In patients with an atypical femoral fracture, radiographs or computed tomography (CT) images should be obtained for both legs considering the impending atypical femoral fracture on the contralateral side. A one- or two-stage bilateral surgery can prevent long-term bed rest in older patients.
Dr. Kazuki Fujimoto, Department of Orthopaedic Surgery, Kohnodai Hospital, National Center for Global Health and Medicine, Chiba, Japan. E-mail: s9082@nms.ac.jp
Introduction: Long-term bisphosphonate (BP) administration may cause an atypical femoral fracture that is occasionally bilateral. We encountered a case of an impending atypical femoral fracture on the contralateral side that progressed to a complete fracture early after surgery for an atypical femoral fracture.
Case Report: An 83-year-old woman who had received long-term BP therapy developed a right femoral atypical incomplete fracture that progressed to a complete fracture 5 days after surgery for an atypical complete left femoral fracture.
Conclusion: The findings from this case suggest that when an atypical femoral fracture occurs in patients receiving long-term BP therapy, the possibility of an impending atypical femoral fracture on the contralateral side should be considered, and radiographs or CT images should be obtained for both legs. To prevent long-term bed rest in older adults, one- or two-stage bilateral surgery should be considered when imaging reveals bilateral atypical femoral fractures.
Keywords: Atypical femoral fracture, bisphosphonates, computed tomography, surgery.
Long-term bisphosphonate (BP) administration may cause an atypical femoral fracture (AFF) that is occasionally bilateral [1-4]. Imaging tests of both legs are necessary to diagnose atypical incomplete fractures [5]. However, when the fracture on the contralateral side is incomplete, it remains unclear whether surgery should be performed and, if so, it’s optimal timing. Here, we report a case of bilateral AFF diagnosed using computed tomography (CT) in an older woman receiving long-term BP therapy. The patient developed an impending AFF on the contralateral side that progressed to a complete fracture early after surgery for an AFF.
An 83-year-old woman had experienced right leg pain for approximately 1 year. She was diagnosed with lumbar spinal stenosis by a local doctor and had been consuming oral analgesics. She had a history of osteoporosis and had been receiving BPs (oral administration of minodronate for 1 year, intravenous alendronate for 1 year, and intravenous ibandronate for 3 years) and the active form of vitamin D analog (oral administration of eldecalcitol) prescribed by a local doctor for more than 5 years. She had no history of malignant tumors. She could walk independently with a T-cane; however, when she exerted weight on the left leg and lost balance, she felt severe pain in that leg and could not walk. She was subsequently admitted to our hospital. Her height, weight, and body mass index were 158.0 cm, 57.0 kg, and 22.8 kg/m2, respectively. Medical history included hypertension and cerebral hemorrhage that had resolved without sequelae. Radiographs of her left leg showed a short oblique fracture of the femoral diaphysis with a periosteal reaction, cortical thickening, and beak-like changes at the fracture site (Fig. 1).
The patient was diagnosed with an atypical complete left-sided femoral fracture. Subsequent CT revealed bilateral AFF, with an incomplete fracture of the right femur with cortical thickening and beak-like changes (Fig. 2). Blood tests showed no anemia (hemoglobin, 14.0/mL) and no abnormalities in calcium levels (9.7 mg/dL). BP administration was discontinued, and eldecalcitol was continued. Because the leg pain was considered related to lumbar spinal stenosis, surgery was planned only for the left-side complete fracture.
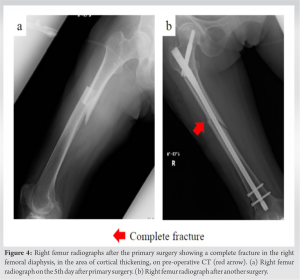
Primary surgery was performed for the complete fracture in the left leg 4 days after the injury (Fig. 3). An intramedullary nail was used. The patient was not allowed to exert weight on the left leg but was allowed to exert full weight on the right leg; early mobilization was started the following day. On the 5th day after primary surgery, when exerting body weight on the right leg, the patient felt severe pain in that leg and was unable to stand up from the floor. Radiographs revealed a complete fracture in the right femoral diaphysis, which was in the area of cortical thickening, on pre-operative CT (Fig. 4a). She was diagnosed with another atypical complete femoral fracture in the right leg.
