Osteoarthritis patients commonly exhibit Vitamin D insufficiency, elevated parathyroid hormone levels, and lipid dysregulation, suggesting a complex metabolic interplay that underscores the importance of assessing and potentially correcting these parameters to improve disease management and patient outcomes.
Dr. KS Karthik, Department of Orthopaedics, Faculty of Medicine – Sri Lalithambigai Medical College and Hospital, Dr MGR Educational and Research Institute, Chennai, Tamil Nadu, India. E-mail: drks2050@gmail.com
Introduction: Osteoarthritis (OA) is a degenerative joint disease characterized by cartilage degradation, bone remodeling, and pain. Recent evidence suggests that Vitamin D insufficiency, alterations in parathyroid hormone (PTH) levels, and dyslipidemia may play roles in the pathophysiology of OA, affecting calcium homeostasis and bone health. We investigated the association between Vitamin D, PTH levels, lipid profile, and calcium homeostasis in OA patients.
Materials and Methods: This case–control study involved 200 participants, divided into OA and control groups, at a tertiary care center from April to May 2023. Serum levels of 25-hydroxyvitamin D, PTH, total cholesterol, HDL, LDL, triglycerides, and calcium were measured. Statistical analysis was conducted to assess correlations between these biomarkers and OA status.
Results: OA patients demonstrated significantly lower Vitamin D levels and higher PTH and total cholesterol levels compared to controls. Vitamin D insufficiency was prevalent, with a notable correlation between decreased Vitamin D levels, elevated PTH, and dyslipidemia. These findings suggest a potential metabolic interplay affecting OA progression and symptomatology.
Conclusion: The study highlights a significant association between Vitamin D insufficiency, altered PTH levels, and lipid dysregulation in OA patients, underscoring the importance of assessing these parameters in the clinical management of OA. Further research is needed to explore the therapeutic implications of correcting Vitamin D insufficiency and lipid abnormalities in OA.
Keywords: Osteoarthritis, Vitamin D, parathyroid hormone, lipid profile, calcium homeostasis, dyslipidemia.
The intricate relationship between Vitamin D, parathyroid hormone (PTH), lipid profile, and calcium homeostasis in osteoarthritis (OA) patients presents a compelling field of study. Vitamin D, essential for calcium regulation and bone health, has been linked to lipid profiles, important predictors of cardiovascular diseases. Notably, Vitamin D levels inversely correlate with cardiovascular risk biomarkers, including atherogenic lipid profiles. However, the implications of Vitamin D supplementation in modifying cardiovascular risks are not well established [1]. PTH, working synergistically with Vitamin D, is pivotal in mineral metabolism, essential for maintaining calcium and phosphate homeostasis and overall bone health. This balance is crucial, especially in conditions like osteoarthritis, where bone and joint integrity are compromised [2]. The regulation of phosphate-calcium balance, influenced by Vitamin D and PTH, is significant in bone health, as evidenced in conditions such as adolescent idiopathic scoliosis, where abnormalities in these levels were observed, despite normal phosphate-calcium balance and PTH levels [3]. Moreover, Vitamin D and PTH levels are crucial for bone mineral density and turnover, especially in osteoporosis, a condition that shares several pathophysiological pathways with osteoarthritis [4]. The association of these factors with bone microarchitecture in the aging population further underlines their importance in conditions like osteoarthritis [5]. The aim of this observational study was to explore the association between Vitamin D, PTH, and lipid profile in osteoarthritis patients, focusing on their impact on calcium homeostasis. The objectives are, to analyze the serum levels of Vitamin D in OA patients; to assess PTH levels responsible for calcium homeostasis; and to evaluate the extent of dyslipidemia in these patients. This study investigates the complex interplay between these factors in OA, potentially informing better clinical management and treatment strategies for this condition.
