Surgical bony osteotomy is used for correction of fixed equinus deformity and tendon transfer is used for active dorsiflexion.
Dr. Yash Mehta, Department of Orthopaedics, Apollo Hospitals, Navi Mumbai, Maharashtra, India. E-mail: yashmehtapanasonicp81@gmail.com
Introduction: Fixed Equinus deformity is characterized by limited dorsiflexion of ankle joint and restricted passive movement, along with medial and lateral tibiotalar instability, progressive hindfoot varus, and a supination deformity of the forefoot. Degree of equinus deformity is determined by the Tibio-Metatarsal (TM) angle, subtended between the longitudinal axes of Tibia and 1st Metatarsal, in lateral view of foot. Lambrinudi triple arthrodesis involves the surgical fusion of the talonavicular, talocalcaneal, and calcaneocuboid joints to correct fixed foot deformities, to relieve pain from joint, to provide stability to the imbalanced foot, and to create a plantigrade foot. We combined a Lambrinudi type arthrodesis with a transfer of the posterior tibial tendon (PTT) in adult patients to provide dynamic dorsiflexion and pronation.
Case Report: The case was of 39-year-old male diagnosed as fixed cavoequinus deformity of right foot and ankle, who was operated with Lambrinudi triple arthrodesis with PTT transfer in January 2019 and followed up to 5 years. Outcome measurements included radiographic and clinical investigations, including the TM Angle, American Orthopaedic Foot and Ankle Society (AOFAS) Score and Ankle range of motion (ROM), which were assessed preoperatively, immediate postoperatively, at 3 months, 6 months, 1 year, and 5 years.
Results: The TM angles were 177, 133, 125, and 122, at pre-operative, immediate post-operative, 3 months, 5 years, respectively. Fusion was seen at 1-year follow-up. Improvement in AOFAS Score with values 38, 57, 73, and improvement in Ankle ROM with values 0 (fixed), 10, 15° at pre-operative, 3 months, and 5 years postoperative, respectively. Patient could use ordinary footwear afterward and had no significant subjective pain or pain which affected his daily activities, but patient had post-procedural right lower limb shortening of 1 cm.
Conclusion: This combined procedure demonstrated clinical correction of foot deformity and significant improvement in functional outcome in the form of AOFAS score and Ankle ROM. The ability of all patients to use normal shoes and significant reduction in pain scores represent ultimately, the improvement in quality of life. We have corrected muscle imbalance and provided dynamic force for dorsiflexion and pronation of foot in the form of tibialis posterior.
Keywords: Fixed equinus deformity, lambrinudi triple arthrodesis, tibialis posterior tendon, tibio-metatarsal angle, American orthopaedic foot and ankle society score.
Fixed equinus or foot drop deformity refers to a condition characterized by limited dorsiflexion of the ankle joint and restricted passive movement, with subsequent shortening of the Achilles tendon that can be associated with stiffness of the ankle and hindfoot joints [1]. It is often associated with medial and lateral tibiotalar instability, progressive hindfoot varus, and a supination deformity of the forefoot. Along with stubbing of the forefoot during walking, patients also complain of painful overload in the lateral forefoot [1]. The instability and foot deformity may worsen over time as a result of gravity and a general decrease in muscular strength with aging, ultimately causing muscle imbalance. Adult drop-foot currently results from a lesion of the common peroneal nerve, L5 neuropathy, a partial sciatic nerve lesion, or lesions involving the lumbosacral plexus or cauda equina. This may occur post-traumatically (special cases of trauma such as gunshot wounds at the thigh level) [2], idiopathically, or as a result of a systemic disease such as diabetes mellitus, calcium metabolic disorders, and certain neuropathies. Degree of equinus deformity is determined by taking a lateral radiograph of the ankle region with the patient standing, and measuring the obtuse angle, which is called the Tibio-Metatarsal (TM) angle, subtended between the longitudinal axis of the tibia and that of the first metatarsal. As the degree of equinus deformity increases, the TM angle would correspondingly increases (Fig. 1 and 2).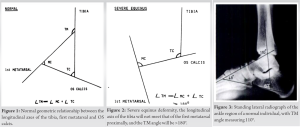
