Simultaneous bilateral intertrochanteric fractures are a very rare pattern of injury, but they do occur. Single-stage stabilization with proximal femoral nail is a good modality of fixing such a rare pattern of injury.
Dr. Akash Mane, Department of Orthopedics, Manipal Tata Medical College, Manipal Academy of Higher Education, Manipal - 576 104, Karnataka, India. E-mail: dr.akashmane54@gmail.com
Introduction: Unilateral intertrochanteric fractures are common injuries in elderly population. Simultaneous bilateral intertrochanteric fractures do occur but are very rare and only a few cases have been reported in the literature.
Case Report: We report two cases with different modes of injury. Both cases were fixed in a single stage by proximal femoral nailing (PFN). The first case had multiple comorbidities and after 6 weeks of follow up, she suddenly expired at home due to medical issue. The second case is the only case reported with associated bilateral superior and inferior pubic rami fracture. PFN was done in a single stage and at 1-year follow-up, the patient was having a good functional outcome.
Conclusion: Simultaneous bilateral intertrochanteric fractures are very rare injuries but these are potentially life-threatening with high morbidity. Quick assessment and early single-stage stabilization with proximal femoral nail give stable fixation and good functional outcome.
Keywords: Bilateral intertrochanteric fracture, proximal femoral nailing, pubic rami.
Unilateral intertrochanteric fractures are the most common fracture in elderly with a female-to-male ratio of 3:1. Mechanism of injury is generally high-velocity trauma in young patients and trivial trauma in elderly [1]. Bilateral fractures do occur, but most of the time the femoral neck is involved [2]. Bilateral intertrochanteric fractures are very rare. Our hospital is 100 years old and till now no case has been reported about simultaneous bilateral intertrochanteric fracture from our hospital. This shows the rarity of this pattern of injury. Cases which have been reported are either due to major trauma, epilepsy, or following primary/secondary bone diseases [3-5]. Here, we present two cases of bilateral intertrochanteric fracture which we encountered in our hospital within a span of 2 years and discuss the management of these rare types of injury.
Case 1
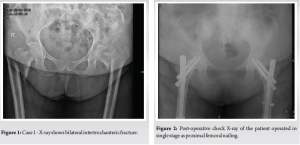
A 64-year-old female was admitted to our orthopedics ward through emergency as a case of pain, swelling and deformity of both lower limbs following injury sustained while riding as a pillion rider over scooter with both legs on same side, she fell from scooter and got injured. On examination, she was drowsy with maintained vitals and her lower limb examination showed external rotation with limitation of movement and severe pain at both hips. Her X-ray in emergency showed bilateral intertrochanteric fracture (Fig. 1).
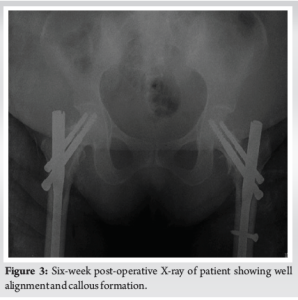
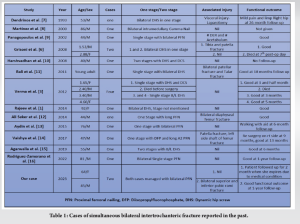
In ward, bilateral skin traction was applied. Her past medical history revealed diabetes and hypertension for which she was taking medication. Her immediate blood report showed reduced hemoglobin and very high blood sugar. Physician referral was done for control of blood sugar and pre-anesthetic checkup was advised. She also had a history of loss of consciousness for which computed tomography brain was advised, which was normal. She was put on insulin for control of blood sugar. Two units of blood were transfused to optimize her hemoglobin. It took around 1 week to make her fit for surgery. We had planned for single-stage stabilization and so the fracture was reduced on the fracture table and bilateral proximal femoral nailing (PFN) was done under general anesthesia. Post-operatively she required coronary care unit care for 3 days, after which she was transferred to ward. Her immediate post-operative X-ray was satisfactory (Fig. 2). Physiotherapy was done and the patient was discharged after stitch removal on 12th post-operative day. At 6-week follow-up check X-ray showed well-aligned fracture (Fig. 3). She suddenly expired at home at around 2-month post-operative due to a medical issue.
