A rotating hinge TKR significantly improves function and is an effective treatment for severe OA in patients with poliomyelitis.
Dr. Vikram I Shah, Shalby Multispeciality Hospital, Sarkhej-Gandhinagar Highway, Opposite Karnavati Club, Ramdev Nagar, Ahmedabad - 380 015, Gujarat, India. E-mail: arthroplasty1@shalby.in
Introduction: The results of primary total knee replacement (TKR) using hinge implants performed in the Indian population with post-polio residual paresis (PPRP) are unknown. The purpose of this study was to report the outcome of primary rotating hinge TKR in Indian patients with PPRP at a minimum follow-up of 12 months.
Materials and Methods: We retrospectively reviewed the clinical and radiological records of six patients treated with primary rotating hinge TKR. Pre-and post-operative (at final follow-up) knee range of motion (ROM), knee sagittal deformity, knee society score (KSS), and Oxford knee score (OKS) were compared to determine improvement in function.
Results: Six rotating hinge TKRs (five female and one male patient) were analyzed for this study. At a mean follow-up of 27 ± 22 months (range, 12–71 months), the mean pre-operative KSS of 50.6 ± 2.5 significantly improved (P < 0.0001) to 72.5 ± 1.6, and the mean pre-operative OKS of 23.6 ± 1.6 significantly improved (P < 0.0001) to 35.3 ± 1.7. The mean pre-operative knee ROM of 94° ± 10° changed to 92° ± 4° (P = 0.64) and the mean pre-operative sagittal deformity of 7° ± 23.5° changed to −3° ± 2.5° (P = 0.32) at final follow-up. None of the knees had any intra- or post-operative complications or showed radiologic evidence of post-operative loosening, subsidence, or periprosthetic radiolucent lines at the final follow-up.
Conclusion: Rotating hinge TKR gave excellent clinical and radiological results at a mean follow-up of 27 months in the present study. Despite TKR being a technically challenging procedure in patients with poliomyelitis-affected limbs, a rotating hinge design, along with meticulous surgical technique, can significantly improve function in such patients.
Keywords: Poliomyelitis, total knee arthroplasty, hyperextension, rotating hinge, knee, outcome.
Poliomyelitis, a viral disease, can lead to irreversible muscle weakness and residual paralysis. Although the incidence of poliomyelitis has significantly decreased in recent years due to the widespread administration of the polio vaccine, many individuals who were affected by the disease before the routine mass immunization era continue to experience the long-term effects of the disease. Post-polio residual paresis (PPRP) of the lower limb and the resultant hypotonia, joint laxity, abnormal alignment, fixed deformities, and abnormal gait pattern predispose to early degeneration of the knee joint in these subjects [1,2]. Although primary total knee replacement (TKR) is an effective treatment option for severe tricompartmental osteoarthritis (OA), the use of traditional implant designs may not be suitable for knees with concomitant PPRP due to bone deformities, severe soft-tissue laxity, compromised quadriceps strength, and significant bone loss commonly seen in them [3,4]. This has popularized the use of rotating hinge implants for TKR in patients with PPRP to help achieve optimum stability and function and reduce the risk of implant failure. While some studies have reported favorable outcomes of hinge implants in patients with PPRP, others have raised concerns regarding higher rates of complications such as loosening, infection, and instability [4]. Despite being polio-free for several years now, India has one of the highest prevalences of post-polio sequelae worldwide [5,6]. However, the literature is lacking on primary TKR using hinge implants performed in the Indian population with PPRP. Hence, this study aimed to report the outcome of primary rotating hinge TKR in Indian patients with PPRP at a minimum follow-up of 12 months. We hypothesized that the clinical and radiological outcomes of primary rotating hinge TKR in Indian patients with PPRP would be excellent in the short term and comparable to previously published results in similar patients from other countries.
