Before considering revision surgery for knee stiffness post-total knee arthroplasty, assess and consider V-Y quadricepsplasty for cases with quadriceps tendon tightness.
Dr. Said Saghieh, Department of Orthopaedic Surgery, American University of Beirut Medical Center, Beirut, Lebanon. E-mail: ss15@aub.edu.lb
Introduction: Knee stiffness post-total knee arthroplasty (TKA) represents a common and challenging complication. Standard treatment protocols primarily include physical therapy, manipulation under anesthesia (MUA), fibrotic tissue release, lysis of adhesions (LOA), and in refractory cases, revision arthroplasty. However, these interventions often show minimal improvement in refractory cases. This report introduces V-Y quadricepsplasty as an innovative approach for addressing knee stiffness post-TKA, particularly in cases unresponsive to MUA and LOA, without any evidence of prosthetic component malposition or failure.
Case Report: We present a case involving a middle-aged woman experiencing persistent knee stiffness post-TKA, unresponsive to both MUA and LOA. Diagnostic evaluations confirmed no malposition or failure of the prosthetic component. The patient underwent a successful V-Y quadricepsplasty, which resulted in significant improvement in her condition.
Conclusion: This case underscores the efficacy of V-Y quadricepsplasty in managing knee stiffness post-TKA, especially in cases where traditional treatments such as MUA and LOA are ineffective and there is no evidence of prosthetic component failure or malposition. This approach potentially offers a new avenue for treatment in similar clinical scenarios.
Keywords: V-Y quadricepsplasty, total knee arthroplasty, knee, stiffness.
Total knee arthroplasty (TKA) is one of the most common major surgical procedures in the US [1]. The American Joint Replacement Registry reported in 2020, a total of 124,307 TKAs [2]. According to Kurtz et al. between the years of 2005 and 2030, the number of TKAs per year is projected to increase by 673% [3]. However, around 30% of adults with TKA are dissatisfied with their prosthesis [4]. A complication-based analysis using worldwide arthroplasty registers found the revision rate of TKA to be around 9% [5]. In a study by Pitta et al. assessing 18,065 failed total knee arthroplasties, stiffness was the 4th most common cause of TKA failures with 14.1% of all failed arthroplasty [6]. Patients presenting for revision for stiffness usually present earlier than others, with an average of 16-month post-arthroplasty [6]. When looking at early causes of implant failure, within 2 years of arthroplasty, knee stiffness was found to be second (18%) only preceded by joint loosening (26%) [7]. Flexion contracture, stiffness, and arthrofibrosis are usually used interchangeably in the literature when describing restricted knee range of motion [8]. The diagnosis of this entity is purely clinical and relies on the surgeon’s clinical judgment. Although there are no definitive consensus on the criteria for the diagnosis of post-operative treatment, usually a range of motion (ROM) <90°, or flexion contracture >5° is commonly used [8]. The three most common treatments for knee stiffness described are manipulation under anesthesia (MUA), arthroscopic/open debridement, and revision total knee arthroplasty (rTKA). The management algorithm usually starts MUA and escalated to arthroscopic/open debridement. These 2 are usually performed in the same setting. rTKA is usually reserved for refractory cases [9]. In a systematic review evaluating the treatment options for arthrofibrosis post-TKA, MUA contributed to only 20° increase in ROM post-procedure, and around 10% of patients required further treatment. Arthroscopic lysis of adhesions had an improvement of 40° in ROM on average but with a failure rate of 5.6% and 25% needed further treatment. Finally, rTKA had an average improvement of 20° of ROM but the need for further treatment post rTKA was found to be around 42.9% [10, 11]. We are reporting the case of a 47-year-old female presenting for severe knee stiffness post-bilateral total knee arthroplasties managed by release of adhesions and quadriceps tendon lengthening.
