Knowledge of an underlying bone tumor presenting as a skin lesion is an invaluable pearl of knowledge when evaluating dermatologic conditions, particularly of the hand and foot, as failure to recognize an underlying bone tumor presenting as a skin lesion can lead to a delay in diagnosis and if the tumor is malignant, this can lead to loss of limb or life.
Dr. Bruce E Heck, Department of Orthopedic Surgery, Northwest Ohio Orthopedics and Sports Medicine, Findlay, Ohio, USA. E-mail: drbruceheck@gmail.com
Introduction: Osteochondromas are the most common benign tumors of the bone and can be sessile or pedunculated. Although osteochondromas are typically seen in the long bones, they are rarely seen in the small bones of the hand or foot. Verruca vulgaris, also known as the common wart, is one of the most common skin conditions presenting to physicians and must be distinguished either clinically or histologically from other hyperkeratotic conditions, including bone conditions such as bone tumors that can place pressure on the skin and cause callus formation that can mimic a wart or create skin deformity. A high index of suspicion for underlying bone mass or tumor should be entertained when evaluating patients for skin conditions, particularly of the hand or foot, with failure to improve with treatment.
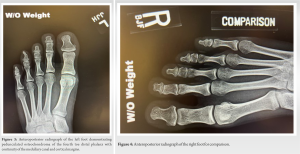
Case Report: This case report presents a 20-year-old male with a pedunculated osteochondroma of the left fourth distal phalanx with hyperkeratotic skin overlying the mass at the end of the toe. He was initially treated by a family doctor and podiatrist for verruca vulgaris for over 5 years with two treatments of liquid nitrogen cryotherapy and surgical excision of the mass when the treating podiatrist encountered bone and recommended radiographs. The family requested follow-up with our practice several days later after they were told the patient had a bone tumor. The patient requested surgical excision of the osteochondroma secondary to pain with activities and difficulties with his vocation as a pilot.
Conclusion: All physicians must be mindful of an underlying bone tumor or mass in patients presenting with skin changes, particularly about the foot or hand. Knowledge that an underlying bone tumor can present as a verruca vulgaris may prevent a delay in diagnosis or unnecessary treatment when evaluating and treating a patient with a skin lesion. Fortunately, our case was a benign osteochondroma; a malignant tumor with a delay in diagnosis could lead to loss of limb or life.
Keywords: Osteochondroma, verruca vulgaris, skin changes, exostosis, bone tumor, wart.
Osteochondromas are the most common benign tumors that present as a cartilage-capped bony projection that can be sessile or pedunculated [1]. Although osteochondromas are typically seen in long bones and rarely seen in smaller bones, rare presentations include flat bones, the body of the pelvis, scapula, skull, and small bones of the hand and foot [2]. Two pathognomonic features that ascertain the diagnosis are the presence of cortical and medullary continuity with the parent bone and a cartilage cap [3, 4]. Most lesions are solitary, but approximately 15% of the patients have multiple tumors, which can be hereditary multiple exostoses (HME), also known as multiple hereditary osteochondromas, multiple osteochondromas, hereditary deforming dyschondroplasia, diaphyseal aclasis, and multiple cartilaginous exostoses, a rare genetic disorder that is inherited in an autosomal dominant manner with an increased risk of tumor malignant transformation to chondrosarcoma [5,6]. It has been reported that malignant transformation occurs in approximately 1% of solitary osteochondromas and 10% of HME cases [1]. Most patients with HME have germ line mutations in the tumor suppressor genes exostosin 1 (EXT1) or exostosin 2 (EXT2) [6-8]. The EXT genes encode glycosyltransferases, catalyzing heparan sulfate polymerization [6]. Traditionally, most osteochondromas are diagnosed incidentally as they are asymptomatic [1,9]. Osteochondromas that present with symptoms are usually painful due to compression of adjacent structures, including the nerve, artery, and bursa; bony deformity with or without limb malignment; fracture of the stalk of the osteochondroma; and malignant transformation [1,9,10]. Plain radiographs are usually sufficient to diagnose osteochondromas; however, cross-sectional imaging such as computerized tomography and magnetic resonance imaging (MRI) are used to evaluate the cartilage cap, where increased thickness has been associated with cancerous degeneration, evaluate tumors in areas of complex anatomy, and evaluate marrow continuity to confirm diagnosis [9]. Asymptomatic lesions with no concerns of malignancy are treated solely with observation, while surgical resection is indicated for symptomatic lesions, cosmesis, or lesions with suspicious imaging findings of malignant transformation [9]. Excision of the tumor with a free margin, without leakage of myxomatous tissue or part of the cartilaginous cap, is the treatment of choice [9]. Local recurrence is <2% if a complete resection is achieved [11]. Verruca vulgaris (common wart) is an epidermal thickening and hyperkeratinization of the skin following infection of the keratinocytes at the basal layer of the epidermis with the human papilloma virus (HPV), resulting in clonal proliferation and a visible wart [12,13]. With classification based on variation of the viral DNA, there are more than 150 genotypically distinct types of HPV. Most common warts are caused by HPV types 1, 2, 4, 27, or 57 and present with pain on pressure or an esthetic problem [12,13]. Although diagnosis of common hand and foot warts is easily made by visual inspection or paring down of the wart to pinpoint bleeding as the capillary loops of the elongated dermal papillae are exposed, warts must be distinguished either clinically or histologically from other keratotic lesions on the hands or feet, such as actinic keratoses, knuckle