Native ipsilateral palmaris longus tendon can be used to encircle the raw surface of ulna, following the synostosis excision, as a novel method to prevent recurrence and re-ossification in cases with radioulnar synostosis.
Dr Ganesh Singh Dharmshaktu, Department of Orthopaedics Surgery, Government Medical College Haldwani, Uttarakhand, India. Email: drganeshortho@gmail.com
Introduction: Radioulnar synostosis is an uncommon complication of forearm fractures and presents with varying degrees of restricted forearm movement. The diaphysial distal third synostosis is less common and excision of the synostosis is fraught with risk of re-ossification. Use of inert or biological interposing material has thus been accompanied with the synostosis excision and various methods have been described. There is still no consensus on the ideal treatment method.
Case Report: We, hereby, report a case of a long-standing radioulnar synostosis with rotational restriction of movement. Despite the movement restriction, the patient could perform basic activities of daily living and wanted to improve the movements. The presence of diaphyseal radioulnar synostosis was conformed on the radiographs and computerized tomography scan. A volar forearm approach was used and the bony bridge was excised. The ipsilateral native palmaris longus (PL) tendon was extracted from distal wrist crease and with its proximal attachment intact, circumferentially wrapped around the ulnar raw surface as an interposing material. Apart from this, free fat was also placed at the synostosis site. In the long-term follow-up of 10 years, there was no radiological evidence of re-ossification noted. The clinical improvement was not much but the patient was performing activities of daily living with no discomfort.
Conclusion: The use of an encircling loop of the native PL tendon, over the raw surface of one of the forearm bones, may be another useful method to decrease the chances of recurrence following the excision of the synostosis.
Keywords: Post-traumatic synostosis, radioulnar synostosis, excision, forearm bone synostosis, heterotopic ossification, management.
Post-traumatic radioulnar synostosis is a rare disabling complication following prior fractures of forearm bones that hinder forearm rotational movements [1]. There are cases reported both following the conservative and the surgical intervention of the forearm fractures. Delayed open reduction, bone fragments left in the interosseous space and bone screws breaching opposite cortex have been described as common causative factors. Vince and Miller classified radioulnar synostosis on the basis of their location into three types (Type 1: Involving distal intra-articular region, Type 2: Diaphyseal, and Type 3: Involving the proximal third forearm) [2]. Higher incidence of the synostosis is noted in cases with proximal third forearm fractures and when single incision is used for fixing both bone forearm fractures [3]. The risk of developing this complication can be attributed to the trauma itself or to the subsequent surgical intervention. Early recognition and treatment leads to good outcome but consensus on the diagnosis, timing of surgery and management is nonexistent [4]. As there is no therapeutic consensus, various treatment methods have been described [3, 4]. The excision of the synostosis and placement of some interposition material has been described frequently, followed by early postoperative physiotherapy leading to the optimal outcome [5]. The types of material used may be biological or synthetic graft and in certain instances, vascularized or non-vascularized tissues have also been utilized [1, 4, 5]. Surgeon preference and availability of the material may impact the treatment choice, but use of native tendon like palmaris longus (PL) can be a good alternative.
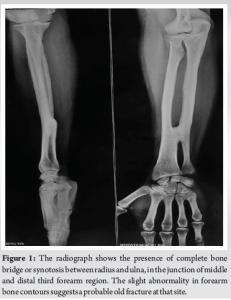
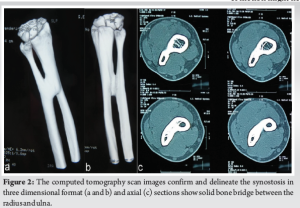
A 30-year-old male patient presented to us with right side restricted forearm movement following a history of the right forearm bone injury treated conservatively with plaster splint 15 years back. No documentary records or radiographs were available with the patient. On examination, there was no apparent forearm deformity noted but the right-sided forearm had fixed forearm pronation deformity with forearm fixed in mid-prone position with no further active or passive pronation. The supination was also restricted with only 15° of supination possible, thus an arc of 15° of forearm movement was noted in the right side as compared to the normal contralateral side. Bilateral elbow and shoulder movements were normal and no distal neuromuscular deficit was noted. The forearm radiographs revealed a complete radioulnar synostosis between radius and ulna diaphysis in the distal third region (Fig. 1). The solid bony-bridge was the reason behind the restricted forearm rotational movements. There was some abnormality in the outer contours of both bones of the forearm around the synostosis site suggesting some malunion of the previous fracture. Three-dimensional rendition of computerized tomogram scan further delineated the lesion in dorsal and volar aspect and also in axial views (Fig. 2). The patient wanted to improve prono-supination, but he was explained that full range of motion might not be guaranteed as the deformity was long standing. Besides that, possibility of inadvertent fracture of forearm bones was explained as a rare intraoperative complication. Following the informed consent, the plan to excise the bony bridge was made. The synostosis was approached with the volar Henry’s incision, and the complete identification of the synostosis was done. Following the multiple tiny drill-holes