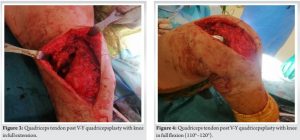
This is the case of a 47-year-old female, with a body mass index of 28, known to have bilateral knee and hip joint erosions due to severe rheumatoid arthritis (RA) status post-bilateral hip replacements and right-sided TKA in 2015. Patient’s RA is well controlled with biologic medications and was considered unrelated to the issue at hand since her inflammatory markers were well within normal range. She had a sedentary life and a desk job that required her to sit and handle papers most of the day. She presented back to clinic in 2019 for gradual decrease in ROM and pain in her right knee. She was unable to ambulate properly or use the stairs which she was able to do few months before presentation, limiting her activity to a minimum. On examination, she was found to have 30° of knee flexion and an arc of motion of 20° with no signs of knee instability. Imaging revealed adequate size and position of the components and a well-maintained joint line with no evidence of overstuffing. Accordingly, a diagnosis of arthrofibrosis was made and she was asked to follow a strict exercise regimen. The patient was lost to follow-up until April of 2022 when she presented back with the same complaint with knee flexion of 20° and tight quadriceps tendon on exam. Repeat imaging showed a stable prosthesis with no malalignments or stuffing. After careful discussion with patient regarding the available treatment options, we decided to proceed with a stepwise plan that started with MUA in the operating room followed by open release of adhesions and V-Y quadricepsplasty if the results were deemed unsatisfactory. The patient was informed of the risks/benefits and consented to all the proposed procedures. The patient was taken to the operating room where she underwent combined spinal and epidural anesthesia in the supine position to allow for full relaxation. MUA was attempted first and around 60° of knee flexion was achieved (Fig. 1). This was not enough given the expectations and functionality of the patient. We decided to proceed with the second stage of the surgery. Through the previous midline incision, a medial parapatellar approach was utilized and the patella was dislocated laterally. The supra and infra-patellar adhesions were removed including adhesions formed between the quadriceps tendon and femur. Subperiosteal release was done medially and laterally. Scar tissues were removed from the medial and lateral gutters as well. The knee flexion improved to around 90°. Extensor mechanism tightness was found to be significant and prevented further improvement in knee flexion. The patellar component was found to be overstuffed and revision was decided. A downgrade from 42 mm to 38 mm patella cemented peg was done while removing around 8 mm of the patella. The knee components were otherwise found stable. We then opted to proceed with VY-quadricepsplasty, in line with the extensor mechanism. It was performed along the tendon of the quadriceps. Knee flexion reached 110°–120° (Fig. 2).
The quadricepsplasty was reinforced using Vicryl sutures (Fig. 3 and 4).
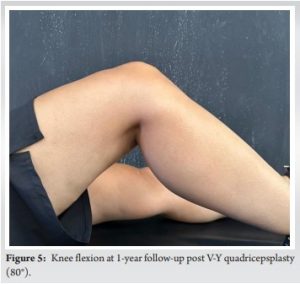
The patella tracking was found to be optimal throughout the knee ROM. The wound was closed over a Hemovac drain. Postoperatively, the patient was started on continuous passive motion (CPM) machine 0°–110°. She was discharged home 2 days after surgery with CPM machine and aggressive physical therapy. On 2-week post-operative follow-up, the patient was able to ambulate with assistance and sit comfortably with minimal pain. Wounds were healing well, and she was able to achieve active flexion of 90° on examination. She was instructed to continue with aggressive physical therapy. At 6-month follow-up, knee ROM was stable at 90°, and she was able to ambulate without assistance and climb stairs. The last follow-up was at the 1-year benchmark where the patient was able to achieve 80° of knee flexion (Fig. 5). The patient did not have any complaints concerning her knee and was satisfied by the amount of flexion she was able to achieve at this point.