Study design and setting
This study was designed as an observational and cross-sectional investigation involving a total of 200 participants. The study was conducted after obtaining ethics approval from the Faculty of Medicine – Sri Lalithambigai Medical College and Hospital, Chennai – Dr MGR-ERI/SLMCH/2023/004 dated February 08, 2023
Sample size
In accordance with the findings by Yarparvar et al., [6] to achieve a power of 80% (0.84) and maintain a significance level of 5% (1.96), each group necessitates a sample size of 95. Factoring in a non-response rate of 5%, the requisite sample size per group is adjusted to 100. Therefore, the cumulative sample size required for both groups amounts to 200.
Participants
Inclusion criteria for participation in the study encompassed adults 39–70 years of age who had received a diagnosis of of all stages. In addition, participants were required to express their willingness to participate and provide informed consent.
Exclusion criteria involved individuals with a history of other metabolic bone diseases, such as osteoporosis or Paget’s disease. Those who had used medications affecting bone metabolism (e.g., bisphosphonates and corticosteroids) within the past 3 months were excluded from the study. Participants with severe comorbid conditions (e.g., end-stage renal disease and uncontrolled diabetes), as well as pregnant or lactating individuals, were also not included in the study.
Sample collection and processing
Blood samples were collected in the morning following an overnight fast lasting a minimum of 10 h. These samples were collected using serum-separating tubes and subsequently centrifuged at 3000 rpm for duration of 10 min. The resulting serum was then aliquoted and stored at −80°C until the time of analysis.
Laboratory analysis
Vitamin D measurement
Serum 25-hydroxyvitamin D levels were quantified utilizing a high-performance liquid chromatography-tandem mass spectrometry (HPLC-MS/MS) system, known for its high specificity and sensitivity. Calibration and quality control procedures were implemented, involving the use of standard Vitamin D controls.
PTH measurement
Intact parathyroid hormone (PTH) levels were assessed through a chemiluminescent immunoassay, ensuring both high accuracy and low cross-reactivity.
Lipid profile assessment
The lipid profile, including parameters such as total cholesterol, HDL, LDL, and triglycerides, was enzymatically measured using an automated clinical chemistry analyzer. Quality control for lipid profile assessment was upheld through the deployment of lipid calibrators and control sera.
Calcium measurement
Serum calcium levels were determined using the colorimetric method with an automated analyzer. The process involved the use of standard calibrators for assay calibration and control sera to ensure quality assurance.
Statistical analysis
In the data analysis phase, descriptive statistics were employed to summarize participant characteristics and laboratory results. This included the calculation of means with standard deviations and medians with interquartile ranges. Correlation analyses and subgroup analyses, considering factors such as gender and age, were conducted using statistical tests such as Pearson’s or Spearman’s correlation, t-tests, or ANOVA, as deemed appropriate. The odds ratio was calculated as well. Statistical significance was defined at a threshold of P < 0.05, and software Python 3.10 utilized for data.
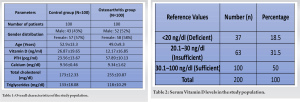
Study population characteristics
The study consisted of two groups, with 100 participants each: A control group and an osteoarthritis group. The gender distribution across groups showed a slightly higher proportion of females than males, with the control group comprising 43% males and 57% females, whereas the osteoarthritis group consisted of 52% males and 58% females. Age analysis revealed an average age of 52.9 ± 13.3 years in the control group and 49.0 ± 9.3 years in the osteoarthritis group, indicating a younger demographic in the latter. Notably, Vitamin D levels were significantly lower in the osteoarthritis group (12.17 ± 16.85 ng/ml) compared to the control group (26.87 ± 19.65 ng/ml). Parathyroid hormone (PTH) levels and total cholesterol were markedly elevated in the osteoarthritis group, with values of 57.89 ± 10.13 pcg/ml and 255 ± 20.87 mg/dl, respectively, compared to the control group (23.56 ± 13.67 pcg/ml and 173 ± 12.33 mg/dl, respectively). Conversely, triglyceride levels were higher in the control group (133 ± 18.08 mg/dl) compared to the osteoarthritis group (118 ± 10.29 mg/dl) (Table 1).
