“Double hit” mechanism of fracture pattern and corticosteroid usage the potential contributing factors of ON.
Dr. Kenneth A. Egol, NYU Langone Orthopedic Hospital, 301 E 17th street, New York, NY; Jamaica Hospital Medical Center, 8900 Van Wyck Expressway, Queens, New York. E-mail: Kenneth.egol@nyulangone.org
Introduction: Osteonecrosis (ON) of the humeral head is defined as “avascular” when the death of bone is due to a disrupted blood supply. It is a known complication following proximal humeral fractures and can lead to poor long-term outcomes and even additional revision surgeries.
Case Report: Patient AP developed symptomatic ON, 3 years following repair of a 4-part valgus impacted proximal humerus fracture. The point of interest in this case is the length of time from injury at which she developed symptomatic ON. Following surgical repair, she was seen at standard intervals, 6 weeks, 3-, 6-, and 12- month follow-ups and demonstrated an excellent recovery. By the 1 year follow-up appointment, she had obtained a range of motion in her left shoulder of 170° forward elevation and 60° in external rotation. At this point, she was able to discontinue physical therapy and was radiographically and clinically healed. However, 2 years after, she began experiencing sudden onset of pain with shoulder ROM and progressive limitation. She was diagnosed with an ON of her proximal humerus. The patient was prescribed a 3-month course of corticosteroid, 3 months following her operation for a gynecological-related issue. However, with strong progress being made 9 months after this prescription, and problems occurring over 2 years after taking the medication, it is unclear whether the ON was related to her fracture pattern or developed as a result of the corticosteroid usage or a combination of the 2 due to a “double hit.”
Conclusion: This case review points out the potential need for continued monitoring even after radiographic and clinical healing is achieved in these injuries.
Keywords: blood supply, delayed presentation, osteonecrosis, proximal humerus fracture, corticosteroid
Second to the femoral head, the humeral head is known to be the second most common site of osteonecrosis [1]. There is little known about the pathogenesis of osteonecrosis; however, the pathway is known to result in disrupted blood supply, increased intraosseous pressure, and eventually bone death [2, 3]. Osteonecrosis of the humeral head is an uncommon condition and can be difficult to recognize due to non-specific initial symptoms. Radiography is the main tool used stage disease progression [4]. That said, radiographic findings in the initial stage of osteonecrosis are nearly normal. We report a case of a 70-year-old female who presented with shoulder pain and limited range of motion 3 years post open reduction and internal fixation of her proximal humerus. The shoulder is highly susceptible to osteoarthritis which is known to be the most common cause of shoulder pain and limited range of motion [5]. Osteonecrosis can also lead to joint pain but is less common. In most cases, trauma is the cause of osteonecrosis. However, atraumatic necrosis can develop in patients with risk factors such as corticosteroid administration, heavy alcohol intake, rheumatoid arthritis, and systemic lupus erythematous [4].
The patient is a 70-year-old female who presented to the outpatient clinic 3 weeks after falling down a staircase. She postponed her appointment due to fear of contracting COVID during her medical examination. She was diagnosed with a displaced 4-part valgus impacted proximal humerus fracture (Fig. 1) and has a medical history of GERD, hyperlipidemia, and cholecystectomy. She had no medical conditions, nor took any medications associated with ON. On initial physical examination, moderate ecchymosis was noted along with limited active and passive motion. Motor and vascular examinations were normal.
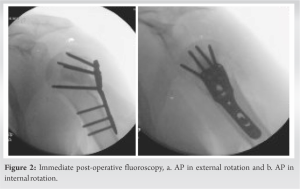
She was indicated for open reduction and internal fixation to repair the fracture, with the option for reverse total shoulder arthroplasty (RTSA) if unreconstructable. The procedure was performed through a deltopectoral incision. The biceps tendon was noted to be intact. The rotator cuff was noted to be torn. A biceps tenodesis was performed and the humeral head was reduced to the shaft and the tuberosities reconstructed around the elevated head. The fracture reduction was assessed as near anatomic and a three-hole proximal humerus locking plate applied laterally and fixed with six unicortical locking screws into the head, two bicortical locking screws, and one non-locking screw into the shaft. The large void was filled with 10 cc calcium-phosphate cement. At this point, intraoperative fluoroscopy was used to obtain AP, internal and external rotation views, and axillary views which confirm reduction and the absence of articular penetration of the screws (Fig. 2). Number 5 braided, non-absorbable suture was passed through the rotator cuff tendon and passed through the plate to further secure the fixation. The shoulder was then put through range of motion and found to be full. The wound was closed with suture. The post-operative plan was for the early range of shoulder motion, antibiotics, and DVT prophylaxis.