Knee stiffness and arthrofibrosis are one of the most common early complications post-TKA. Three possible treatments options are described for people presenting with arthrofibrosis following TKA. MUA is by far the least invasive and most efficient in the early post-operative period. In case of failure MUA to yield acceptable ROM, surgical treatment is then indicated. The surgical options include either arthroscopic or open release of fibrotic tissue. rTKA is reserved for refractory cases or cases with malpositioned components and poor soft tissue balance. The literature provides limited intel on how to proceed once release of adhesions fails to provide functional ROM. rTKA is known to yield unsatisfactory results in terms of ROM even in the presence of a correctable defect in implant position [12]. In a recent review by Haffar et al., rTKA for stiffness and arthrofibrosis leads to inferior clinical outcomes and final ROM as compared to MUA [10]. Furthermore, they found that as many as 43% of patients undergoing rTKA for arthrofibrosis treatment required further care, compared to 17% of MUA patients. A systematic review by van Rensch et al., looking at long-term outcome post-rTKA, found that patients revising for stiffness had by far worse outcome in terms of pain, quality of life post-operative, and functionality compared to other etiologies requiring revisions [13]. Furthermore, these patients deteriorated slightly at longer follow-up compared to initial presentation. To our knowledge, this is the first case in the literature describing quadricepsplasty as a treatment option for patients with arthrofibrosis following total knee replacement. A V-Y quadricepsplasty was first described by Curtis and Fisher where the central portion of the quadriceps tendon incised in a V-Y fashion to allow advancement through a long anterolateral incision [14]. The iliotibial band is released, and the anterior capsule of the knee is divided transversely as far as the collateral ligament. The quadriceps muscle is mobilized. The knee ROM is then assessed, and the desired degrees are tested. The lengthened quadriceps is re-sutured with the knee held at 30°. Although not previously described for knee flexion contracture post-TKA treatment, V-Y quadricepsplasty is a widely used procedure for tendon lengthening in patients presenting with extensor element contracture and limited flexion. Myelomeningocele [15, 16], congenital short femur [17], patellar [18], and Achilles chronic tendon ruptures [19, 20] are all examples where V-Y plasties are widely used. In addition, V-Y quadricepsplasty has been widely used in severe extensor mechanism contracture during TKA. If done properly, without insulting the biomechanics of the patella and extensor mechanism, V-Y quadricepsplasty proved to be a safe and efficient procedure for tendon lengthening [21-23]. Knee mobility is required for daily living and functionality. Different degrees are required to carry out the different tasks of daily life. For example, post-knee arthroplasty, climbing stairs requires 66° of knee flexion whereas sitting on a chair requires 77° of knee flexion [24]. With no clear benchmark identified for satisfactory minimal knee flexion ROM, careful case specific consideration needs to be taken factoring in patient’s day-to-day requirements and expectations. Furthermore, the risks versus benefits of aiming for a drastic improvement in knee flexion capacity need to be carefully assessed, considering potential complications, such as supracondylar fractures and patellar tendon ruptures [25]. Our patient’s ROM allowed her to do all her activities of daily living, such as walking, climbing stairs, and sitting on a chair. We were able to achieve 60° of flexion post-MUA and 90° of flexion after open release of adhesions. The degree of MUA applied was deemed enough to not increase the risk of intraoperative fracture given patient’s history of RA [25, 26]. Intraoperative MUA and open release of adhesions did not yield satisfactory results knowing that whatever degree of flexion achieved under anesthesia while the patient is fully relaxed will most probably decrease once the patient is awake. The decision to proceed with quadricepsplasty was taken. V-Y quadricepsplasty is a known procedure that is widely used and that our performing team is familiar with, our team’s extensive experience and previous reports in the literature state that if done properly, no clinically significant extension lag or patellar blood supply compromise would be a risk [21-23]. The patient reported satisfactory results following her final follow-up allowing her to proceed with most of her daily tasks such as walking, climbing up and down the stairs, and sitting comfortably. Furthermore, quadriceps tendon contraction is a known and well-described complication of long-term disuse, especially in patients with known inflammatory conditions [27]. We hypothesize that our patient’s limited knee flexion is due to contraction of the quadriceps muscle, especially that she did not have any clinical or radiographic signs of prosthetic malfunction, other than a flexion extension gap and a tight quadriceps tendon on physical examination. Similar to our patient, a case series found that tethering adhesions of the quadriceps muscle are the major pathological structures responsible for a limited ROM in the stiff arthritic knee [28].