Case 2
A 45-year-old male was admitted through emergency as a case of pain, swelling, and deformity of the bilateral lower limb following fall of wall over the back of the patient. On examination, he was a conscious, oriented, average built person with maintained vitals and her both lower limbs examination showed external rotation posture with bilateral trochanteric tenderness and severe pain at both hips and groin. His X-ray in emergency showed bilateral intertrochanteric fracture with bilateral superior and inferior pubic rami fracture (Fig. 4).
In ward, bilateral skin traction was applied. He had no comorbidities. His blood reports were normal apart from mildly reduced hemoglobin. Patient was stabilized and pre-anesthetic checkup was advised. Once cleared for surgery, in this case, also we did single-stage stabilization by performing PFN on both sides over the traction table (Table 1).
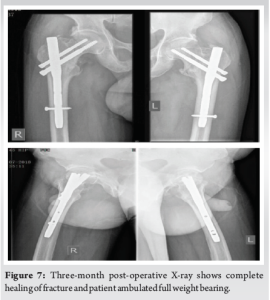
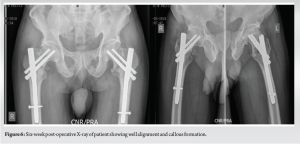
The post-operative course was uneventful. His post-operative check X-ray was satisfactory (Fig. 5). In bed, physiotherapy started from the 2nd day with leg hanging and quadriceps drill. He was discharged with advice for physiotherapy and follow-up at 6-week, 3-month, 6-month, and 1-year postoperatively. After check X-ray (Fig. 6), weight bearing with walker was allowed at 6 weeks. At 3-month follow-up, his X-ray showed a well united fracture (Fig. 7) and he could walk without support. At last, follow-up of 1 year, he had attained good functional outcome without any complication.
Simultaneous bilateral intertrochanteric fractures are very rare compared to unilateral fractures with incidence of 0.24% to 0.3% of trochanteric fractures [6]. They generally occur following road traffic accidents or high impact forces, which happened to be in our case. Cases reported in the past with either road traffic accidents or high impact forces have been summarized in Table 1. Apart from direct trauma, excessive and imbalanced contraction of muscles in the proximal part of femur does play a role in these fractures. In elderly patient’s bone loses its elastic adaptability and this leads to these types of fractures. There were a lot of challenges in managing both cases. As it was a bilateral case, when to operate, single stage or in two stage, what implant to use, which side to operate first, managing co-morbidities associated and post-operative care and rehabilitation. As both were bilateral cases, our primary aim was to stabilize the patient and make them fit for surgery. The first case, because of old age and multiple co-morbidity, took about a week to stabilize. We tried to operate as early as possible once the patient was fit for surgery. As both lower extremities were involved, we thought of using an implant which will allow early mobilization and weight bearing [2]. Various implants have been described for fixation of intertrochanteric fractures, broadly classified into extramedullary and intramedullary. As both cases had unstable fracture and we wanted them to mobilize early, we planned for single stage stabilization with intramedullary implant, and the fracture with mild displacement was fixed first. In both cases, we did stable fixation by proximal femoral nail as it is a biomechanically stronger implant, has better axial telescoping, rotational stability, and it is a load-sharing device [17]. Aggressive physiotherapy has a major role in post-operative rehabilitation and to prevent complications of chest infection and deep vein thrombosis. Both patients were mobilized in bed from the 2nd day and walking with support started at 6 weeks. Due to multiple co-morbidity, our first case suddenly expired at 2 months, but second case had good functional outcome and was doing well at 1-year follow-up.
Simultaneous bilateral intertrochanteric fractures are very rare injuries. There is a paucity of data about such injury in literature. Our second case is the only case reported with associated bilateral superior and inferior pubic rami fracture. They are potentially life-threatening with high morbidity. Treating this pattern of injury is challenging, but early single-stage stabilization with proximal femoral nail gives stable fixation and good functional outcome.
- Simultaneous intertrochanteric fractures are a very rare pattern of injury, but they do occur.
