A 10 mm approach for fixation of dorsal displaced distal radius fractures with a volar locking plate can obtain early postoperative outcomes and alignment comparable to conventional incision surgery
Dr. Kiyohito Naito, Department of Orthopaedics, Juntendo University Faculty of Medicine, Bunkyo-ku, Tokyo, Japan. E-mail: knaito@juntendo.ac.jp
Introduction: The aim of this study was to investigate whether surgery with a 10 mm approach for volar locking plate fixation provides equivalent early post-operative outcomes to conventional incision surgery for distal radius fractures.
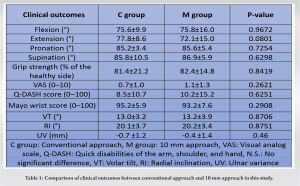
Materials and Methods: The subjects were divided into a conventional incision group (mean age: 59.1 years, 8 males and 23 females) and a 10 mm approach group (mean age: 59.9 years of age, 6 males and 20 females). The wrist range of motion; grip strength; visual analog scale (VAS); quick disabilities of the arm, shoulder, and hand (Q-DASH) score; and modified Mayo score were assessed at 3 months after surgery. In addition, radial inclination, ulnar variance, and volar tilt were evaluated on post-operative radiography.
Results: There was no significant difference between the groups in the wrist range of motion, grip strength, VAS, Q-DASH score, modified Mayo wrist score, and three parameters of post-operative radiography. All patients in both groups had no complications during the perioperative period.
Conclusion: We found that a 10 mm approach obtained early post-operative outcomes and alignment comparable to conventional incision surgery for patients with dorsal displaced distal radius fractures.
Keywords: Distal radius fractures, volar locking plates, conventional incision, 10 mm approach, minimally invasive plate osteosynthesis.
Recently, minimally invasive surgery with a small incision has become widespread in surgery [1, 2]. In orthopedic surgery, minimally invasive surgery has advantages such as a reduction in bleeding amount and hospital stay. Good clinical results in total hip arthroplasty and total knee arthroplasty using a minimal incision have been reported [3, 4]. Furthermore, in osteosynthesis with plates, osteosynthesis using a small incision has been clinically applied, and many clinical studies have been conducted under the concept of minimally invasive plate osteosynthesis (MIPO) [5, 6]. Our institution has been performing distal radius fracture fixation with a volar locking plate as MIPO for the past 10 years. Our previous study reported that volar locking plate fixation with a 10 mm approach is minimally invasive and has a cosmetic advantage; however, the procedure is more complicated than conventional incision surgery [7]. Therefore, we hypothesized that a 10 mm approach for distal radius fracture would obtain equivalent clinical outcomes to conventional surgery. In the present study, the results of early post-operative clinical outcomes were investigated and compared between conventional surgery and surgery with a 10 mm approach for distal radius fracture fixation with a volar locking plate. The occurrence of complications was investigated in both groups.
The study was approved by the Ethics Committee for Medical Research of our university (No. E22-0447), and informed consent was received from all patients. Based on previous reports, we used A2 (extra-articular fractures) and C1 (complete articular fractures) fracture types, according to AO classification, for the 10 mm approach [7]. However, type C1 may not be suitable for fractures that involve a depressed intra-articular fragment, which is needed for the intramedullary reduction to perform osteosynthesis by this technique. Moreover, Type B fractures, or partial articular fractures, were considered contraindications. Between January 2019 and June 2020, 57 patients underwent surgery at our hospital for a distal radius fracture. Among these, 31 patients (mean age: 59.1 [18–87] years old; eight males and 23 females; A2: eight cases, C1: 23 cases) underwent surgery with a conventional approach (C Group). On the other hand, 26 patients (mean age: 59.9 [22–88] years old; six males and 20 females; A2: 13 cases, C1: 13 cases) underwent surgery with a 10 mm approach (M Group). All patients had sustained low-energy trauma, such as collapsing to the floor. All patients underwent surgery under a brachial plexus block. A volar locking plate (Dural Loc V17; MEIRA, Nagoya, Japan) was used in all cases. As previously described, volar locking plate fixation was performed with the Henry approach through a 10 mm incision [7]. The incision was marked on the flexor carpi radialis, starting from 15 mm proximal to the radial styloid (Fig. 1a). The volar locking plate was put on the radius after all muscles, vessels, and nerves of the anterior compartment (except the radial artery) were retracted. To manipulate the volar locking plate more easily, a threaded drill guide is attached. This technique enables the use of a 10 mm approach (Fig. 1b). First, distal locking screws were inserted to fix the plate and the distal fragment. Then, the distal fragment was reduced by the condylar stabilizing technique (Fig. 1c and d) [8]. The skin was closed by a 4–0 nylon thread (Fig. 1e).