In patients with severe arthrofibrosis, quadriceps tightening, and limited ROM following TKA, a combination of quadricepsplasty and open release of fibrotic tissue may prove beneficial. Particularly in cases where extensor mechanism tightness is evident upon physical examination, and where results from exercise therapy, MUA, and release of adhesions have been unsatisfactory, tendon lengthening could be advantageous. Quadricepsplasty presents as a safe and cost-effective alternative to rTKA for patients with refractory arthrofibrosis. However, its application should be confined to those patients where tight quadriceps are confirmed intraoperatively under complete relaxation. There is a need for further research to thoroughly assess the long-term risks and benefits of quadricepsplasty in this specific patient group. This case report details the experience with a single patient; a larger case series is required to establish the efficacy of this procedure in similar clinical scenarios.
For patients with severe arthrofibrosis, quadriceps tightening, and limited ROM post-TKA, combining V-Y quadricepsplasty with open release of fibrotic tissue offers a promising, cost-effective alternative to revision surgeries. However, careful patient selection, confirmed by intraoperative assessment of quadriceps tightness, is crucial, underscoring the need for further research to validate long-term outcomes of this approach.
References
- 1.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among medicare beneficiaries, 1991-2010. JAMA 2012;308:1227-36. [Google Scholar]
- 2.Springer BD, Levine BR, Golladay GJ. Highlights of the 2020 American joint replacement registry annual report. Arthroplast Today 2021;9:141-2. [Google Scholar]
- 3.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [Google Scholar]
- 4.Abdel MP, Ledford CK, Kobic A, Taunton MJ, Hanssen AD. Contemporary failure aetiologies of the primary, posterior-stabilised total knee arthroplasty. Bone Joint J 2017;99:647-52. [Google Scholar]
- 5.Sadoghi P, Liebensteiner M, Agreiter M, Leithner A, Böhler N, Labek G, et al. Revision surgery after total joint arthroplasty: A complication-based analysis using worldwide arthroplasty registers. J Arthroplasty 2013;28:1329-32. [Google Scholar]
- 6.Pitta M, Esposito CI, Li Z, Lee YY, Wright TM, Padgett DE. Failure after modern total knee arthroplasty: A prospective study of 18,065 Knees. J Arthroplasty 2018;33:407-14. [Google Scholar]
- 7.Le DH, Goodman SB, Maloney WJ, Huddleston JI. Current modes of failure in TKA: Infection, instability, and stiffness predominate. Clin Orthop Relat Res 2014;472:2197-200. [Google Scholar]
- 8.Tibbo ME, Limberg AK, Salib CG, Ahmed AT, Van Wijnen AJ, Berry DJ, et al. Acquired idiopathic stiffness after total knee arthroplasty: A systematic review and meta-analysis. J Bone Joint Surg Am 2019;101:1320-30. [Google Scholar]
- 9.Cheuy VA, Foran JR, Paxton RJ, Bade MJ, Zeni JA, Stevens-Lapsley JE. Arthrofibrosis associated with total knee arthroplasty. J Arthroplasty 2017;32:2604-11. [Google Scholar]
- 10.Haffar A, Goh GS, Fillingham YA, Torchia MT, Lonner JH. Treatment of arthrofibrosis and stiffness after total knee arthroplasty: An updated review of the literature. Int Orthop 2022;46:1253-79. [Google Scholar]