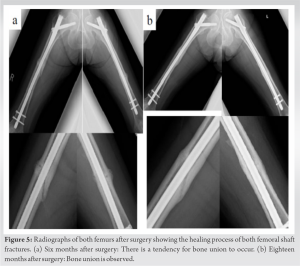
Another surgery was performed with an intramedullary nail on the 3rd day after the right leg fracture (Fig. 4b). The pain reduced, and the post-operative course was unremarkable; however, she was not allowed to walk on both legs for approximately 4 weeks after the surgeries and was only allowed to move the lower limbs with both legs unloaded. Consequently, long-term bed rest was advised. Post-operative assessment of bone density using dual-energy X-ray absorptiometry indicated osteoporosis in the lumbar spine (bone mineral density: 0.661 g/cm2, t score: −3.2). The patient was allowed to practice walking with full weight bearing approximately 2 months after the surgeries and was finally allowed to walk with a T-cane 6 months after surgeries. Radiography revealed the healing process with bony callus formation at the fracture site (Fig. 5a). During follow-up, she developed a lumbar compression fracture. Therefore, after confirming bone union, denosumab was initiated to prevent new fragility fractures 18 months after surgery (Fig. 5b). The BP discontinuation period was 18 months.
The findings from this case suggested the following: First, an AFF on one side may indicate an impending AFF on the contralateral side, and the necessary investigations should always be performed. Radiography and CT are useful for diagnosing AFFs. According to a review of AFFs in a report by a task force of the American Society for Bone and Mineral Research (ASBMR), 100 out of 100,000 patients treated with BPs for more than 3 years develop AFFs every year [5], with the occasional occurrence of a bilateral AFFs; however, simultaneous occurrence of bilateral complete fracture is rare [1-4]. BPs negatively affect collagen maturation in the bone, reduce turnover, result in accumulated damage from load stress, and reduce strength [6, 7]. Although BP therapy has been excluded as a risk factor for AFF [5, 8], patients receiving these medications remain at risk of periprosthetic AFF [9]. Long-term BP administration can cause all types of AFFs, not only periprosthetic AFFs; therefore, the ASBMR task force criteria need to be revised. In addition, it has been reported that 50–77% of patients with AFFs have prodromal symptoms [10,11]. Leg pain caused by AFF may be diagnosed as other locomotory diseases, and complete fractures may occur during the period of misdiagnosis [5, 12]. Imaging tests for both legs are necessary for the diagnosis of patients receiving long-term BP therapy and complaining of leg pain [2]. In the present case, the patient had been receiving BPs for >5 years and had complained of leg pain for approximately 1 year. She was diagnosed and treated for lumbar spine stenosis by a local doctor, and a bilateral leg CT on admission to our hospital later revealed bilateral AFFs. Second, for patients with bilateral AFFs with an incomplete fracture on one side, surgery only on the complete fracture side may increase the burden on the contralateral side and can be a risk factor for a subsequent complete fracture on that side. Prophylactic surgery should be considered for patients with AFFs showing prodromal symptoms [1, 2]. However, there are no reports on the timing of the surgery. A previous study reported bilateral simultaneous surgery in cases with incomplete fractures on one side, with a good outcome [13]. With regard to simultaneous bilateral lower limb surgery, there are many reports on the usefulness of one-stage bilateral total hip arthroplasty, which requires anesthesia only once, shortens the morbidity period and the hospitalization period, and reduces medical costs [14]. However, because bleeding is heavier in one-stage surgery than in two-stage surgery [15,16], the mortality rate is higher for high-risk patients. In such cases, two-stage surgery should be considered [17]. Post-operative treatment for osteoporosis in patients with AFFs remains controversial. Denosumab is also a bone resorption inhibitor and is associated with a low incidence of AFF [18]. Thus, denosumab can be an option for osteoporosis treatment after sufficient withdrawal of BPs, and it was accordingly prescribed to our patient. However, data regarding Vitamin D status, bone remodeling biomarkers, and thyroid hormones that can affect osteoporosis were not obtained, which is a limitation of this study. In the present case, the pain in the contralateral leg was considered to occur because of lumbar spinal stenosis and was not considered a pre-cursor symptom of an AFF, and complete weight bearing on that leg was allowed without preventive surgery, resulting in an early complete fracture. One-stage bilateral osteosynthesis surgery was a possible option for our patient. However, she was 83-year-old and had a history of cerebral hemorrhage; therefore, two-stage bilateral surgery would have been more feasible, allowing early ambulation and preventing disuse.
When an AFF occurs in patients on long-term BP therapy, the possibility of an impending AFF on the contralateral side should be considered, and radiographs or CT images should be obtained for both legs. One- or two-stage bilateral surgery can prevent long-term bed rest in older patients. However, these findings are based on a single case report, and long-term follow-up is necessary.
