Open reduction of irreducible elbow dislocations due to varus posteromedial rotary instability may require addressing capsular interposition, ligament repair, and coronoid fixation for optimal outcome.
Dr. Prasoon Kumar, Department of Orthopaedics, PGIMER, Chandigarh, India. E-mail: drprasoonksingh@gmail.com
Introduction: Elbow dislocations, particularly those associated with varus posteromedial rotary instability, are relatively uncommon. We present the case of a 25-year-old male initially managed nonoperatively for a posterior elbow dislocation, who subsequently experienced irreducible re-dislocation with characteristic fractures of the anteromedial facet and tip of the coronoid, indicative of varus posteromedial rotary instability.
Case Report: Following an unsuccessful attempt at closed reduction under general anesthesia, open reduction was performed, revealing the interposition of the posterior capsule of the humero-ulnar joint as the cause of irreducibility. Fixation of the coronoid fracture was undertaken, and the patient exhibited excellent functional outcomes at a 4.5-year follow-up.
Conclusion: This case underscores the rarity of irreducible elbow dislocation in the context of varus posteromedial rotary instability and highlights the crucial role of capsular interposition in such cases. Successful open reduction, coronoid fixation, and attentive postoperative care contributed to the patient’s favorable long-term functional outcome.
Keywords: Varus posteromedial rotary instability, elbow dislocation, capsular Interposition, open reduction, coronoid fracture.
Acute elbow dislocations are relatively common, with a reported rate of approximately 5/100,000 person-years, with adolescent males being particularly susceptible [1]. Simple dislocations, which do not involve fractures, are more prevalent than complex fracture-dislocations. Most acute elbow dislocations occur posteriorly or posterolaterally, often due to falls onto outstretched hands with the forearm in a pronated position, while other types such as anterior, lateral, and posteromedial dislocations, as well as transolecranon fracture dislocations, are less frequent [2]. Most elbow dislocations are amenable to closed reduction; irreducible elbow dislocation, though uncommon, presents significant challenges and often results in poorer outcomes. Inadequate evaluation or management of accompanying injuries to the coronoid, radial head, and ligaments during initial elbow dislocations can contribute to its persistence and so is the patient’s delay in seeking treatment. Irreducibility by closed means may also be attributable to osseous or soft tissue interposition or buttonholing of the radial head through the lateral collateral ligament (LCL) complex. Treating elbow instability poses a challenge as it necessitates a delicate balance between addressing instability and avoiding excessive stiffness. Arthroscopic assessment plays a crucial role in diagnosing and evaluating the severity of acute or chronic instability cases, allowing for precise treatment planning. Capsular-ligament plication or ligament reattachment using suture anchors are common arthroscopic treatment methods [3]. Surgical repair or reconstruction of ligamentous injuries, such as LCL and medial collateral ligament, is indicated in cases of severe or recurrent instability, with various techniques available depending on the extent of the injury and patient factors [4]. Most of the cases reported in the literature are those of posterior, simple elbow dislocations, wherein the elbow dislocation is not associated with any fracture [4-13]. Irreducibility after varus posteromedial rotary instability of the elbow has not been reported so far in the literature. We present a case of irreducible posterior elbow dislocation due to varus posteromedial rotary instability, wherein interposition of the posterior capsule of the humero-ulnar joint prevented relocation of the elbow.
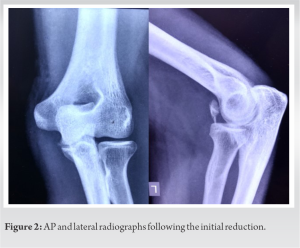
A 25-year-old, otherwise, healthy male was referred to our center with an irreducible posterior elbow dislocation. He had injured himself 1 month back after falling on the elbow while attempting to catch a cricket ball. Closed reduction under conscious sedation was performed by an orthopedic surgeon elsewhere and the elbow was immobilized in a back-slab (Fig. 2). At 3 weeks, the back-slab was removed. As the patient attempted to extend the elbow, he felt a jerk and had sudden onset pain. Repeat radiographs confirmed re-dislocation. Closed reduction was attempted again but failed, and the patient was referred to our center.