along the bridge, careful use of osteotome was done to connect the drill holes, and the bony bridge was excised completely (Fig. 3a). After the excision of the bony bridge, through saline wash was done to remove bone debris and hemostasis was achieved. The ipsilateral PL tendon was identified and harvested through a small incision distally over the volar wrist crease and was extracted proximally through the surgical site (Fig. 3b). The tendon was kept intact at the proximal site. The tendon was looped multiple times and encircled the raw surface of ulna before stitching the end to the tendon itself for a secure and stable coverage (Fig. 3c and d). After the tendon loop, some free fat from the subcutaneous layer was filled in the gap. The step was done to provide an interposition structure to prevent chances of re-ossification before the wound was closed in layers. The intraoperative regain of movement was not much and only 20° was gained from the pre-operative status and that too only in supination. Pronation was also improved by only 10°. Fearing inadvertent breakage of bones, no further attempts to improve the movement by manual force was exercised. The fascia was not stitched tightly to decrease chances of increased compartmental pressure due to potential post-surgery swelling. The wound healed uneventfully and early physiotherapy was initiated. The patient was lost to follow-up after 5 days and could not be traced for many years. He was also non-compliant to regular physiotherapy. The movements, however, were not improved and when compared to the status on presentation (Fig. 4a and b) were only 20° improvement in supination was noted (Fig. 4c and d). He reappeared after 10 years and the radiographs were done and confirmed no re-ossification (Fig. 4e). He, however, could perform most of the activities of daily living. One of the reasons for his non-compliance to the follow-up was that he was a skilled worker and busy in his vocation. Despite the suboptimal functional result, this report describes a novel interposition technique of PL graft, wrapping around one bone over the site of excised synostosis. This method may serve as another adjunct option in the management of diaphyseal radioulnar synostosis.

The post-traumatic radioulnar synostosis is an uncommon complication, usually reported following the forearm bone fractures [1, 2, 3, 5]. Most of the reported synostosis is noted in proximal forearm region while the diaphysial lesions are uncommon. The diaphyseal lesions are type 2 as per the classification given by Vincent and Miller [2, 4, 5]. The radioulnar synostosis is seen commonly in cases with high energy forearm fracture, extensive soft tissue or burn injury, and concomitant head or neurological injury. Other factors associated are the presence of comminuted forearm fracture, delayed surgery, single incision used for fixing both bone fractures, prolonged immobilization or delayed rehabilitation [6]. As our case had a history of childhood injury but with no documentary evidence, we could only assume that the injury and conservative management might have resulted in the formation of synostosis while the fracture united. The distal forearm bone synostosis in children has been reported and it has been described that during childhood, simple excision without interposition graft can result in good outcome [7]. However, in adult cases, excision of synostosis has mostly been supplemented with other procedures to decrease chances of recurrence or re-ossification. A combination of therapies has thus been utilized in the treatment of radioulnar synostosis. Triple therapy in the form of pre-operative radiotherapy, heterotypic ossification excision, tissue interposition, and post-operative indomethacin has been used successfully [8]. Adipofascial radial artery perforator flap has been used in diaphyseal synostosis in one case following the concomitant head injury and surgical fixation of the fracture [9]. In a five case series, pedicled adipofascial grafts, (based on radial artery in four and posterior interosseous artery in one case) have also been used to prevent recurrence [10]. Free fat or non-vascularised fat transplant, as a readily available alternative, have also been used successfully as the interposition material following the excision of cross-union [11]. In another case, a cigar-shaped acellular dermal matrix was interposed in distal forearm synostosis and cited no donor site morbidity and more resistance to infection as advantage with its use [12]. With limited resource and financial issues, we utilized a native adjacent tendon and free fat as an inexpensive and low-morbidity option in our case, which in a longer follow-up resulted in no re-ossification. There are descriptions of low-dose radiation following the excision as other option. Limited-field, single fraction, and low dose (800 cGy) have been used previously [13]. We did not pursue this option as the solid evidence is not available. Mid-forearm synostosis, however, is reported to have good outcome [14]. We believe, our case could have been improved with supervised physiotherapy. A case of radioulnar synostosis, very similar to us, was reported following a previous ulna fracture. The excision of the synostosis and encircling of the raw surface of the ulna by silastic sheet and transplantation of free fat was done [15]. There was increase in the forearm pronation and supination movement. In place of silastic sheet, that is not available widely, we used the tendon loop over the raw surface following synostosis excision. We could not find similar reports as per the literature search done by us. This report may thus add value to the existing literature in this context.