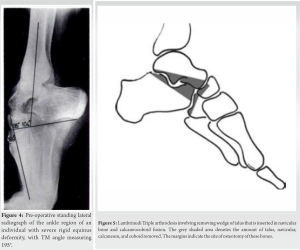
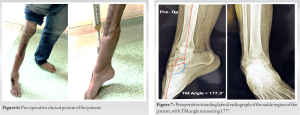
The case was done at Apollo Hospital, Navi Mumbai, India, in January 2019 and followed up to February 2024, approximately a span of 5 years. The prospective study comprised of 39-year-old male having history of severe crush injury to right lower limb in year 2011 with complete loss of muscles of anterior compartment of right leg. He had undergone multiple surgeries at Private Hospital and Medical College, Navi Mumbai, for the management of the same. Patient presented to us in January 2019 at Apollo Hospital, Navi Mumbai, with extensive scarring of right lower limb, extending 10 cm above knee to mid lower third of leg. There were deficient muscles in proximal anterior and lateral compartments and superficial posterior compartment of the Leg. He was diagnosed as fixed cavo-equinus deformity of right foot and ankle with no mobility with associated ankylosed right knee with no mobility (Fig. 6). Pt had difficulty in doing activities of daily living and used crutches for ambulation. He used to walk on toes with deformed supinated foot. The patient was evaluated on clinical and radiological basis preoperatively. For radiological investigations, X-ray foot (Lateral view in non-weight bearing) was done which measured the TM angle (between longitudinal axis of Tibia and 1st Metatarsal) to be 177.3° Obtuse (Fig. 7). Functional outcome measured by American Orthopaedic Foot and Ankle Society (AOFAS) score was 38 preoperatively and ankle range of motion (ROM) was minimal (Fixed 55° Plantarflexion) preoperatively. Informed consent was taken for the surgery.
Operative procedure
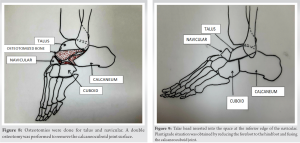
Patients were positioned supine with a thigh tourniquet. An 8–9 cm lateral incision was made, from the tip of the fibula, extending distally over the anterior process of the calcaneum, to the base of the lateral cuneiform bone, extending medially up to navicular tuberosity. The sinus tarsi and the bifurcate ligament were elevated to expose the subtalar and the talonavicular joint. As the foot was held in a neutral plantigrade position in the coronal plane, the osteotomies were done at inferior surface of talus and at superior surface of calcaneum (subtalar joint) with the help of an oscillating saw. A double osteotomy was performed to remove the calcaneocuboid joint surface (Fig. 8).
Post-operative protocol
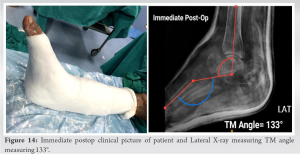
The foot was placed in a short leg cast after surgery for 3 weeks (Fig. 14). The cast was changed after 3 weeks under anesthesia, the new cast was applied in plantigrade position and partial weight bearing was allowed. Physiotherapy was prescribed after the cast immobilization was discontinued. At 4–6 months, the patients were allowed to perform full activities. Follow-up assessment was performed immediate postoperatively, at 3 months, 6 months, 1 year, and 5 years (Fig. 15-17).
Tourniquet minimized the average blood loss for Lambrinudi procedure with PTT transfer. Average duration for procedure was around 75 min.
Radiological:
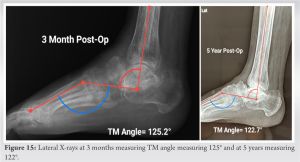
X-ray foot (Lateral View in Non weight bearing) was done in the immediate post-operative period, at 3 months and at 5-year follow-up, to evaluate the TM angle and radiological changes of intertarsal joints. The TM angles were 133, 125.2, and 122.7°, respectively (Fig. 15 and 16). Fusion was seen at 1-year follow-up.
Clinical
AOFAS score: On clinical evaluation, improvement in AOFAS scores was noted. AOFAS scores were 57 at 3 months and 73 at 5-year post-operative follow-up visits. Ankle ROM- Improvement in Ankle ROM with values 10° (10° Plantarflexion to 0° Dorsiflexion) at 3rd month and 15° (10° Plantarflexion to 5° Dorsiflexion) at 5-year postoperative, respectively (Figs. 17 and 18). Instability- Patient did not have any clinical instability of the ankle at follow-up. Infection: Patient did not have any superficial or deep infection. Presence of callosities: Patient had no significant callosities over the heads of the first and fifth metatarsals at follow-up. Shortening: Patient had post-procedural right lower limb shortening of 1 cm.