pads, corns, calluses, lichen planus, angiokeratoma, seborrheic keratoses, focal palmoplantar keratoderma, and squamous cell carcinoma, which has been associated with HPV infections [13]. Treatment includes observation and destruction by a variety of means, including chemical and surgical means (salicylic acid/cryotherapy), destruction by surgical means (scalpel/cautery/laser), virucidal agents (formaldehyde/glutaraldehyde), antiproliferative agents (vitamin D/5-fluorouracil), immunological agents (imiquimod/intralesional candida), and complementary and alternative treatments (hypnosis/herbal/homeopathic/acupuncture) [12,13]. This case report presents a rare case of a pedunculated osteochondroma arising from the left fourth distal phalanx in a 20-year-old college student after 5 years of intermittent treatment by two physicians as well as an attempted surgical excision by the patient for verruca vulgaris. The treatment included two cryotherapy treatments with liquid nitrogen and a surgical excision from the podiatrist before referral. The report highlights the importance of recognizing osteochondromas arising from rare locations and more vitally alerts all physicians to be mindful of an underlying bone tumor or mass in patients presenting with skin changes, particularly of the hand or foot, and to obtain radiographic studies to prevent a delay in diagnosis or treatment.
A 20-year-old male college aviation student sought care for chronic, left, fourth-toe pain with activities of daily living and pain with pressure over the distal end of the affected toe. The patient complained mostly when working the rudders on the control center of the airplane, when he would bump the toe. His past medical history was unremarkable, except for seasonal allergies. He was on no medication. 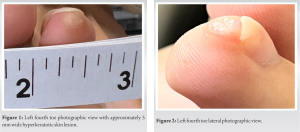

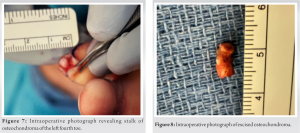
The patient was taken to surgery 3 days after the initial visit, once surgical preparation was complete. Pre-operatively, the patient received Ancef 2 g intravenously. He had general laryngeal mask anesthesia in the supine position, received antibiotics, and had his affected foot prepped and draped. Thromboembolic stockings and compression pumps were placed on the non-operative side. The patient had a tourniquet applied to the base of the left fourth toe. Initially, C-arm fluoroscopic images taken intra-operatively were utilized to localize the osteochondroma, and the images were saved. An excisional biopsy (5 × 5 mm) of the hyperkeratotic skin was performed under a toe tourniquet, discussed with the pathologist, and sent for histopathologic evaluation to rule out squamous cell carcinoma and further investigation by the Mayo Clinic to rule out HPV. Next, utilizing a new scalpel and re-prepping the site, a curvilinear incision at the tip of the toe was made. The volar half of the skin and subcutaneous tissue were retracted plantar, and surgery was performed under 3.5 mm loupe magnification. A cartilage cap consistent with osteochondroma was exposed (Fig. 6). Exposure of the stalk of the osteochondroma continuous with the tuft of the distal phalanx was performed (Fig. 7).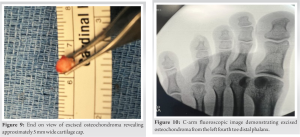
Osteochondromas, despite being the most common benign bone tumor, are rarely seen in the small bones of the hand and foot [1,2]. Common warts (verruca vulgaris) are one of the most common complaints in routine dermatological practice [12]. Although verruca vulgaris is a common presentation to physicians, warts must be distinguished either clinically or histologically from other keratotic lesions on the hands or feet, such as actinic keratoses, knuckle pads, corns, calluses, lichen planus, angiokeratoma, seborrheic keratoses, focal palmoplantar keratoderma, and squamous cell carcinoma, which has been associated with HPV infections [13]. Also, the differential should include underlying bone tumors, as shown in our case. Unfortunately, our patient had chronic symptoms related to osteochondroma of his left fourth toe since he was 7 years old. This is not surprising, as most osteochondromas present in children or adolescents are painless masses and are found incidentally unless they are in a location to have pressure, as occurred in our case when kicking the soccer ball [9]. Even more unfortunate, the diagnosis would take over 5 years, with a delay in diagnosis and maltreatment from several physicians before receiving proper care. Although it is well documented in the literature that osteochondromas can present with symptoms of pain due to compression of adjacent structures including the nerve, artery, and bursa, bony deformity with or without limb malignment, fracture of the stalk of the osteochondroma, and malignant transformation [1,9,10], this is the first case report of an osteochondroma of the distal phalanx of the toe presenting as verruca vulgaris to our knowledge. Interestingly, there has been a unique skin change described with a V-shaped skin depression on the palmar side of the proximal interphalangeal joint of the right middle finger during finger locking in a 50-year-old related to an osteochondroma [14]. Fortunately, our patient had a benign bone tumor as the underlying cause of his skin thickening and pain to the pressure at the tip of his toe, as a delay in diagnosis with an underlying malignant tumor could lead to loss of limb or life. Although it was possible that the patient could have had an underlying bone tumor and verruca vulgaris at the same time, it was clear based on histopathology that there was no verruca vulgaris as the cause of skin thickening. Also, the failure to improve with cryotherapy and surgical excision of the wart, the hard quality to palpation of the skin mass, and the diffuse skin changes should tip the clinician to suspect another diagnosis. In retrospect, the treating physicians should have maintained a high index of suspicion for underlying osteochondroma and obtained radiographs, which would have led to the correct diagnosis.