- 11.Hegazy AM, Elsoufy MA. Arthroscopic arthrolysis for arthrofibrosis of the knee after total knee replacement. HSS J 2011;7:130-3. [Google Scholar]
- 12.Ghani H, Maffulli N, Khanduja V. Management of stiffness following total knee arthroplasty: A systematic review. Knee 2012;19:751-9. [Google Scholar]
- 13.Van Rensch PJ, Hannink G, Heesterbeek PJ, Wymenga AB, Van Hellemondt GG. Long-term outcome following revision total knee arthroplasty is associated with indication for revision. J Arthroplasty 2020;35:1671-7. [Google Scholar]
- 14.Curtis BH, Fisher RL. Congenital hyperextension with anterior subluxation of the knee. Surgical treatment and long-term observations. J Bone Joint Surg Am 1969;51:255-69. [Google Scholar]
- 15.Dias LS. Surgical management of knee contractures in myelomeningocele. J Pediatr Orthop 1982;2:127-31. [Google Scholar]
- 16.Abdelaziz TH, Samir S. Congenital dislocation of the knee: A protocol for management based on degree of knee flexion. J Child Orthop 2011;5:143-9. [Google Scholar]
- 17.Hosalkar HS, Jones S, Chowdhury M, Hartley J, Hill RA. Quadricepsplasty for knee stiffness after femoral lengthening in congenital short femur. J Bone Joint Surg Br 2003;85:261-4. [Google Scholar]
- 18.Zhang X, Li Y, Chen J, Yan C, Tan X, Liu H. Over 20 years of chronic patellar ligament rupture with severe knee osteoarthritis for total knee arthroplasty: A case report. BMC Musculoskelet Disord 2020;21:342. [Google Scholar]
- 19.Guclu B, Basat HC, Yildirim T, Bozduman O, Us AK. Long-term results of chronic achilles tendon ruptures repaired with v-y tendon plasty and fascia turndown. Foot Ankle Int 2016;37:737-42. [Google Scholar]
- 20.Lin YJ, Duan XJ, Yang L. V-Y Tendon plasty for reconstruction of chronic achilles tendon rupture: A medium-term and long-term follow-up. Orthop Surg 2019;11:109-16. [Google Scholar]
- 21.Trousdale RT, Hanssen AD, Rand JA, Cahalan TD. V-Y quadricepsplasty in total knee arthroplasty. Clin Orthop Relat Res 1993;286:48-55. [Google Scholar]
- 22.Tsukamoto N, Miura H, Matsuda S, Mawatari T, Kato H, Iwamoto Y. Functional evaluation of four patients treated with V-Y quadricepsplasty in total knee arthroplasty. J Orthop Sci 2006;11:394-400. [Google Scholar]
- 23.Aglietti P, Buzzi R, D’Andria S, Scrobe F. Quadricepsplasty with the V-Y incision in total knee arthroplasty. Ital J Orthop Traumatol 1991;17:23-9. [Google Scholar]
- 24.Myles CM, Rowe PJ, Walker CR, Nutton RW. Knee joint functional range of movement prior to and following total knee arthroplasty measured using flexible electrogoniometry. Gait Posture 2002;16:46-54. [Google Scholar]
- 25.Thompson R, Novikov D, Cizmic Z, Feng JE, Fideler K, Sayeed Z, et al. Arthrofibrosis after total knee arthroplasty: Pathophysiology, diagnosis, and management. Orthop Clin North Am 2019;50:269-79. [Google Scholar]
- 26.Purudappa PP, Ramanan SP, Tripathy SK, Varatharaj S, Mounasamy V, Sambandam SN. Intra-operative fractures in primary total knee arthroplasty-a systematic review. Knee Surg Relat Res 2020;32:40. [Google Scholar]
- 27.Bennet GE. Lengthening of the quadriceps tendon. JBJS 1922;4:279-316. [Google Scholar]
- 28.Tarabichi S, Tarabichi Y. Can an anterior quadriceps release improve range of motion in the stiff arthritic knee? J Arthroplasty 2010;25:571-5. [Google Scholar]