We retrospectively reviewed our institution’s registry of 19,485 primary TKR surgeries performed from January 2018 to December 2022. The inclusion criterion for this study was all patients with tricompartmental knee OA with a concomitant PPRP of the same limb who underwent primary TKR at our institution. The exclusion criteria were incomplete patient records and patients with a follow-up of <12 months. Based on the inclusion criteria, records of 7 patients (7 TKRs) with PPRP who underwent primary rotating hinge TKR were included in this study. One patient who had a follow-up duration of <12 months was excluded, and data from a total of 6 patients (6 TKRs) were analyzed for this study. This study was approved by an Institutional Ethics Committee and was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. All TKRs were performed under a tourniquet by senior surgeons at our institution, using a midline incision with a standard medial parapatellar approach to access the joint. The Zimmer NexGen® rotating hinge knee (RHK) (Zimmer Inc., Warsaw, USA) implant was used in 4 knees, and the GKS Butterfly (Permedica SPA, Merate, Italy) semi-constrained rotating hinge implant was used in 2 knees.A pre-operative computer tomographic scan was performed in all patients to determine the geometry of the proximal ½ of the tibia and distal ½ of the femur and the internal diameter of the canal. This was done to determine the feasibility of using a long stem in each case and the precautions that needed to be taken while reaming the canal during the procedure. After excision of the cruciate ligaments and menisci, coronal and sagittal imbalances were assessed in extension. Appropriate soft-tissue releases were performed, medially, laterally, and posteriorly, to address coronal and/or sagittal plane deformities and imbalances. The proximal tibial cut was performed in line with the lower tibial plateau side using a reciprocating saw and an extra-medullary referencing jig. The tibial canal was then prepared using flexible reamers to appropriate depths depending on the length of the tibial stems to be used (30 mm, 100 mm, or 155 mm for the RHK implant, and 105 mm or 160 mm for the Permedica implant). The distal femoral cut of 8–10 mm at a distal valgus angle of 5°–7° was then performed using an intramedullary guide rod and a distal cutting block. The rotation of the femoral component was set using the anteroposterior distal femur cutting block with the knee positioned at 90° flexion using the tibial cut plane, epicondylar axis, and anterior surface of the femur as anatomical references. After appropriate sizing, the anterior, posterior, and notch cuts were performed using a cutting block. The femoral canal was then prepared using sequential flexible reamers depending on the length of the femoral stems to be used and a diameter 1 mm larger, based on the length and diameter of the femoral stem to be used. None of our patients required a proximal tibial or distal femoral corrective osteotomy. Patellar resurfacing was performed on the knees due to the presence of severe patellofemoral arthritis. A trial reduction was performed using appropriately sized components to confirm adequate mediolateral and anteroposterior stability in full extension and 90° flexion, range of motion (ROM), and patellar tracking. Bone defects of ≤5 mm was filled with bone cement, and bone grafts taken from bone cuts were used in defects >5 mm, supplemented with cancellous screw fixation in large defects. The final femoral and tibial components and stems were cemented in place. The final assembly was completed once the cement was set by aligning the femoral and tibial components and inserting the hinge post and polyethylene insert in place. The tourniquet was deflated, pulse lavage given after thorough hemostasis, and the wound closed in layers under a suction drain. All patients were mobilized with full weight-bearing on the 1st post-operative day. All patients received post-operative thromboprophylaxis using oral ecosprin for 2 weeks. Apart from the perioperative antibiotic injections, patients were administered prophylactic oral antibiotics for 1 week postoperatively. All patients were reviewed clinically and radiologically at 6 weeks, 12 weeks, 6 months, and annually thereafter. Pre- and post-operative knee ROM and knee sagittal deformity (flexion and hyperextension) were measured using a digital goniometer placed on the anterior surface of the distal femur and the anterior aspect of the proximal tibia, with the knee in maximum extension and in maximum flexion. The Knee Society score (KSS) and the Oxford knee score (OKS) were used to evaluate pain and function preoperatively and at 12 weeks, 6 months, and annually thereafter. Serial anteroposterior and lateral radiographs were reviewed postoperatively, at 6 months, and on an annual basis thereafter using the Knee Society radiological score [7]. The most recent radiograph was evaluated for component and knee alignment and the presence of periprosthetic radiolucent lines. Pre- and post-operative knee ROM, knee sagittal deformity, KSS, and OKS at final follow-up were compared to determine improvement in pain and function using the t-test. P < 0.05 was considered statistically significant.