On presentation, we noted that the patient had minimal swelling around the elbow and painful restriction of flexion-extension movements as well as prono-supination. There was no neurovascular deficit.
Investigations
On the initial radiographs, we noted a posterolateral elbow dislocation with a fracture of the coronoid tip and anteromedial facet, typical of a varus posteromedial rotary mechanism (Fig. 1a and b). In addition to the findings of initial radiographs, redislocation radiographs revealed significant anterior translation of the distal humerus, relative to the proximal radius and ulna. A computed tomography (CT) scan of the elbow was done; sagittal and coronal reformatted sections and three-dimensional volume rendered images were obtained (Fig. 1c and d). No osseous interposition was noticed in any of the radiographs or computed tomography scans. Post-reduction radiographs showed a congruently reduced elbow (Fig 2). As the elbow had been successfully reduced previously by closed reduction, we assumed that the irreducibility was due to pain and inadequate muscle relaxation, and magnetic resonance imaging was not obtained to check for soft-tissue interposition. We planned to attempt closed reduction under general anesthesia, failing which we would resort to open reduction. In either case, we planned to perform internal fixation of the coronoid and repair of the LCL.
Treatment
Under general anesthesia, we attempted to perform a closed reduction of the elbow; however, this was unsuccessful and we proceeded to open reduction. The patient was placed in the lateral decubitus position. The elbow was approached through the utilitarian posterior midline incision, taking care to curve the incision medially around the olecranon. The ulnar nerve was identified and dissected till its course between the two heads of the flexor carpi ulnaris. Thereafter, the triceps muscle was carefully lifted off the distal humerus in a medial-to-lateral direction. As soon as this was performed, we could visualize soft tissue interposed in the humero-ulnar joint (Fig 3). On further inspection, this was found to be the posterior capsule of the humero-ulnar joint (Fig 4). We attempted to use a Freer elevator to lift the capsule off the trochlea, but this could not be done. We then resorted to splitting the capsule by sharp dissection. At this point, the elbow could be reduced with minimal force but it was grossly unstable, as anticipated. We could identify the tip and the anteromedial facet fragments of the coronoid (Fig. 2). To fix the coronoid tip fragment, which essentially contains the anterior capsule and the brachialis insertion, we used a transosseous suture fixation technique as described by Morrey and O’Driscoll [14]. Briefly, multiple suture bites with Ethibond No 2 were taken through the anterior capsule and the brachialis tendon, passed through two tunnels in the ulna, and tied securely on its dorsal aspect with the elbow in 90° of flexion, after ensuring that the fragment was well reduced onto the crater. We then reduced and fixed the anteromedial facet fragment with a single headless screw and used a mini plate as a buttress (Fig. 5).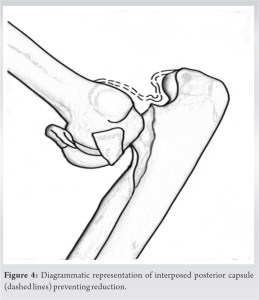
Outcome and Follow-up
The external fixator was removed after 10 days and a gradual active range of flexion-extension was started in an elbow range-of-motion brace with the forearm in neutral rotation. The brace was discontinued after 6 weeks and unrestricted prono-supination was permitted. Serial clinical and radiological examination was done. The patient had an uneventful postoperative course and regained a painless full range of flexion-extension and prono-supination by 3-month follow-up. By 6 months, the patient achieved complete radiological fracture union. Mild heterotopic ossification was noted along the posterior aspect of the olecranon. At 2-year follow-up, one screw from the buttress plate was noted to have backed out therefore, the plate along with screws was removed. One screw was noted to be buried deep in the anteromedial pericapsular tissues of the humero-ulnar joint and could not be approached through the midline posterior approach (Fig 6). Removal of this screw would have necessitated a separate anterior approach and dissection of the anterior humero-ulnar joint capsule. Since this screw was anterior, and far away from the ulnar nerve, as well as the humero-ulnar joint, a second, anterior approach to remove the screw was not performed. The patient was counseled about the retained screw and has been offered the option for removal if it were to become symptomatic in future. At the time of writing this report, the patient has been in follow-up for about 4 years and 5 months. He was noted to have a loss of terminal 5° of hyperextension as compared to the other side, and a full range of flexion, with no complaints of instability (Fig. 7). Radiology demonstrated a congruent elbow with complete union of the coronoid fragments and no signs of arthrosis of the elbow (Fig. 4). Minimal heterotopic ossification was noted on the posterior aspect of the elbow, but this did not result in any symptoms and was therefore not addressed. The Mayo Elbow performance score at the final follow-up was 95.
