Highlighting Hallux Saltans as an uncommon clinical condition within a demographic not previously documented and underlining the efficacy and cost-effectiveness of non-operative treatment options.
Dr. Rohan, Junior Clinical Fellow, Department of Trauma and Orthopaedics, Wythenshawe Hospital (Manchester University NHS Foundation Trust) Southmoor Road, Manchester, M23 9LT, United Kingdom. E-mail: rohan7@doctors.net.uk
Introduction: Stenosing tenosynovitis is a condition characterized by the inflammation and constriction of the tendons within a fibro-osseous tunnel.
Case Report: We present a case of a 38-year-old man who presented with hallux saltans, a rare manifestation of this condition which was successfully treated with intralesional steroid injection. The patient experienced significant relief from pain and improved function following the procedure.
Conclusion: This case highlights the importance of considering stenosing tenosynovitis as a potential cause of hallux saltans and the efficacy of non-surgical interventions in its management.
Keywords: Stenosing tenosynovitis, hallux saltans, intralesional steroid injection, tarsal tunnel, posterior process of talus.
Tenosynovitis refers to an inflammatory condition involving the synovial sheath of a tendon. [1]. Stenosing forms of tenosynovitis are peculiar entities characterized by the presence of a thickened retinaculum or pulley that constricts the osseo-fibrous tunnel through which the tendon runs [1]. Hallux saltans or “Trigger Toe” was first described in 1940 [2], and is a rare manifestation of stenosing tenosynovitis in the great toe characterized by sudden triggering or locking during flexion followed by sudden release and snapping during extension [3]. We present a case of a 38-year-old man who presented with right hallux saltans secondary to stenosing tenosynovitis at the level of posterior process of the talus or the tarsal tunnel. This case report also illustrates the successful management of this condition using an intralesional steroid injection.
A 38-year-old doctor presented to our orthopedic clinic with 2-year history of right hallux pain and locking. He described episodes of the right hallux suddenly getting “stuck” in a flexed position, which sometimes required manual manipulation to unlock. These episodes of triggering were more pronounced in the morning and were associated with significant pain and discomfort. The patient denied any previous trauma to the right hallux or any systemic medical conditions. He tried to maintain an active lifestyle and played badminton recreationally at the time of review. Physical examination revealed mild tenderness over the plantar aspect of the right hallux, with limited active and passive range of motion. During examination, the patient demonstrated characteristic “locking” of the hallux during active flexion and release or “snapping” during extension. No significant swelling or erythema was observed, and the rest of the foot examination was unremarkable. Neurovascular examination was within normal limits. Radiographs of the right foot were obtained and showed no evidence of bony abnormalities or fractures. The patient was subsequently referred to our interventional radiology colleagues for an ultrasound of the right foot and an intralesional steroid injection if indicated. Ultrasonography revealed mild thickening of the flexor hallucis longus (FHL) tendon resulting in impeded tendon glide most pronounced at the level of posterior process of the talus within the tarsal tunnel. Given the clinical and radiological findings, a diagnosis of hallux saltans secondary to stenosing tenosynovitis was made. The treatment plan was discussed with the patient, and conservative management with an intralesional steroid injection was chosen as the initial approach.
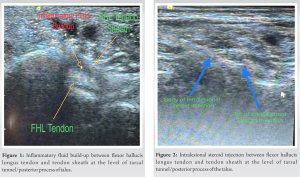
Under sterile conditions and with ultrasound guidance, the posterior process of the talus was identified showing maximum inflammatory fluid build-up around the tendon (Fig. 1). At this site, the patient received 1 ml of 1% lidocaine injection subcutaneously followed by intralesional injection (Fig. 2) of 2 mL of bupivacaine 0.25% with 20 mg of triamcinolone acetonide into the inflamed FHL tendon sheath. The procedure was uneventful. Following the injection, the patient was advised to rest the foot and refrain from any strenuous activities involving the right hallux for 2 weeks. He was also instructed to perform a gentle range of motion exercises during this period. At the post-procedure follow-up visit, the patient reported significant improvement in his symptoms. He no longer experienced episodes of hallux locking, and the pain had substantially reduced. The range of motion of the right hallux had improved, and there was no tenderness at the injection site (Fig. 3). The patient was encouraged to gradually return to his regular activities and was provided with a referral for physical therapy to optimize his hallux function.
During our most recent clinic follow-up which was 2-year post-procedure, the patient reported that pain is still very well managed. However, he does report some clicking of the right hallux which he feels is more psychological and does not interfere with his day-to-day activities. We could not demonstrate any clicking on examination with the right foot examination being unremarkable. The patient was advised to undergo a magnetic resonance imaging (MRI) scan to evaluate the soft tissues of the right foot at 2 years post-procedure. The MRI revealed no signs of tendinitis, ligamentous injuries, effusions, or masses. He has started boxing to maintain fitness and is happy to return for another steroid injection if symptoms get worse.