In the C group, the wrist range of motion was 75.6° ± 9.9 of flexion, 77.8° ± 8.6 of extension, 85.2° ± 3.4 of pronation, and 85.8° ± 10.5 of supination, and mean grip strength was 81.4 ± 21.2% compared to the healthy side. VAS, Q-DASH score, and modified Mayo score were 0.7 ± 1.0, 8.5 ± 10.7, and 95.2 ± 5.9, respectively. Plain radiography showed that VT, RI, and UV were 13.0° ± 3.2, 20.1° ± 3.7, and −0.7 ± 1.2 mm, respectively. On the other hand, in the M group, the wrist range of motion was 75.8° ± 16.0 of flexion, 72.1° ± 15.0 of extension, 85.6° ± 5.4 of pronation, and 86.9° ± 5.9 of supination, and the mean grip strength was 82.4 ± 14.8% compared to the healthy side. VAS, Q-DASH score, and modified Mayo wrist score were 1.1 ± 1.3, 10.2 ± 15.2, and 93.2 ± 7.6, respectively. Plain radiography showed that VT, RI, and UV were 13.2° ± 3.9, 20.2° ± 3.4, and −0.4 ± 1.4 mm, respectively (Table 1). There was no significant difference between the groups in all categories. All patients had no complications during the perioperative period.
In minimally invasive surgery for distal radius fractures, Imatani et al. and Zenke et al. reported that the advantages of the procedure are that the tissue is less invaded, the post-operative pain is reduced at an early stage, and the wound is small and less noticeable [10, 11]. In a previous study, we reported that there were no difficulties to fix with the volar locking plate, and bone union was achieved in all patients [7]. Surgery with a 10 mm approach for distal radius fractures is a very complicated procedure, and case reports are rare. In the volar approach, there are flexor tendons and the median nerve between the incision and fragments, and these tissues need to be retracted to attach the plate to the fragment [7]. The risks of post-operative flexor tendon injuries and carpal tunnel syndrome are increased if the reduction is poor or the plate is floating because of the complexity of the procedure [12-14]. In addition, the plate is not designed for a 10 mm approach. Despite these complexities, our previous study and the present study found no technical trouble performing surgery with a 10 mm approach [7]. In this study, superior clinical outcomes were obtained in both groups, and there was no significant difference in all categories between the groups. Kodama et al. reported a significant correlation between post-operative plain radiography parameters (VT, UV) and clinical outcomes in volar locking plate fixation for distal radius fractures [15]. In this study, good post-operative clinical outcomes and post-operative plain radiography parameters (VT, RI, and UV) were obtained in all cases. Good alignment was obtained because the included cases had simple dorsal dislocated distal radius fractures (types A2 and C1 according to the AO classification). In addition, since the detachment of soft tissue was reduced in the minimal incision group, it was possible to obtain a reduction position by ligamentotaxis. Thus, this may explain why good alignment was obtained even in the group receiving surgery with a 10 mm approach [16]. There are some limitations to this study. The first is that the follow-up period was 3 months. Previous studies reported a follow-up period of 12 months or longer for volar locking plate fixation [17, 18]. However, the purpose of this study was to investigate the clinical outcomes and the occurrence of complications in the early post-operative period. Moreover, there are reports that clinical scores, such as the Q-DASH score and Mayo wrist score, which were evaluated in this study, show a ceiling effect 3 months after operation, and recovery of the upper limb function sufficient for returning to daily life is also acquired early, at 3 months after surgery [19, 20]. Therefore, we considered that 3 months was sufficient for the observation period of this study. The second is that it took a long time to acquire the procedure for performing surgery with a 10 mm approach. Our team had undergone many successful surgeries with a 10 mm approach before this study [7, 21]. Although the first cases required a lot of operation time, at the time of this study, all operators were able to perform surgery with a 10 mm approach. Finally, the number of patients was small and insufficient for statistical analysis. The effect size by t-test was d = 0.4662119 and verification power is 1–β = 0.3954425l; thus, the number of cases may have been insufficient to obtain sufficient verification power. Although the maximum possible number of patients was included, in the future, it will be necessary to conduct research using a larger sample of cases.
In this study, the results of early post-operative clinical outcomes were investigated and compared between conventional surgery and surgery with a 10 mm approach for fixation of dorsal displaced distal radius fractures with a volar locking plate. Surgery with a 10 mm approach for distal radius fractures is a very complicated procedure. However, since the detachment of soft tissue was reduced in a 10 mm approach, it was possible to obtain a reduction position by ligamentotaxis. Therefore, this study suggested that a 10 mm approach obtained early post-operative outcomes and alignment comparable to conventional incision surgery.
In the fixation of dorsal displaced distal radius fractures with a volar locking plate, a 10mm approach can obtain early postoperative outcomes and alignment comparable to conventional incision surgery.