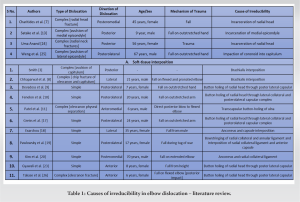
Elbow dislocations can be classified as “simple” or “complex,” depending on whether or not they involve the articular and ligamentous structures that contribute to elbow stability [16]. A review of the published literature on irreducible elbow dislocations reveals a variety of causes (Table 1). The dislocation was simple in most cases and most often, posterolateral [9, 10, 17-19]. The most frequently reported cause for irreducibility was buttonholing of the radial head posteriorly through a tear in the lateral ligament complex or the common extensor origin [9, 10, 19, 20]. To achieve reduction, the tear needed to be enlarged to allow the radial head to fall back into place; the rent was repaired subsequently [9, 10, 19, 20].
Osseous interposition has also been reported as a cause for irreducibility [7, 13, 17, 18]. Perhaps, the most commonly interposed structure is the medial epicondyle and the mechanism for this has been well described. As valgus force is applied to the elbow, the medial epicondyle fails in tension. The ulnohumeral joint opens up and the vacuum thus created entraps in the displaced epicondyle within the joint, preventing reduction. Interposition of the fractured radial head has also been reported as a cause of irreducible posterolateral dislocation [7, 17]. Varus posteromedial rotatory instability (VPMRI) is known to be associated with instability and recurrent dislocations [21-23]. Due to capsule-ligamentous disruption and fracture of the coronoid, the reduction is usually easy [24]. The inability to reduce a dislocated elbow joint in the presence of VPMRI has not yet been reported to the best of our knowledge. Chhaparwal et al. [8] reported a case of irreducible elbow dislocation due to the interposition of the brachialis muscle with chip fractures of the coronoid and capitulum. However, these fracture fragments were small and did not cause any instability. We discovered that in our case, closed reduction during the 2nd time was prevented by the torn, interposed posterior capsule (Fig. 5). A probable explanation could be that the posterior capsule would have sustained damage during the primary dislocation. In the subsequent 3 weeks, it did not heal completely. During the second episode, the incompletely healed capsule probably re-ruptured and got entrapped in the ulno-humeral joint. Once the aforementioned issue was addressed surgically, the elbow could be reduced easily.
Irreducible elbow dislocation is uncommonly encountered after VPMRI of the elbow. When faced with this problem, the surgeon must think in terms of obstacles to reduction. The present case highlights the role of the interposed posterior capsule of the humero-ulnar joint as an obstacle to reduction.
- Irreducibility in the case of varus posteromedial rotary instability of the elbow is rare, and warrants open reduction. In this case, the interposition of the humero-ulnar joint capsule was the cause of irreducibility.
- To ensure an excellent functional outcome in such cases, the surgeon must ensure congruent reduction of the elbow, repair the LCL, and perform adequate fixation of the tip as well as the anteromedial facet fragment of the coronoid.