Stenosing tenosynovitis may occur in any part of an extremity where a tendon must pass through a pulley arrangement and is covered with a sheath [4]. De Quervain tendinopathy is considered to be one of the most recognized forms of inflammation of the tendon sheaths [5]. Other sites include trigger finger (flexor digitorum tendons); extensor carpi ulnaris, extensor carpi radialis, or extensor comunis tendons; flexor hallucis tendon; and peroneal tendons [1]. Hallux saltans is a relatively uncommon presentation of tenosynovitis and has most frequently been reported among ballet dancers [6-8], which may be related to them balancing on the tips of their toes en pointe, meaning extreme plantar flexion of the ankle and first toe in the weight-bearing position [7]. However, other mechanisms are also possible due to people practicing different types of sports such as tennis [9] and running [10]. In the case presented here, the patient is a doctor and plays badminton only recreationally. We found no documented cases in the literature of this rare condition occurring within this particular demographic. The inflammation and constriction were localized to the FHL tendon within the tarsal tunnel, specifically at the level of the posterior process of the talus as visualized during ultrasonography. The surgical release has been the most common treatment employed for Hallux saltans [11]. However, conservative management with intralesional steroid injections has shown success rates as high as 69% in the treatment of trigger fingers [11]. Steroids have potent anti-inflammatory effects and can help reduce tendon sheath inflammation and alleviate symptoms. The choice of the FHL tendon sheath as the injection site in this case was based on the ultrasonography findings, which localized the pathology to a previously specified area. The use of local anesthetic ensured the patient’s comfort during the procedure. The successful outcome, in this case, highlights the efficacy of non-surgical management with intralesional steroid injections for hallux saltans due to stenosing tenosynovitis. The patient experienced rapid relief from pain and a return to near-normal function, with no recurrence of locking or snapping of the hallux at the post-procedure follow-up. The minimally invasive nature of this treatment option, coupled with its effectiveness makes it a valuable option for patients with similar presentations. Moreover, the procedure can be conducted on an outpatient basis, eliminating the need for operating theater space, thereby reducing overhead costs associated with surgical facilities, such as anesthesia, surgical staff, and post-operative care making it a highly cost-effective option for health institutions.
Hallux saltans is a rare manifestation of stenosing tenosynovitis in the great toe, characterized by snapping or locking of the hallux during flexion or extension. Dynamic sonography provides valuable information in the assessment of this condition including identification of focal tendon abnormality as well as guiding management. This minimally invasive treatment offers an effective and well-tolerated treatment option for patients with this condition. Further research and larger-scale studies may help validate its efficacy in a broader patient population.
This case report highlights the successful management of hallux saltans using a minimally invasive approach with ultrasound guidance, highlighting the potential benefits of this technique for the patient in terms of decreased complications and recovery time as well as for the institution in terms of cost and time. It also encourages further research, including larger studies or randomized controlled trials, to further investigate the effectiveness and safety of ultrasound-guided intralesional injection in managing hallux saltans and similar conditions.
References
- 1.Vuillemin V, Guerini H, Bard H, Morvan G. Stenosing tenosynovitis. J Ultrasound 2012;15:20-8. [Google Scholar]
- 2.Lewin P. The Foot and Ankle. Their Injuries, Diseases, Deformities and Disabilities. Philadelphia, PA: Lea and Febiger; 1940. p. 207-8. [Google Scholar]
- 3.Purushothaman R, Karuppal R, Inassi J, Valsalan R. Hallux saltans due to flexor hallucis longus entrapment at a previously unreported site in an unskilled manual laborer: A case report. J Foot Ankle Surg 2012;51:334-6. [Google Scholar]
- 4.Gould N. Stenosing tenosynovitis of the flexor hallucis longus tendon at the great toe. Foot Ankle 1981;2:46-8. [Google Scholar]
- 5.Seyhan H, Kopp J, Horch R. Erkennen sie auf anhieb die tendovaginitis stenosans de quervain? [De Quervain’s stenosing tendovaginitis--one of the most common conditions affecting the hand]. MMW Fortschr Med 2006;148:33-5. [Google Scholar]
- 6.Tudisco C, Puddu G. Stenosing tenosynovitis of the flexor hallucis longus tendon in a classical ballet dancer. A case report. Am J Sports Med 1984;12:403-4. [Google Scholar]
- 7.Lereim P. Trigger toe in classical-ballet dancers. Arch Orthop Trauma Surg (1978) 1985;104:325-6. [Google Scholar]
- 8.Lamata Iturria M, Lison Torres A, Bento Gérard J, Guillen Montijano F. Ténosynovite sténosante bilatérale du long fléchisseur du gros orteil chez une danseuse. A propos d’un cas bilatéral [Bilateral stenosing tenosynovitis of the long flexors of the great toe in a dancer. Apropos of a bilateral case]. Rev Chir Orthop Reparatrice Appar Mot 1988;74:190-2. [Google Scholar]
- 9.Moorman CT 3rd, Monto RR, Bassett FH 3rd. So-called trigger ankle due to an aberrant flexor hallucis longus muscle in a tennis player. A case report. J Bone Joint Surg Am 1992;74:294-5. [Google Scholar]
- 10.Theodore GH, Kolettis GJ, Micheli LJ. Tenosynovitis of the flexor hallucis longus in a long-distance runner. Med Sci Sports Exerc 1996;28:277-9. [Google Scholar]
- 11.Martinez-Salazar EL, Vicentini JR, Johnson AH, Torriani M. Hallux saltans due to stenosing tenosynovitis of flexor hallucis longus: dynamic sonography and arthroscopic findings. Skeletal Radiol 2018;47:747-50. [Google Scholar]