References
- 1.Frumovitz M, Sun CC, Jhingran A, Schmeler KM, Reis DR, Milam MR, et al. Radical hysterectomy in obese and morbidly obese women with cervical cancer. Obstet Gynecol 2008;112:899-905. [Google Scholar]
- 2.Azagra JS, Goergen M, Arru L, Facy O. Total gastrectomy for locally advanced cancer: The pure laparosopic approach. Gastroenterol (Oxf) 2013;1:119-26. [Google Scholar]
- 3.Bonutti MP, Mont AM, McMahon M, Ragland SP, Kester M. Minimally invasive total knee arthroplasty. J Bone Joint Surg Am 2004;86:26-32. [Google Scholar]
- 4.Sculco TP, Jordan LC, Walter WL. Minimally invasive total hip arthroplasty: The hospital for special surgery experience. Orthop Clin North Am 2004;35:137-42. [Google Scholar]
- 5.Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: A retrospective study of 32 patients. Injury 2007;38:365-70. [Google Scholar]
- 6.Kayali C, Haluk A, Eren A, Serkan O. How should open tibia fractures be treated? A retrospective comparative study between intramedullary nailing and biologic plating. Ulus Travma Acil Cerrahi Derg 2009;15:243-8. [Google Scholar]
- 7.Naito K, Zemirline A, Sugiyama Y, Obata H, Liverneaux P, Kaneko K. Possibility of fixation of a distal radius fracture with a volar locking plate through a 10 mm approach. Tech Hand Up Extrem Surg 2016;20:71-6. [Google Scholar]
- 8.Kiyoshige Y. Condylar stabilizing technique with AO/ASIF distal radius plate for colles’fracture associated with osteoporosis. Tech Hand Up Extrem Surg 2002;6:205-8. [Google Scholar]
- 9.Hassoun A, Haroun R, Hoyek F, Lahoud JC, Tawk C, El Hajj Moussa M, et al. Relation between the dash score and radiographic evaluation of the wrist in patients with wrist fracture. BMC Musculoskelet Disord 2024;25:217. [Google Scholar]
- 10.Imatani J, Noda T, Morito Y, Sato T, Hashizume H, Inoue H. Minimally invasive plate osteosynthesis for comminuted fractures of the metaphysis of the radius. J Hand Surg Br 2005;30:220-5. [Google Scholar]
- 11.Zenke Y, Sakai A, Oshige T, Moritani S, Fuse Y, Maehara T, et al. Clinical results of volar locking plate for distal radius fractures: Conventional versus minimally invasive plate osteosynthesis. J Orthop Trauma 2011;25:425-31. [Google Scholar]
- 12.Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma 2007;21:316-22. [Google Scholar]
- 13.Itsubo T, Hayashi M, Uchiyama S, Hirachi K, Minami A, Kato H. Differential onset patterns and causes of carpal tunnel syndrome after distal radius fracture: A retrospective study of 105 wrists. J Orthop Sci 2010;15:518-23. [Google Scholar]
- 14.Kivrak A, Igrek S, Uiusoy I. Comparison of cases with and without carpal tunnel release in volar plate fixation of AO type 23-B and 23-C feactures. Exp Biomed Res 2023;6:308-13. [Google Scholar]
- 15.Kodama N, Takemura Y, Ueba H, Imai S, Matsusue Y. Acceptable parameters for alignment of distal radius fracture with conservative treatment in elderly patients. J Orthop Sci 2014;19:292-7. [Google Scholar]
- 16.Igeta Y, Vemet P, Facca S, Naroura I, Diaz JJ, Liverneaux PA. The minimally invasive flexor carpi radialis approach: A new perspective for distal radius fractures. Eur J Orthop Surg Traumatol 2018;28:1515-22. [Google Scholar]
- 17.Mulders MA, Walenkamp MM, van Dieren S, Goslings JC, Schep NW, VIPER Trial Collaborators. Volar plate fixation versus plaster immobilization in acceptably reduced extra-articular distal radial fractures: A multicenter randomized controlled trial. J Bone Joint Surg Am 2019;101:787-96. [Google Scholar]
- 18.Saving J, Severin Wahlgren S, Olsson K, Enocson A, Ponzer S, Sköldenberg O, et al. Nonoperative treatment compared with volar locking plate fixation for dorsally displaced distal radial fractures in the elderly: A randomized controlled trial. J Bone Joint Surg Am 2019;101:961-9. [Google Scholar]
- 19.Kim SJ, Lee BG, Lee CH, Choi WS, Kim JH, Lee KH. Comparison of ceiling effects between two patient-rating scores and a physician-rating score in the assessment of outcome after the surgical treatment of distal radial fractures. Bone Joint J 2015;97:1651-6. [Google Scholar]
- 20.Nagura N, Naito K, Sugiyama Y, Obata H, Goto K, Kaneko A, et al. Evaluation of patient-reported and clinician-reported outcomes of volar locking plate fixation for distal radius fractures. J Hand Surg Asian Pac Vol 2020;25:359-63. [Google Scholar]
- 21.Naito K, Sugiyama Y, Kinoshita M, Zemirline A, Taleb C, Dilokhuttakarn T, et al. Minimally invasive plate osteosynthesis for a distal radius fracture with forearm skin problem. Case Rep Orthop 2018;2018:8195376. [Google Scholar]