Data from six rotating hinge TKRs performed on five female and one male patient were analyzed for this study. The mean age at the time of surgery was 51 ± 12 years (range, 36–68 years) and the mean body mass index was 26.2 ± 2.6 kg/m2 (range, 23–29 kg/m2). At a mean follow-up of 27 ± 22 months (range, 12–71 months), the mean pre-operative KSS of 50.6 ± 2.5 (range, 46–53) significantly improved (P < 0.0001) to a mean post-operative KSS of 72.5 ± 1.6 (range, 70–74) (Table 1).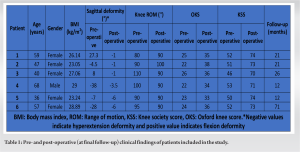 Similarly, the mean pre-operative OKS of 23.6 ± 1.6 (range, 22–26) significantly improved (P < 0.0001) to a mean post-operative OKS of 35.3 ± 1.7 (range, 33–38) at the final follow-up (Table 1). The mean pre-operative knee ROM of 94° ± 10° (range, 80°–110°) changed to a mean knee ROM of 92° ± 4° (range, 90°–100°) at final follow-up (P = 0.64) (Table 1). The mean pre-operative sagittal deformity of 7° ± 23.5° (range, 27°–38°) changed to a mean sagittal deformity of −3° ± 2.5° (range, −6°−1°) at the final follow-up (P = 0.32) (Table 1). None of the knees had any intraoperative complications such as fractures or developed post-operative complications such as deep vein thrombosis, medical complications, periprosthetic infection, knee instability, or periprosthetic fractures. None of the knees showed post-operative loosening, subsidence, or periprosthetic radiolucent lines on radiographic evaluation during follow-up (Fig. 1).
Similarly, the mean pre-operative OKS of 23.6 ± 1.6 (range, 22–26) significantly improved (P < 0.0001) to a mean post-operative OKS of 35.3 ± 1.7 (range, 33–38) at the final follow-up (Table 1). The mean pre-operative knee ROM of 94° ± 10° (range, 80°–110°) changed to a mean knee ROM of 92° ± 4° (range, 90°–100°) at final follow-up (P = 0.64) (Table 1). The mean pre-operative sagittal deformity of 7° ± 23.5° (range, 27°–38°) changed to a mean sagittal deformity of −3° ± 2.5° (range, −6°−1°) at the final follow-up (P = 0.32) (Table 1). None of the knees had any intraoperative complications such as fractures or developed post-operative complications such as deep vein thrombosis, medical complications, periprosthetic infection, knee instability, or periprosthetic fractures. None of the knees showed post-operative loosening, subsidence, or periprosthetic radiolucent lines on radiographic evaluation during follow-up (Fig. 1).
The present study showed excellent clinical and radiographic outcomes of primary rotating hinge TKR in patients with PPRP at a mean follow-up of 27 months. The short-term clinicoradiological results in our patients were similar to results previously published in the literature on primary rotating hinge TKR performed in patients with PPRP [7-9] (Table 2). 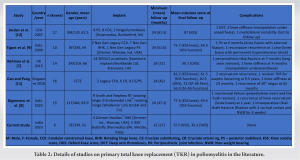 Digennaro et al. [8], in a retrospective review of 15 primary rotating hinge TKRs in polio patients, reported significant improvement in patient function using KSS at a minimum follow-up of 24 months. Similarly, Rahman et al. [7], in a retrospective review of 14 rotating hinge TKAs using the SMILES prosthesis, reported excellent clinicoradiological outcomes at a minimum follow-up of 16 months. Rotating-hinge designs provide excellent coronal and sagittal plane stability in limbs affected by poliomyelitis. This is primarily through the hinge post connecting the tibial and femoral components that resist varus-valgus and translational stresses [10]. Furthermore, rotation of the tibial bearing on the tibial platform reduces stresses at the implant-bone interface and the risk of loosening or early failure [10]. However, few studies have reported the outcomes of standard cruciate-retaining (CR), cruciate-substituting (CS), or semi-constraint implant TKR designs in poliomyelitis [9,11,12]. Jordan et al. [12] reported significant functional improvement and knee stability in 16 patients with poliomyelitis treated with TKRs using a CS, or semi-constraint design, at a mean follow-up of 41.5 months. This was similar to the retrospective study by Gan and Pang [11], where standard CR and CS TKR implants helped achieve good clinical outcomes in 14 TKRs at a mean follow-up of 42 months. Despite these encouraging results of conventional or semi-constraint TKR designs in patients with poliomyelitis [9,11,12], a systematic review by Prasad et al. [4] reported an increased risk of recurrence of hyperextension and ligamentous laxity, revision to a more constraint design, and poor long-term outcome when a conventional TKR design was used in such patients. A rotating hinge prosthesis provides intrinsic stability to the knee joint, especially