Serum Vitamin D levels
The distribution of Vitamin D levels across the entire study population showed that 18.5% were deficient (<20 ng/dl), 31.5% were insufficient (20.1–30 ng/dl), and 50% were sufficient (30.1–100 ng/dl), encompassing both control and osteoarthritis group (Table 2).
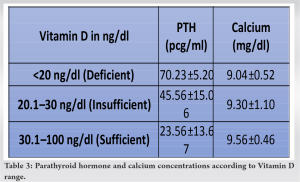
Parathyroid hormone and calcium concentrations
Vitamin D deficiency correlated with elevated PTH levels (70.23 ± 5.20 pcg/ml) and lower calcium levels (9.04 ± 0.52 mg/dl). Participants with insufficient Vitamin D levels exhibited intermediate PTH levels (45.56 ± 15.06 pcg/ml) and calcium levels (9.30 ± 1.10 mg/dl). Those with sufficient Vitamin D levels showed the lowest PTH levels (23.56 ± 13.67 pcg/ml) and the highest calcium levels (9.56 ± 0.46 mg/dl), indicating a possible inverse relationship between Vitamin D levels and PTH, and a direct relationship with calcium level (Table 3).
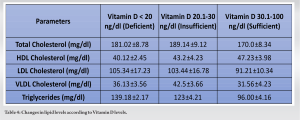
Lipid levels and Vitamin D
Analysis of lipid levels in relation to Vitamin D status showed that participants with Vitamin D deficiency had higher total cholesterol (181.02 ± 8.78 mg/dl) and VLDL cholesterol (36.13 ± 3.56 mg/dl), but lower HDL cholesterol (40.12 ± 2.45 mg/dl) compared to those with sufficient Vitamin D levels, who exhibited lower total cholesterol (170.0 ± 8.34 mg/dl), VLDL cholesterol (31.56 ± 4.23 mg/dl), and higher HDL cholesterol (47.23 ± 3.98 mg/dl). LDL cholesterol levels were also lower in the sufficient Vitamin D group (91.21 ± 10.34 mg/dl) compared to the deficient group (105.34 ± 17.23 mg/dl) (Table 4).
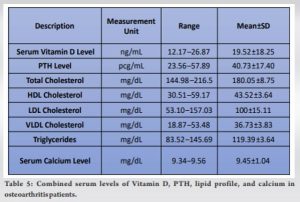
Combined serum levels in osteoarthritis patients
In osteoarthritis patients, the mean serum Vitamin D level was found to be 19.52 ± 18.25 ng/mL, indicating a general trend toward Vitamin D insufficiency. PTH levels ranged broadly from 23.56 to 57.89 pcg/mL, with a mean of 40.73 ± 17.40 pcg/mL. The lipid profile was characterized by a total cholesterol mean of 180.05 ± 8.75 mg/dL, HDL cholesterol at 43.52 ± 3.64 mg/dL, LDL cholesterol at 100 ± 15.11 mg/dL, and VLDL cholesterol at 36.73 ± 3.83 mg/dL. Triglyceride levels were moderately elevated, with a mean of 119.39 ± 3.64 mg/dL. Calcium levels were relatively stable, ranging from 9.34 to 9.56 mg/dL, with a mean of 9.45 ± 1.04 mg/dL (Table 5).
The observed data suggest that osteoarthritis patients exhibit distinct biochemical profiles, characterized by lower Vitamin D levels, higher PTH, and altered lipid profiles, including total cholesterol and triglyceride levels, compared to controls. These findings underscore the potential interplay between Vitamin D status, parathyroid hormone levels, and lipid metabolism in the context of osteoarthritis.