- Multidisciplinary team approach is required for managing and rehabilitating such injuries.
- Single-stage stabilization with proximal femoral nail is a good modality of fixing such a rare pattern of injury.
References
- 1.Rajeev A. Bilateral spontaneous inter-trochanteric fractures of proximal femurs. Int J Surg Case Rep 2014;5:246-8. [Google Scholar]
- 2.Sood A, Rao C, Holloway I. Bilateral femoral neck fractures in an adult male following minimal trauma after a simple mechanical fall: A case report. Cases J 2009;2:92. [Google Scholar]
- 3.Verma V, Kundu ZS, Batra A, Singh R, Sangwan SS, Gupta P. Simultaneous bilateral trochanteric fractures--a report of four cases. Chin J Traumatol 2012;15:360-3. [Google Scholar]
- 4.Copuroğlu C, Ozcan M, Dülger H, Yalniz E. Late-diagnosed bilateral intertrochanteric femur fracture during an epileptic seizure. Ulus Trauma Acil Cerrahi Derg 2012;18:92-4. [Google Scholar]
- 5.Akçali Ö, Ko C, Günal I, Alici E. Bilateral trochanteric fractures of the femur in a patient with chronic renal failure. Int Orthop 2000;24:179-80. [Google Scholar]
- 6.Grisoni N, Foulk D, Sprott D, Laughlin RT. Simultaneous bilateral hip fractures in a level I trauma center. J Trauma 2008;65:132-5. [Google Scholar]
- 7.Dendrinos G, Kousoulas D, Papagiannopoulos G. Simultaneous bilateral trochanteric and subtrochanteric fractures: Casze reports. J Trauma Acute Care Surg 1993;34:157-60. [Google Scholar]
- 8.Martínez Martín AA, Cuenca Espiérrez J, Herrera Rodríguez A, Herrero Barcos L. Fractura simultánea de ambas caderas en ancianos. MAPFRE Med 2002;13:284-6. [Google Scholar]
- 9.Panagopoulos A, Papadopoulos D, Giannikas D, Tyllianakis M. Simultaneous bilateral traumatic inter-trochanteric fractures: A case report. Acta Orthopaed Traumatol Hellenica 2002;53:284-6. [Google Scholar]
- 10.Harshvadhan J, Prabhakar MM. A case of bilateral simultaneous traumatic intertrochanteric fracture in a young patient due to dashboard injury. Internet J Orthop Surg 2008;10:3. [Google Scholar]
- 11.Bali K, Krishnan V, Sen R. Bilateral pertrochanteric fractures with bilateral patellar fractures with missed medial process fracture of talus in a young adult: A case report and review of literature. Musculoskeletal Surg 2011;95:259-63. [Google Scholar]
- 12.Seker A, Kara A, Seckin MF, Sonmez M, Erturer E, Ozturk I. Bilateral intertrochanteric and femoral diaphyseal fractures with unilateral proximal tibial fracture: A case report and review of the literature. Int J Surg Case Rep 2014;5:509-12. [Google Scholar]
- 13.Aydin E, Dülgeroğlu TC, Metineren H. Bilateral simultaneous intertrochanteric fractures of femur without major trauma. Int Med Case Rep J 2015;8:137-9. [Google Scholar]
- 14.Vaishya R, Agarwal AK, Nwagbara IC, Vijay V. Simultaneous bilateral intertrochanteric fractures of the femur: A case report and review of the literature. Cureus 2017;9:e1236. [Google Scholar]
- 15.Agarwalla A, Agarwal S, Mohindra M. Bilateral simultaneous symmetrical intertrochanteric fracture. Indian J Case Rep 2019;5:117-9. [Google Scholar]
- 16.Rodríguez-Zamorano P, Galán-Olleros M, Garcia-Coiradas J, Llanos S, Valle-Cruz JA, Marco F. Simultaneous bilateral extracapsular proximal femur fractures in the elderly. A case reports. J Surg Case Rep 2022;2022:rjac313. [Google Scholar]
- 17.Koval KJ, Zuckerman JD. Hip Fractures a Practical Guide to Management. New York: Springer-Verlag; 2000. p. 142. [Google Scholar]