The radioulnar synostosis is an uncommon clinical entity which is challenging to treat and more so in the light of no universal guideline or evidence-backed policy. Most of the treatment strategies are described as sporadic reports or small series and high-quality studies are not available. Most of the articles agree on the fact that the excision of the synostosis should be supplemented with interposition grafting of some material, be it biological or synthetic. Various sort of interposing substances have been described and successfully utilized. In view of universal availability of high-end materials and affordability, use of a native disposable material like like the ipsilateral PL tendon grafting in an interesting manner may be beneficial. Encircling loop of the tendon over the raw surface and secured by suturing it to itself, may prove to be a good adjunct in the management of similar cases.
In the low-resource settings, use of expandable donor tendon like the PL tendon, can be done in novel manners to cover the raw surface of the site of synostosis excision on either forearm bones during the surgical management of the diaphysial radioulnar synostosis. Encircling loop while the tendon is intact proximally, can be an inexpensive alternative to other non-biological substances or vascular grafts.
References
- 1.Osterman AL, Arief MS. Optimal management of post-traumatic radioulnar synostosis. Orthop Res Rev 2017;9:101-6. [Google Scholar]
- 2.Vince KG, Miller JE. Cross-union complicating fracture of the forearm. Part II: Adults. J Bone Joint Surg Am 1987;69:640-53. [Google Scholar]
- 3.Bauer G, Arand M, Mutschler W. Post-traumatic radioulnar synostosis after forearm fracture osteosynthesis. Arch Orthop Trauma Surg 1991;110:142-5. [Google Scholar]
- 4.Bergeron SG, Desy NM, Bernstein M, Harvey EJ. Management of posttraumatic radioulnar synostosis. J Am Acad Orthop Surg 2012;20:450-8. [Google Scholar]
- 5.Dohn P, Khiami F, Rolland E, Goubier JN. Adult post-traumatic radioulnar synostosis. Orthop Traumatol Surg Res 2012;98:709-14. [Google Scholar]
- 6.Malhotra G, Patil R, Al Yassari G, Ibrahim ES, Komma VN. Release of extensive post traumatic radio-ulnar synostosis with vascularized free flap interposition. Indian J Orthop 2021;55:493-500. [Google Scholar]
- 7.Gounot A, Simon AL, Dizin F, Chinnappa J, Mas V, Jehanno P. Pot-traumatic radioulnar synostosis in distal forearm fractures in children: A report of 2 cases. JBJS Case Connect 2022;12:e21.00590. [Google Scholar]
- 8.Abdul Azeem M, Alhojailan K, Awad M, Khaja AF. Post-traumatic radioulnar synostosis: A retrospective case series of 10 patients in Kuwait. J Shoulder Elbow Surg 2022;31:1595-602. [Google Scholar]
- 9.Samson D, Power D, Tan S. Adipofascial radial artery perforator flap interposition to treat post-traumatic radioulnar synostosis in a patient with head injury. BMJ Case Rep 2015;2015:bcr2014207659. [Google Scholar]
- 10.Sonderegger J, Gidwani S, Ross M. Preventing recurrence of radioulnar synostosis with pedicled adipofascial flaps. J Hand Surg Eur Vol 2012;37:244-50. [Google Scholar]
- 11.Yong-Hing K, Tchang SP. Traumatic radio-ulnar synostosis treated by excision and a free fat transplant. A report of two cases. J Bone Joint Surg Br 1983;65:433-5. [Google Scholar]
- 12.Gould DJ, Rahgozar P, Nagengast ES, Kulber DA. Use of acellular dermal matrix to prevent recurrence of radioulnar heterotopic ossification. Plast Reconstr Surg Glob Open 2019;7:e2257. [Google Scholar]
- 13.Cullen JP, Pellegrini VD Jr., Miller RJ, Jones JA. Treatment of traumatic radioulnar synostosis by excision and postoperative low-dose irradiation. J Hand Surg Am 1994;19:394-401. [Google Scholar]
- 14.Hanel DP, Pfaeffle HJ, Ayalla A. Management of posttraumatic metadiaphyseal radioulnar synostosis. Hand Clin 2007;23:227-34. [Google Scholar]
- 15.Miyazaki M, Haramaki N, Tabira R, Matsuyama N, Hirohashi K, Omagari K, et al. A case report of traumatic radio ulnar synostosis. Orthop Traumatol 1991;40:694-8. [Google Scholar]