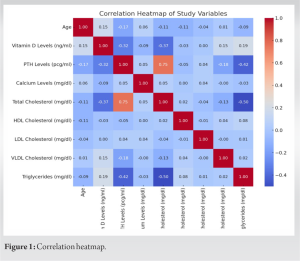
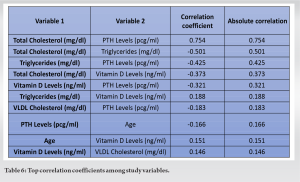
Correlation analysis
Correlation analyses revealed significant relationships between Vitamin D levels and PTH levels (r = −0.321), indicating an inverse relationship. A significant negative correlation was also observed between Vitamin D levels and total cholesterol (r = −0.372). PTH levels showed a strong positive correlation with total cholesterol (r = 0.754). These findings suggest interplay between Vitamin D status, parathyroid hormone levels, and lipid metabolism (Table 6, Fig. 1).
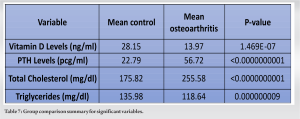
Group comparisons
Group comparison analyses using t-tests and Mann–Whitney U-tests revealed significant differences between the control and osteoarthritis groups in PTH levels, total cholesterol, triglycerides, and Vitamin D levels. The osteoarthritis group exhibited higher PTH and cholesterol levels but lower Vitamin D levels compared to the control group (Table 7).
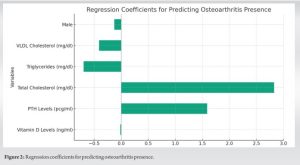
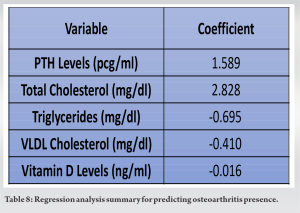
Regression analysis
Logistic regression identified PTH levels and total cholesterol as strong predictors of osteoarthritis presence, with coefficients of 1.589 and 2.827, respectively. Triglycerides and VLDL cholesterol were negatively associated with osteoarthritis presence, suggesting complex metabolic interactions (Fig. 2, Table 8).
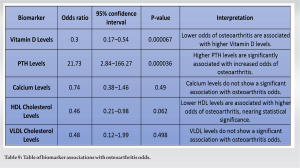
Odds ratio
Vitamin D levels were inversely associated with the odds of developing osteoarthritis, with an odds ratio (OR) of 0.30 (95% CI: 0.17–0.54, P = 0.000067). This finding suggests that higher levels of Vitamin D may confer a protective effect against the development of osteoarthritis. Conversely, parathyroid hormone (PTH) levels showed a significant positive association with osteoarthritis odds, with an OR of 21.73 (95% CI: 2.84–166.27, P = 0.000036). This substantial increase in odds indicates a potential detrimental role of elevated PTH levels in osteoarthritis pathogenesis. Calcium levels did not exhibit a significant association with osteoarthritis odds (OR: 0.74, 95% CI: 0.38–1.46, P = 0.49), suggesting that within the range of values observed in this cohort, calcium levels alone do not significantly influence the risk of osteoarthritis. HDL Cholesterol levels were found to be inversely associated with osteoarthritis odds, with an OR of 0.46 (95% CI: 0.21–0.98, P = 0.062). This association is on the border of statistical significance, suggesting that lower HDL levels may be associated with an increased risk of osteoarthritis, warranting further investigation. VLDL cholesterol levels showed no significant association with osteoarthritis odds (OR: 0.48, 95% CI: 0.12–1.99, P = 0.498), indicating that VLDL cholesterol levels, within the observed range, do not significantly affect osteoarthritis risk. The odds ratio is shown in Table 9.