in the presence of poor quadriceps muscle power, and reduces the risk of recurrence of hyperextension and instability in patients with PPRP. However, rotating hinge implants may be associated with complications such as periprosthetic fractures, post-operative knee stiffness, and recurrence of knee instability [7-9,11,12] (Table 2). In the present study, none of the knees had any intraoperative or post-operative periprosthetic fractures or post-operative knee stiffness, and none of the patients developed a post-operative recurrence of hyperextension at a minimum follow-up of 12 months. The present study, to the best of our knowledge, is the largest cohort of Indian patients with poliomyelitis treated with hinged TKR reported in the literature. However, this study has some limitations. First, this study was a case series of six patients with limited follow-up. Hence, the encouraging short-term clinicoradiographic results in the present study need confirmation with long-term follow-up in a larger cohort of patients. Second, we did not have a control group of conventional or semi-constraint implant designs to compare our results with the rotating hinge design. However, a previously published systematic review [10] confirms superior clinical performance and a lower risk of complications with the rotating hinge design, especially in the presence of quadriceps weakness.
Digennaro et al. [8], in a retrospective review of 15 primary rotating hinge TKRs in polio patients, reported significant improvement in patient function using KSS at a minimum follow-up of 24 months. Similarly, Rahman et al. [7], in a retrospective review of 14 rotating hinge TKAs using the SMILES prosthesis, reported excellent clinicoradiological outcomes at a minimum follow-up of 16 months. Rotating-hinge designs provide excellent coronal and sagittal plane stability in limbs affected by poliomyelitis. This is primarily through the hinge post connecting the tibial and femoral components that resist varus-valgus and translational stresses [10]. Furthermore, rotation of the tibial bearing on the tibial platform reduces stresses at the implant-bone interface and the risk of loosening or early failure [10]. However, few studies have reported the outcomes of standard cruciate-retaining (CR), cruciate-substituting (CS), or semi-constraint implant TKR designs in poliomyelitis [9,11,12]. Jordan et al. [12] reported significant functional improvement and knee stability in 16 patients with poliomyelitis treated with TKRs using a CS, or semi-constraint design, at a mean follow-up of 41.5 months. This was similar to the retrospective study by Gan and Pang [11], where standard CR and CS TKR implants helped achieve good clinical outcomes in 14 TKRs at a mean follow-up of 42 months. Despite these encouraging results of conventional or semi-constraint TKR designs in patients with poliomyelitis [9,11,12], a systematic review by Prasad et al. [4] reported an increased risk of recurrence of hyperextension and ligamentous laxity, revision to a more constraint design, and poor long-term outcome when a conventional TKR design was used in such patients. A rotating hinge prosthesis provides intrinsic stability to the knee joint, especially in the presence of poor quadriceps muscle power, and reduces the risk of recurrence of hyperextension and instability in patients with PPRP. However, rotating hinge implants may be associated with complications such as periprosthetic fractures, post-operative knee stiffness, and recurrence of knee instability [7-9,11,12] (Table 2). In the present study, none of the knees had any intraoperative or post-operative periprosthetic fractures or post-operative knee stiffness, and none of the patients developed a post-operative recurrence of hyperextension at a minimum follow-up of 12 months. The present study, to the best of our knowledge, is the largest cohort of Indian patients with poliomyelitis treated with hinged TKR reported in the literature. However, this study has some limitations. First, this study was a case series of six patients with limited follow-up. Hence, the encouraging short-term clinicoradiographic results in the present study need confirmation with long-term follow-up in a larger cohort of patients. Second, we did not have a control group of conventional or semi-constraint implant designs to compare our results with the rotating hinge design. However, a previously published systematic review [10] confirms superior clinical performance and a lower risk of complications with the rotating hinge design, especially in the presence of quadriceps weakness.
