet induced-membrane technique: An option for a tertiary-referral conflict setting. J Surg Case Rep 2019;2019:rjz149. [Google Scholar]
- 8.Toth Z, Roi M, Evans E, Watson J, Nicolaou D, McBride-Gagyi S. Masquelet technique: Effects of spacer material and micro-topography on factor expression and bone regeneration. Ann Biomed Eng 2018;1:174-89. [Google Scholar]
- 9.Jiang N, Qin C, Ma Y, Wang L, Yu B. Possibility of one-stage surgery to reconstruct bone defects using the modified Masquelet technique with degradable calcium sulfate as a cement spacer: A case report and hypothesis. Biomed Rep 2016;4:374-8. [Google Scholar]
- 10.Gaio N, Martino A, Toth Z, Watson JT, Nicolaou D, McBride-Gagyi S. Masquelet technique: The effect of altering implant material and topography on membrane matrix composition, mechanical and barrier properties in a rat defect model. J Biomech 2018;72:53-62. [Google Scholar]
- 11.Hoit G, Kain MS, Sparkman JW, Norris BL, Conway JD, Watson JT, et al. The induced membrane technique for bone defects: Basic science, clinical evidence, and technical tips. OTA Int 2021;4:e106(1-5). [Google Scholar]