Subjective
Exercise tolerance and footwear: The patient had difficulty in using ordinary footwear before the operation because of his deformity, but he could use ordinary footwear afterwards. Pain: Before operation, patient had pain in the foot that limited his walking range. After he had no significant subjective pain or pain which affected his daily activities. General satisfaction: The patient was satisfied with the overall results of the operation.
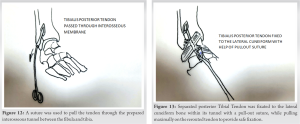
A combined procedure of a modified Lambrinudi arthrodesis with an additional PTT transfer provided a stable correction of the adult rigid drop-foot of patients with muscle imbalance. The additional PTT transfer performed by fixing the transferred tendon on the lateral cuneiform in maximal dorsiflexion of the foot lead to stable fixation and a dynamic dorsiflexor of foot. As the PTT transfer provides active dorsiflexion power, the patient returned to an almost normal life style and wearing normal footwear. The surgical options for equinus deformity correction include arthrodesis and the use of an external fixator. Arthrodesis has a lower risk of infection and a high degree of correction of varus and valgus deformities, providing realignment and gait improvement [6]. Furthermore, our results demonstrated that Lambrinudi arthrodesis preserved the tibiotarsal joint and therefore, can be used to correct severe, rigid hindfoot deformities at the transverse tarsal joint. Standard arthrodesis is associated with a loss of hindfoot motion that may lead to overuse of the neighboring joints and cause degenerative changes such as arthritis. Degeneration of the ankle joint is observed in approximately 30% of non-rheumatoid patients 5 years after fusion in studies by Knupp et al. [7] and Saltzman et al. [8]. However, the degree of bony correction in young children (i.e., the amount of the Lambrinnudi type wedge resection) is lesser than in an adult patient population. Hence, the combined procedure mentioned below can be safely performed in older patients. Most procedures involving the PTT transfer for the treatment of drop-foot deformity in adult patients include tendon transfer of the PTT alone to achieve active dorsiflexion. As described by Rodriguez [9] and Prahinski et al. [5]. Barr performed Anterior transfer of PTT by dissecting deep between the tendons of the anterior tibial muscle and the extensor hallucis longus; expose the interosseous membrane just proximal to the malleoli. It involves making a window in the interosseous membrane but avoid stripping the periosteum from the tibia or fibula. The PTT is passed through the window between the bones, taking care that it is not kinked, twisted, or constricted. Pass the tendon beneath the cruciate ligament, which can be divided if necessary to relieve pressure on the tendon [10-12]. Ober modified anterior transfer of PTT in which the Tendon and muscle is passed through anterior tibial compartment, and not through the interosseous membrane to dorsum of foot, and tendon then anchored in third metatarsal [13]. In patients with marked overpull of the posterior tibial muscle, Greene found that transfer of the PTT to the dorsum of the foot combined with other tenotomies or tendon lengthening gave better results than PTT lengthening alone. Although transfer of the PTT is technically more demanding and has a higher perioperative complication rate, Greene noted that the patients retained the plantigrade posture of their feet, even after walking ceased [14, 15]. Mubarak described transfer of the PTT to the dorsum of the base of the second metatarsal. Compared with the Greene technique, the more distal placement of the PTT increases the lever arm in dorsiflexion of the ankle and the technique allows easier plantarflexion and dorsiflexion balancing of the ankle at the time of surgery [16]. The split tendon transfer to the peroneus brevis, passing posterior to the tibia, was reported to give good results at 5-year follow-up [17]. Performing a soft-tissue procedure on the dorsal aspect of the foot can lead to wound healing problems. However, the tension in the soft tissue of the patient included in this study was not considered to be critical at the time of the wound closure, and postoperative dehiscence did not occur. In an attempt to achieve a plantigrade position, much of the talus had to be removed, together with resection of a big wedge of bone in the subtalar joint. This may lead to problems like avascular necrosis of the talus, non-union, or shortening of the foot, but in our case, we did not had any complication like AVN or non-union disproportionate shortening. Our results convincingly demonstrate improvement in function, and we are therefore encouraged to continue using the technique. Our results indicated significant improvement in the tibia-metatarsal angles, restoring the foot to an almost plantigrade position and preserving the tibiotarsal joint.