Patients on long-term BPs may develop AFF.
Radiography and CT are helpful in diagnosing bilateral AFF.
An incomplete fracture may progress to complete after unilateral surgery in AFF.
References
- 1.Capeci CM, Tejwani NC. Bilateral low-energy simultaneous or sequential femoral fractures in patients on long-term alendronate therapy. J Bone Joint Surg Am 2009;91:2556-61. [Google Scholar]
- 2.Higgins M, Morgan-John S, Badhe S. Simultaneous, bilateral, complete atypical femoral fractures after long-term alendronate use. J Orthop 2016;13:401-3. [Google Scholar]
- 3.Kobayashi T, Ishikawa T, Katsuragi J, Sasaki Y, Ohtori S. Open reduction and internal fixation of simultaneous, bilateral, atypical femoral shaft fractures after nine years of bisphosphonate treatment. Cureus 2021;13:e19177. [Google Scholar]
- 4.Hwang S, Seo M, Lim D, Choi MS, Park JW, Nam K. Bilateral atypical femoral fractures after bisphosphonate treatment for osteoporosis: A literature review. J Clin Med 2023;12:1038. [Google Scholar]
- 5.Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2014;29:1-23. [Google Scholar]
- 6.Allen MR, Reinwald S, Burr DB. Alendronate reduces bone toughness of ribs without significantly increasing microdamage accumulation in dogs following 3 years of daily treatment. Calcif Tissue Int 2008;82:354-60. [Google Scholar]
- 7.Burr DB, Liu Z, Allen MR. Duration-dependent effects of clinically relevant oral alendronate doses on cortical bone toughness in beagle dogs. Bone 2015;71:58-62. [Google Scholar]
- 8.Shane E, Burr D, Ebeling PR, Abrahamsen B, Adler RA, Brown TD, et al. Atypical subtrochanteric and diaphyseal femoral fractures: Report of a task force of the American society for bone and mineral Research. J Bone Miner Res 2010;25:2267-94. [Google Scholar]
- 9.Mondanelli N, Facchini A, Troiano E, Muratori F, Bottai V, Giannotti S. Periprosthetic atypical femoral fractures exist: A retrospective study at a single institution. Prevalence on 115 periprosthetic femoral fractures around a primary hip stem. J Arthroplasty 2021;36:2189-96. [Google Scholar]
- 10.Schneider JP, Hinshaw WB, Su C, Solow P. Atypical femur fractures: 81 individual personal histories. J Clin Endocrinol Metab 2012;97:4324-8. Erratum in: J Bone Miner Res 2011;26, 1987 [Google Scholar]
- 11.Markman LH, Allison MB, Rosenberg ZS, Vieira RL, Babb JS, Tejwani NC, et al. A retrospective review of patients with atypical femoral fractures while on long-term bisphosphonates: Including pertinent biochemical and imaging studies. Endocr Pract 2013;19:456-61. [Google Scholar]
- 12.Ward WG Sr., Carter CJ, Wilson SC, Emory CL. Femoral stress fractures associated with long-term bisphosphonate treatment. Clin Orthop Relat Res 2012;470:759-65. [Google Scholar]
- 13.Moghnie A, Scamacca V, De Fabrizio G, Valentini R. Atypical femoral fractures bilaterally in a patient receiving bisphosphonate: A case report. Clin Cases Miner Bone Metab 2016;13:57-60. [Google Scholar]
- 14.Wang H, Fan T, Li W, Yang B, Lin Q, Yang M. A nomogram to predict the risk of prolonged length of stay following primary total hip arthroplasty with an enhanced recovery after surgery program. J Orthop Surg Res 2021;16:716. [Google Scholar]
- 15.Berend ME, Ritter MA, Harty LD, Davis KE, Keating EM, Meding JB, et al. Simultaneous bilateral versus unilateral total hip arthroplasty an outcomes analysis. J Arthroplasty 2005;20:421-6. [Google Scholar]
- 16.Bhan S, Pankaj A, Malhotra R. One- or two-stage bilateral total hip arthroplasty: A prospective, randomized, controlled study in an Asian population. J Bone Joint Surg Br 2006;88:298-303. [Google Scholar]
- 17.Alfaro-Adrián J, Bayona F, Rech JA, Murray DW. One- or two-stage bilateral total hip replacement. J Arthroplasty 1999;14:439-45. [Google Scholar]
- 18.Kendler DL, Cosman F, Stad RK, Ferrari S. Denosumab in the treatment of osteoporosis: 10 years later: A narrative review. Adv Ther 2022;39:58-74. [Google Scholar]