References
- 1.Van der Windt AE, Colaris JW, den Hartog D, The B, Eygendaal D. Persistent elbow dislocation. JSES Int 2023;7:2605-11. [Google Scholar]
- 2.Tao F, Zhou D, Song W. Trans-olecranon fracture posterior dislocation: A novel type of elbow injury. J Orthop Surg Res 2023;18:228. [Google Scholar]
- 3.Smith MF. Surgery of the Elbow. Springfield, Illinois: Charles C Thomas; 1954. p. 233. [Google Scholar]
- 4.Marinelli A, Graves BR, Bain GI, Pederzini L. Treatment of elbow instability: State of the art. J ISAKOS 2021;6:102-15. [Google Scholar]
- 5.Atkinson CT, Pappas ND, Lee DH. Irreducible posterolateral elbow dislocation. Am J Orthop (Belle Mead NJ) 2014;43:E34-6. [Google Scholar]
- 6.Bradley MP, Tashjian RZ, Eberson CP. Irreducible radial head dislocation in a child: A case report. Am J Orthop (Belle Mead NJ) 2007;36:E76-9. [Google Scholar]
- 7.Charitides J, Kitsis C, Tsakonas A. Irreducible elbow dislocation associated with a radial neck fracture: A case report. Acta Orthop Belg 2001;67:395-8. [Google Scholar]
- 8.Chhaparwal M, Aroojis A, Divekar M, Kulkarni S, Vaidya SV. Irreducible lateral dislocation of the elbow. J Postgrad Med 1997;43:19-20. [Google Scholar]
- 9.Devadoss A. Irreducible posterior dislocation of the elbow. Br Med J 1967;3:659. [Google Scholar]
- 10.Fenelon C, Zafar MM, Sheridan GA, Kearns S. Irreducible posterolateral elbow dislocation: A rare injury. BMJ Case Rep 2016;2016:bcr2016217967. [Google Scholar]
- 11.Patel NN, Bruce RW. Transcapsular buttonholing of the proximal ulna as a cause for irreducible pediatric anterior elbow dislocation. Case Rep Orthop 2018;2018:8986230. [Google Scholar]
- 12.Rodriguez-Merchan EC. Controversies on the treatment of irreducible elbow dislocations with an associated non-salvageable radial head fracture. J Orthop Trauma 1995;9:341-4. [Google Scholar]
- 13.Satake Y, Tomori Y, Sawaizumi T, Nanno M, Kodera N, Takai S. Irreducible elbow fracture and dislocation due to incarceration of the medial epicondyle of the humerus in a child. J Nippon Med Sch 2018;85:60-5. [Google Scholar]
- 14.Morrey BF, O’Driscoll SW. Fractures of the coronoid and complex instability of the elbow. In: Master Techniques in Orthopaedic Surgery: The Elbow. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2002. p. 128-38. [Google Scholar]
- 15.Kumar D, Sodavarapu P, Kumar K, Hooda A, Neradi D, Bachchal V. Functional outcome of surgically treated isolated coronoid fractures with elbow dislocation in young and active patients. Cureus 2020;12:e10883. [Google Scholar]
- 16.Morrey BF. Current concepts in the management of complex elbow trauma. Surgeon 2009;7:151-61. [Google Scholar]
- 17.Greiss M, Messias R. Irreducible posterolateral elbow dislocation: A case report. Acta orthopaedica Scandinavica 1987;58:421-2. [Google Scholar]
- 18.Exarchou EJ. Lateral dislocation of the elbow. Acta Orthop Scand 1977;48:161-3. [Google Scholar]
- 19.Pawlowski RF, Palumbo FC, Callahan JJ. Irreducible posterolateral elbow dislocation: Report of a rare case. J Trauma Acute Care Surg 1970;10:260-6. [Google Scholar]
- 20.Kim SJ, Ji JH. Irreducible posteromedial elbow dislocation: A case report. J Shoulder Elbow Surg 2007;16:e1-5. [Google Scholar]
- 21.Gyawali GP, Pokharel B, Pokharel RK. Irreducible anterior dislocation of the elbow without associated fracture. JNMA J Nepal Med Assoc 2013;52:398-401. [Google Scholar]
- 22.Ramirez MA, Stein JA, Murthi AM. Varus posteromedial instability. Hand Clin 2015;31:557-63. [Google Scholar]
- 23.Chan K, Athwal GS. Varus Posteromedial Rotatory Instability. The Unstable Elbow 2017 (pp. 75-84). [Google Scholar]
- 24.Anand U. A rare presentation of irreducible posterior dislocation of elbow-radial head interposition. Univ J Surg Surg Special 2017;3(3). [Google Scholar]
- 25.Weng HK, Chang WL, Yeh ML, Su WR, Hsu KL. Irreducible elbow dislocation associated with hill? Sachs-like lesion over the capitellum. Clin Shoulder Elbow 2019;22:37-9. [Google Scholar]
- 26.Takase K, Mizuochi J. Irreducible dislocation of the radial head with undisplaced olecranon fracture in a child: A case report. J Pediatr Orthop B 2011;20:345-8. [Google Scholar]