The intricate relationship between Vitamin D, PTH, lipid profiles, and calcium homeostasis holds significant implications for patients with OA, offering insights into the metabolic interplays affecting disease progression and management strategies. Research has demonstrated an inverse relationship between serum PTH levels and the risk of OA, particularly emphasizing knee OA. A Mendelian randomization study highlighted this inverse association, suggesting a protective role of PTH against OA development. However, this study also noted the absence of a causal effect of serum 25-hydroxyvitamin D [25(OH)D] levels on OA, indicating the complexity of these relationships and the need for further exploration into how PTH may influence OA [7]. Vitamin D deficiency has been directly associated with the progression of knee OA. Studies suggest that individuals deficient in Vitamin D are at an increased risk of knee OA progression, underscoring the importance of maintaining adequate Vitamin D levels for joint health and potentially slowing OA progression [8]. This is further supported by longitudinal data from the Osteoarthritis Initiative (OAI), which indicated that low Vitamin D levels significantly increased the risk of knee OA worsening over a period of 4 years, with those having both low Vitamin D and high PTH concentrations facing a threefold risk increase [9]. A cross-sectional study investigating early OA (EOA) revealed that patients with EOA exhibited significantly lower levels of serum 25(OH)D compared to matched controls. Importantly, lower Vitamin D levels were associated with higher levels of pain intensity, disability, and anxiety, as well as diminished physical performance measures such as sit-to-stand and walking speed, highlighting the broader implications of Vitamin D not just in physiological aspects of OA but also in affecting the quality of life and mental health of patients [10]. The significance of Vitamin D and PTH extends beyond calcium homeostasis to encompass lipid metabolism and cardiovascular health. An inverse correlation between LDL cholesterol levels and Vitamin D suggests a potential protective effect of Vitamin D against atherogenic lipid profiles, though the impact of Vitamin D supplementation on blood lipids and cardiovascular risk factors remains an area of active research [1]. The role of Vitamin D and PTH in metabolic syndrome components and their potential influence on metabolic risk factors further emphasizes their broader metabolic roles [11]. Patients with OA, particularly postmenopausal women and those with established osteoporosis, have shown that hypovitaminosis D and altered PTH response can affect bone turnover and mortality, stressing the need for adequate Vitamin D levels for bone health and overall mortality risk management [4]. The mutual relationship between the Vitamin D-PTH axis and lipid and glucose metabolism highlights a significant, synergistic role in influencing not only bone metabolism but also plasma glucose and serum lipid levels [12]. Our study’s findings on the association between Vitamin D levels, parathyroid hormone (PTH) levels, lipid profiles, and osteoarthritis are corroborated by a wide array of global research, offering a comprehensive view of the role of Vitamin D in osteoarthritis progression. We discovered significantly lower Vitamin D levels in the osteoarthritis group (12.17 ± 16.85 ng/ml) compared to the control group (26.87 ± 19.65 ng/ml). This observation aligns with global trends, such as those reported in a systematic review and meta-analysis focusing on the Indian population, which found a significant reduction in Vitamin D levels among knee osteoarthritis patients, indicating a widespread issue of Vitamin D insufficiency in osteoarthritis across different demographics [13]. The elevated PTH levels in our osteoarthritis patients, compared to controls, underscore the inverse relationship between Vitamin D and PTH, highlighting how Vitamin D deficiency may contribute to osteoarthritis progression through its effects on bone and mineral metabolism. This finding dovetails with broader research, suggesting that Vitamin D insufficiency can exacerbate osteoarthritis symptoms and progression, emphasizing the importance of maintaining sufficient Vitamin D levels for bone health and potentially mitigating osteoarthritis-related outcomes [9]. Lipid profile alterations, observed in our study, with significant differences in total cholesterol and triglyceride levels between osteoarthritis patients and controls, suggest a complex interplay between lipid metabolism and Vitamin D status. This aspect, though less frequently explored, echoes the need for further investigation as indicated by our findings and the broader implications for osteoarthritis management [14, 15]. Moreover, the NHANES analysis and a study published in Arthritis Research and Therapy complement our findings by highlighting the beneficial effects of maintaining sufficient serum Vitamin D levels on knee symptoms, psychological health, and inflammatory markers over time. These studies provide a broad epidemiological