This case report highlights the importance of physicians being mindful of an underlying bone tumor or mass in patients presenting with skin changes, particularly about the foot or hand. Knowledge that an underlying bone tumor can present as a verruca vulgaris may prevent a delay in diagnosis or unnecessary treatment when evaluating and treating a patient with a skin lesion. Fortunately, our case was a benign osteochondroma; a malignant tumor with a delay in diagnosis could lead to loss of limb or life.
All physicians must be mindful of an underlying bone tumor or mass in patients presenting with skin changes, particularly about the foot or hand. Radiographs should be obtained when evaluating a patient with a skin lesion of the hand or foot to prevent a misdiagnosis or a delay in diagnosis, particularly when they do not respond to treatment. Knowledge that an underlying bone tumor can present as verruca vulgaris may prevent a delay in diagnosis or unnecessary treatment when evaluating and treating a patient with skin lesions.
References
- 1.Tepelenis K, Papathanakos G, Kitsouli A, Troupis T, Barbouti A, Vlachos K, et al. Osteochondromas: An updated review of epidemiology, pathogenesis, clinical presentation, radiological features and treatment options. In Vivo 2021;35:681-91. [Google Scholar]
- 2.Khodnapur G, Kulkarni S, Patil V, Venkat M, Basavaraj MK. Case series - Osteochondromas at rare locations. J Orthop Case Rep 2023;13:74-80. [Google Scholar]
- 3.Motamedi K, Seeger LL. Benign bone tumors. Radiol Clin North Am 2011;49:1115-34, v. [Google Scholar]
- 4.Alyas F, James SL, Davies AM, Saifuddin A. The role of MR imaging in the diagnostic characterisation of appendicular bone tumours and tumour-like conditions. Eur Radiol 2007;17:2675-86. [Google Scholar]
- 5.Bovee JV. Multiple osteochondromas. Orphanet J Rare Dis 2008;3:3. [Google Scholar]
- 6.D’Arienzo A, Andreani L, Sacchetti F, Colangeli S, Capanna R. Hereditary multiple exostoses: Current insights. Orthop Res Rev 2019;11:199-211. [Google Scholar]
- 7.Yang C, Zhang R, Lin H, Wang H. Insights into the molecular regulatory network of pathomechanisms in osteochondroma. J Cell Biochem 2019;120:16362-9. [Google Scholar]
- 8.Pacifici M. Hereditary multiple exostoses: New insights into pathogenesis, clinical complications, and potential treatments. Curr Osteoporos Rep 2017;15:142-52. [Google Scholar]
- 9.Kitsoulis P, Galani V, Stefanaki K, Paraskevas G, Karatzias G, Agnantis NJ, et al. Osteochondromas: Review of the clinical, radiological and pathological features. In Vivo 2008;22:633-46. [Google Scholar]
- 10.Khare GN. An analysis of indications for surgical excision and complications in 116 consecutive cases of osteochondroma. Musculoskelet Surg 2011;95:121-5. [Google Scholar]
- 11.Garrison RC, Unni KK, McLeod RA, Pritchard DJ, Dahlin DC. Chondrosarcoma arising in osteochondroma. Cancer 1982;49:1890-7. [Google Scholar]
- 12.Mursic I, Vcev A, Kotrulja L, Kuric I, Milavic T, Sustic N, et al. Treatment of verruca vulgaris in traditional medicine. Acta Clin Croat 2020;59:745-50. [Google Scholar]
- 13.Sterling JC, Gibbs S, Haque Hussain SS, Mohd Mustapa MF, Handfield-Jones SE. British association of dermatologists’ guidelines for the management of cutaneous warts 2014. Br J Dermatol 2014;171:696-712. [Google Scholar]
- 14.Yabumoto T, Endo T, Itoga R, Kawamura D, Matsui Y, Iwasaki N. Unique skin findings in a case of the A3 pulley trigger finger due to an osteochondroma. Jt Dis Relat Surg 2024;35:249-53. [Google Scholar]