A combined procedure based on a modified resection arthrodesis initially described by Lambrinudi for the stable correction of the adult fixed equinus with severe hindfoot varus deformity demonstrated significant improvements of the AOFAS hindfoot score and ankle ROM. The ability of all patients to use normal shoes and significant reduction in pain scores represent ultimately, the improvement in quality of life. We have corrected muscle imbalance and provided dynamic force for dorsiflexion and pronation of foot in the form of tibialis posterior.
Single stage corrective osteotomy without any implant that healed in the plaster cast giving a plantigrade foot and muscle imbalance corrected by tendon transfer getting active dorsiflexion.
References
- 1.Elsner A, Barg A, Stufkens SA, Hintermann B. Lambrinudi Arthrodesis with posterior tibialis transfer in adult drop-foot. Foot Ankle Int 2010;31:30-7. [Google Scholar]
- 2.Hamdan FB, Jaffar AA, Ossi RG. The propensity of common peroneal nerve in thigh-level injuries. J Trauma 2008;64:300-3. [Google Scholar]
- 3.Tang SC, Leong JC, Hsu LC. Lambrinudi triple arthrodesis for correction of severe rigid drop-foot. J Bone Joint Surg Br 1984;66:66-70. [Google Scholar]
- 4.Lambrinudi C. New operation of drop-foot. Br J Surg 1927;15:193-200. [Google Scholar]
- 5.Prahinski JR, McHale KA, Temple HT, Jackson JP. Bridle transfer for paresis of the anterior and lateral compartment musculature. Foot Ankle Int 1996;17:615-9. [Google Scholar]
- 6.Gunther GD, Sérgio DS, Fabio F, Rizzo MA. Clinical and functional outcomes of patients with tibiotarsal arthrodesis in foot drop treatment. Rev ABTPé 2016;10:1-5. [Google Scholar]
- 7.Knupp M, Skoog A, Törnkvist H, Ponzer S. Triple arthrodesis in rheumatoid arthritis. Foot Ankle Int 2008;29:293-7. [Google Scholar]
- 8.Saltzman CL, Fehrle MJ, Cooper RR, Spencer EC, Ponseti IV. Triple arthrodesis: Twenty-five and forty-four-year average follow-up of the same patients. J Bone Joint Surg Am 1999;81:1391-402. [Google Scholar]
- 9.Rodriguez RP. The bridle procedure in the treatment of paralysis of the foot. Foot Ankle 1992;13:63-9. [Google Scholar]
- 10.Barr JS. Transference of Posterior Tibial Tendon for Paralytic Talipes Equinovarus. Personal Communication; 1954.(Campbell Operative orthopaedics 13e) [Google Scholar]
- 11.Barr JS, Record EE. Arthrodesis of the ankle for correction of foot deformity. Surg Clin North Am 1947;27:1281-8. [Google Scholar]
- 12.Barr JS, Record EE. Arthrodesis of the ankle joint; indications, operative technic and clinical experience. N Engl J Med 1953;248:53-6. [Google Scholar]
- 13.Ober FR. Tendon transplantation in the lower extremity. N Engl J Med 1933;209:52-9. [Google Scholar]
- 14.Greene WB. Transfer versus lengthening of the posterior tibial tendon in Duchenne’s muscular dystrophy. Foot Ankle 1992;13:526-31. [Google Scholar]
- 15.Green WT, Grice DS. The surgical correction of the paralytic foot. Instr Course Lect 1953;10:343. [Google Scholar]
- 16.Mubarak SJ, Morin WD, Leach J. Spinal fusion in Duchenne muscular dystrophy--fixation and fusion to the sacropelvis? J Pediatr Orthop 1993;13:7562. [Google Scholar]
- 17.Kling TF Jr., Kaufer H., Hensinger RN. Split posterior tibial-tendon transfers in children with cerebral spastic paralysis and equinovarus deformity. J Bone Joint Surg Am 1985;67:186-94. [Google Scholar]