Rotating hinge TKR gave excellent clinical and radiological results at a mean follow-up of 27 months in the present study. Despite TKR being a technically challenging procedure in poliomyelitis-affected limbs due to the associated bony and soft-tissue abnormalities, a rotating hinge design, along with meticulous surgical technique, can significantly improve function in such patients.
A rotating hinge prosthesis provides intrinsic stability to the knee joint, significantly improves function in patients in the short term, and is an effective treatment option for severe tricompartmental OA in patients with PPRP.
References
- 1.Baliga S, Mcmillan T, Sutherland A, Sharan D. The prevalence and severity of joint problems and disability in patients with poliomyelitis in Urban India. Open Orthop J 2015;9:204-9. [Google Scholar | PubMed]
- 2.Ofran Y, Schwartz I, Shabat S, Seyres M, Karniel N, Portnoy S. Falls in post-polio patients: Prevalence and risk factors. Biology (Basel) 2021;10:1110. [Google Scholar | PubMed]
- 3.Giori NJ, Lewallen DG. Total knee arthroplasty in limbs affected by poliomyelitis. J Bone Joint Surg Am 2002;84:1157-61. [Google Scholar | PubMed]
- 4.Prasad A, Donovan R, Ramachandran M, Dawson-Bowling S, Millington S, Bhumbra R, et al. Outcome of total knee arthroplasty in patients with poliomyelitis: A systematic review. EFORT Open Rev 2018;3:358-62. [Google Scholar | PubMed]
- 5.Modlin JF, Bandyopadhyay AS, Sutter R. Immunization against poliomyelitis and the challenges to worldwide poliomyelitis eradication. J Infect Dis 2021;224 12 Suppl 2:S398-404. [Google Scholar | PubMed]
- 6.Jones KM, Balalla S, Theadom A, Jackman G, Feigin VL. A systematic review of the worldwide prevalence of survivors of poliomyelitis reported in 31 studies. BMJ Open 2017;7:e015470. [Google Scholar | PubMed]
- 7.Rahman J, Hanna SA, Kayani B, Miles J, Pollock RC, Skinner JA, et al. Custom rotating hinge total knee arthroplasty in patients with poliomyelitis affected limbs. Int Orthop 2015;39:833-8. [Google Scholar | PubMed]
- 8.Digennaro V, Manzetti M, Bogucki BD, Barile F, Panciera A, Viroli G, et al. Total knee replacements using rotating hinge implants in polio patients: Clinical and functional outcomes. Musculoskelet Surg 2022; Aug 10. doi: 10.1007/s12306-022-00755-w. Online ahead of print. [Google Scholar | PubMed | CrossRef]
- 9.Tigani D, Fosco M, Amendola L, Boriani L. Total knee arthroplasty in patients with poliomyelitis. Knee 2009;16:501-6. [Google Scholar | PubMed]
- 10.Abdulkarim A, Keane A, Hu SY, Glen L, Murphy DJ. Rotating-hinge knee prosthesis as a viable option in primary surgery: Literature review and meta-analysis. Orthop Traumatol Surg Res 2019;105:1351-9. [Google Scholar | PubMed]
- 11.Gan ZJ, Pang HN. Outcomes of total knee arthroplasty in patients with poliomyelitis. J Arthroplasty 2016;31:2508-13. [Google Scholar | PubMed]
- 12.Jordan L, Kligman M, Sculco TP. Total knee arthroplasty in patients with poliomyelitis. J Arthroplasty 2007;22:543-8. [Google Scholar | PubMed]