and clinical trial perspective, contrasting with our focused examination but collectively affirming the critical role of Vitamin D in osteoarthritis pathology [14, 15]. Our findings also highlight the prevalence of Vitamin D deficiency and insufficiency in osteoarthritis patients, aligning with the NHANES study’s documentation of a nuanced relationship between serum 25(OH)D concentrations and osteoarthritis prevalence. This parallel reinforces the notion that Vitamin D status significantly influences osteoarthritis management and highlights the potential benefits of early diagnosis and treatment of Vitamin D deficiency to delay osteoarthritis progression [15]. This study, while providing valuable insights into the relationship between Vitamin D, PTH, lipid profiles, and osteoarthritis, carries certain limitations that must be acknowledged. One primary constraint is its cross-sectional design, which restricts the ability to infer causality between the observed variables. The study’s findings reflect associations at a single point in time, making it challenging to determine the directionality of the relationships observed. In addition, the sample size, although adequate for preliminary observations, may limit the generalizability of the findings to broader populations. The study population, drawn from a specific geographic location and demographic, may not fully represent the diverse manifestations of osteoarthritis across different ethnicities and regions. Moreover, the reliance on serum markers as proxies for Vitamin D status, bone health, and lipid profiles does not account for individual variations in metabolism, dietary intake, and lifestyle factors that could influence these measurements. The study did not control for all potential confounding variables, such as physical activity levels, sun exposure, dietary habits, and use of Vitamin D supplements, which could affect Vitamin D levels and lipid profiles independently of osteoarthritis status. Future research should aim to address these limitations through longitudinal study designs that can better establish causality and explore the temporal dynamics of Vitamin D, PTH, and lipid profiles in osteoarthritis progression. Larger, multicentric studies involving diverse populations would enhance the external validity of the findings, providing a more comprehensive understanding of these associations globally. Interventional studies investigating the effects of Vitamin D supplementation on osteoarthritis outcomes, including pain management, disease progression, and quality of life, are needed to elucidate potential therapeutic benefits. Moreover, exploring the molecular mechanisms underlying the observed associations could provide deeper insights into the pathophysiology of osteoarthritis and identify novel targets for intervention. Our study aligns with global research, emphasizing the critical role of Vitamin D in osteoarthritis. It highlights a consistent trend of Vitamin D insufficiency in osteoarthritis patients, underlining its importance in disease progression and associated symptoms. Standardized research approaches are needed to deepen our understanding of osteoarthritis’s metabolic basis and the therapeutic potential of Vitamin D. These findings underscore the significance of Vitamin D and parathyroid hormone in osteoarthritis, suggesting their adequate maintenance may protect against disease progression. Vitamin D and PTH influence not only calcium homeostasis but also broader metabolic pathways relevant to osteoarthritis. Further, clinical exploration of Vitamin D supplementation is warranted for potential benefits in slowing disease progression, improving patient outcomes, and reducing pain and disability.
This observational study revealed a significant association between Vitamin D and PTH levels, lipid profiles, and calcium homeostasis in patients with OA. Our findings indicate that OA patients commonly exhibit Vitamin D insufficiency, which is correlated with altered lipid metabolism and elevated PTH levels, suggesting a complex interplay that potentially influences disease progression and symptomatology. The study underscores the importance of Vitamin D in maintaining bone health and suggests a potential link between lipid profiles and OA severity. These insights highlight the importance of Vitamin D status and lipid management in the clinical management of OA, highlighting the need for further research to explore the therapeutic implications of Vitamin D supplementation in OA patients. By establishing a foundational understanding of these relationships, our study contributes to the broader discourse on the metabolic factors influencing OA and underscores the potential of targeted interventions to improve patient outcomes.
Assessing and managing Vitamin D levels, parathyroid hormone (PTH) concentrations, and lipid profiles in patients with osteoarthritis (OA) may be crucial for optimizing disease management and improving patient outcomes, highlighting the importance of a comprehensive approach to address the complex metabolic interplay influencing OA progression.