At 3, 6, and 12 months post-operative, patient AP was progressing well. She demonstrated progressively increased range of shoulder motion. X-ray images of her left shoulder demonstrated a healed fracture in acceptable alignment (Fig. 3). No radiographic complications were found. Three months post-operative, she was started on prasterone by her gynecologist for vaginal atrophy. She was kept on the medication for 3 months. At 1-year post-operative, she was found to have recovered near full range of shoulder motion.
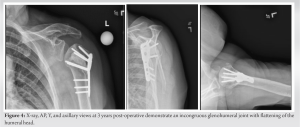
The patient returned at 3 years with a 2-month new-onset shoulder pain with reaching activities and decreased left shoulder range of motion. She did not report any new trauma or inciting event. Range of motion of her left shoulder was forward elevation 160°, external rotation 45° and internal rotation to T12. Her range of motion was painful at terminal range of motion and decreased compared to the contralateral side. Imaging data of her left shoulder demonstrated altered contour of the humeral head consistent with development of osteonecrosis (Fig. 4). There was no screw penetration or other evidence of hardware complication. The glenohumeral joint remained reduced, but incongruent.
Osteonecrosis of the humeral head is a rare, but well-known complication of proximal humerus fractures [6]. In this case report, we present a unique case of a healthy 70-year-old woman who developed ON 3 years following open reduction and internal fixation of her proximal humerus. The patient had a normal recovery following her initial surgery and had achieved a range of motion of 170° forward elevation and 60° in external rotation. At the time of her last fracture follow-up appointment, she was considered to be radiographically and clinically healed. However, 2 years after her last follow-up appointment, she began experiencing pain during range of motion, and subsequent imaging revealed ON in her proximal humerus. The pathogenesis of osteonecrosis is not well understood, but it is thought to result from disrupted blood supply, increased intraosseous pressure, and eventual bone death [2, 3]. Trauma is the most common cause of osteonecrosis, but atraumatic necrosis can also occur in patients with certain risk factors such as corticosteroid administration, heavy alcohol intake, rheumatoid arthritis, and systemic lupus erythematosus [4]. In this case, the patient was prescribed a corticosteroid known as prasterone to treat vaginal atrophy by her gynecologist 3 months after her operation. It is not known how long she was taking the medication for; however, it was prescribed nightly for 90 days. It is important to note that this certainly could have been a contributing factor to the patient’s presentation of ON 3 years post-operative, but the development of symptoms and radiographic changes occurred more than 2.5 years following cessation of the medication. Osteonecrosis of the humeral head is difficult to diagnose in the early stages because radiographic findings may appear normal [4]. However, as the disease progresses, radiographs can reveal findings such as subchondral sclerosis, flattening of the articular surface, and cyst formation [7]. Magnetic resonance imaging (MRI) is a sensitive tool for detecting early-stage ON, and it is recommended in cases where there is a high clinical suspicion of osteonecrosis [8]. In this case, the patient presented with shoulder pain and limited range of motion, which are non-specific symptoms that can be attributed to a variety of shoulder conditions. It was not until imaging was performed that ON was diagnosed. It is possible that the ON developed earlier but was not symptomatic until much later.
The treatment of osteonecrosis depends on the stage of the disease, and early diagnosis is important for successful management [9]. In the early stages of the disease, conservative measures such as analgesics, non-steroidal anti-inflammatory drugs, and physical therapy may be sufficient [10]. However, in advanced stages, surgical management such as joint-preserving procedures, total joint replacement, or revascularization procedures may be necessary. It is possible that the development of ON at this late stage was a consequence of a “double hit to the blood supply.” In general, a double hit phenomenon refers to nerve compression at distinct time periods and different locations that act synergistically to increase symptom intensity [11]. We theorize that the delayed incidence of ON in this patient occurred due to a double hit of initial proximal humerus fracture following corticosteroid intake. While there is a different biological mechanism underlying each “double hit” case, they entail the same conceptual sequential and synergistic impact of two biological triggers leading to a serious medical complication. Therefore, we propose a new definition for a “double hit to the blood supply” and propound a mechanism in which bone fracture and subsequent corticosteroid intake leads to osteonecrosis.