References
- 1.Association between Serum Vitamin D Levels and Lipid Profiles: A Cross-Sectional Analysis-Scientific Reports. Available from: https://www.nature.com/articles/s41598-023-47872-5 [Last accessed on 2024 Jan 20]. [Google Scholar]
- 2.Khundmiri SJ, Murray RD, Lederer E. PTH and Vitamin D. Compr Physiol 2016;6:561-601. [Google Scholar]
- 3.Goździalska A, Jaśkiewicz J, Knapik-Czajka M, Drąg J, Gawlik M, Cieśla M, et al. Association of calcium and phosphate balance, vitamin D, PTH, and calcitonin in patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2016;41:693-7. [Google Scholar]
- 4.Sahota O, Mundey MK, San P, Godber IM, Lawson N, Hosking DJ. The relationship between vitamin D and parathyroid hormone: Calcium homeostasis, bone turnover, and bone mineral density in postmenopausal women with established osteoporosis. Bone 2004;35:312-9. [Google Scholar]
- 5.Bobillier A, Wagner P, Whittier DE, Ecochard R, Boyd SK, Chapurlat R, et al. Association of Vitamin D and parathyroid hormone status with the aging-related decline of bone microarchitecture in older men: The prospective structure of aging men’s bones (STRAMBO) study. J Bone Miner Res 2022;37:1903-14. [Google Scholar]
- 6.Yarparvar A, Elmadfa I, Djazayery A, Abdollahi Z, Salehi F, Heshmat R. The Effects of Vitamin D supplementation on lipid and inflammatory profile of healthy adolescent boys: A randomized controlled trial. Nutrients 2020;12:1213. [Google Scholar]
- 7.Qu Z, Yang F, Yan Y, Huang J, Zhao J, Hong J, et al. A Mendelian randomization study on the role of serum parathyroid hormone and 25-hydroxyvitamin D in osteoarthritis. Osteoarthritis Cartilage 2021;29:1282-90. [Google Scholar]
- 8.Zhang FF, Driban JB, Lo GH, Price LL, Booth S, Eaton CB, et al. Vitamin D deficiency is associated with progression of knee osteoarthritis. J Nutr 2014;144:2002-8. [Google Scholar]
- 9.USDA ARS Online Magazine Low Vitamin D Linked to Osteoarthritis. Available from: https://agresearchmag.ars.usda.gov/2015/jul/vitamin [Last accessed on 2024 Feb 04]. [Google Scholar]
- 10.Alabajos-Cea A, Herrero-Manley L, Suso-Martí L, Viosca-Herrero E, Cuenca-Martínez F, Varangot-Reille C, et al. The role of Vitamin D in early knee osteoarthritis and its relationship with their physical and psychological status. Nutrients 2021;13:4035. [Google Scholar]
- 11.Raposo L, Martins S, Ferreira D, Guimarães JT, Santos AC. Vitamin D, parathyroid hormone and metabolic syndrome-the PORMETS study. BMC Endocr Disord 2017;17:71. [Google Scholar]
- 12.Danese VC, Pepe J, Ferrone F, Colangelo L, De Martino V, Nieddu L, et al. The mutual interplay between bone, glucose and lipid metabolism: The role of vitamin D and PTH. Nutrients 2023;15:2998. [Google Scholar]
- 13.Annamalai R, Sujhithra A, Danis Vijay D. Association between vitamin D and knee osteoarthritis in Indian population: A systematic review and meta-analysis. J Clin Orthop Trauma 2023;46:102278. [Google Scholar]
- 14.Wang Z, Zhu Z, Pan F, Zheng S, Parameswaran V, Blizzard L, et al. Long-term effects of vitamin D supplementation and maintaining sufficient vitamin D on knee osteoarthritis over 5 years. Arthritis Res Ther 2023;25:178. [Google Scholar]
- 15.Yu G, Lin Y, Dai H, Xu J, Liu J. Association between serum 25-hydroxyvitamin D and osteoarthritis: A national population-based analysis of NHANES 2001-2018. Front Nutr 2023;10:1016809. [Google Scholar]