Osteonecrosis of the humeral head is a known complication that can occur following proximal humeral fractures. This case report highlights the importance of the coordination of care between medical specialists to prevent harmful outcomes of treatment that impacts a patient beyond the scope of a specialist’s area. In addition, it underlines the importance of continuing to monitor a musculoskeletal condition even after radiographic and clinical healing is achieved in these injuries when clinical symptoms warrant. The patient in this report developed symptomatic osteonecrosis 3 years following the repair of a 4-part valgus impacted proximal humerus fracture. The case emphasizes the fact that the potential for osteonecrosis is still present even several years following the initial injury. Clinicians should be aware of the risk factors associated with osteonecrosis and counsel patients accordingly. Despite the best efforts, osteonecrosis can still occur, and patients should be informed of the risks associated with surgery. While ON may be unavoidable and associated with poorer outcomes following fracture repair, many patients can still have a successful outcome. The case report also emphasizes the importance of considering osteonecrosis as a potential cause of shoulder pain and limited range of motion in patients long after fixation of a proximal humerus fracture, especially in those with risk factors such as corticosteroid administration (as seen in this patient), heavy alcohol intake, rheumatoid arthritis, and systemic lupus erythematosus. Early diagnosis and treatment can prevent further progression of the disease and improve outcomes for these patients.
In this case report, we describe a “double hit” exposure of the proximal humerus to osteonecrosis involving a combination of bone fracture and subsequent corticosteroid intake. While there is a different biological mechanism underlying each one of the two “hits,” they entail the same conceptual sequential and synergistic impact of two biological triggers leading to this serious clinical condition. The novelty of this case involves the significantly delayed onset of ON following fracture, corticosteroid usage, as well as radiographic and clinical healing. This time sequence has not previously been described in medical literature.
References
- 1.Hernigou P, Hernigou J, Scarlat M. Shoulder osteonecrosis: Pathogenesis, causes, clinical evaluation, imaging, and classification. Orthop Surg 2020;12:1340-9. [Google Scholar]
- 2.Kiaer T, Pedersen NW, Kristensen KD, Starklint H. Intra-osseous pressure and oxygen tension in avascular necrosis and osteoarthritis of the hip. J Bone Joint Surg Br 1990;72:1023-30. [Google Scholar]
- 3.Matthews AH, Davis DD, Fish MJ, Stitson D. Avascular necrosis. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537007 [Last accessed on 2022 Nov 14]. [Google Scholar]
- 4.Byun JW, Shim JH, Shin WJ, Cho SY. Rapid progressive atypical atraumatic osteonecrosis of humeral head: A case report. Korean J Anesthesiol 2014;66:398-401. [Google Scholar]
- 5.Precerutti M, Formica M, Bonardi M, Peroni C, Calciati F. Acromioclavicular osteoarthritis and shoulder pain: A review of the role of ultrasonography. J Ultrasound 2020;23:317-25. [Google Scholar]
- 6.Schmalzl J, Graf A, Kimmeyer M, Gilbert F, Gerhardt C, Lehmann LJ. Treatment of avascular necrosis of the humeral head - Postoperative results and a proposed modification of the classification. BMC Musculoskelet Disord 2022;23:396. [Google Scholar]
- 7.Enge DJ Jr., Fonseca EK, Castro AA, Baptista E, Santos DC, Rosemberg LA. Avascular necrosis: Radiological findings and main sites of involvement - pictorial essay. Radiol Bras 2019;52:187-92. [Google Scholar]
- 8.Manenti G, Altobelli S, Pugliese L, Tarantino U. The role of imaging in diagnosis and management of femoral head avascular necrosis. Clin Cases Miner Bone Metab 2015;12:31-8. [Google Scholar]
- 9.Steinberg ME. Early diagnosis of avascular necrosis of the femoral head. Instr Course Lect 1988;37:51-7. [Google Scholar]
- 10.Martí-Carvajal AJ, Solà I, Agreda-Pérez LH. Treatment for avascular necrosis of bone in people with sickle cell disease. Cochrane Database Syst Rev 2019;12:CD004344. [Google Scholar]
- 11.Kane PM, Daniels AH, Akelman E. Double crush syndrome. J Am Acad Orthop Surg 2015;23:558-62. [Google Scholar]