Selective nerve root block (SNRB) is a technique to treat and delay surgery for patients with lumbar radiculopathy who failed to respond for oral medications.
Dr. Naveen Selvamuthu, Department of Orthopeadics, Rajah Muthiah Medical College, Government Cuddalore Medical College, Chidambaram, Tamil Nadu, India. E-mail: dr.navy278@gmail.com
Introduction: The aim of this research is to study the clinical outcome and symptomatic improvement for patients with lumbar radiculopathy treated with selective nerve root block (SNRB) under fluoroscopic guidance. This non-surgical management can be used at various sites including cervical and lumbar regions and also can prevent early surgeries for patients with radiculopathy.
Materials and Methods: Thirty patients with low back pain with or without sciatica were treated by fluoroscopic-guided nerve root block (F-NRB) as therapeutic management in government Cuddalore Medical College during the period of August 2020–2022. These patients were studied prospectively for the period of 6 months and assessed with the Visual Analog Scale to quantify the severity of pain.
Discussion: 30 patients underwent S-NRB, in that 26 patients had an immediate recovery and four patients showed delayed recovery, so that four patients underwent surgery. At the 3rd and 6th-month follow-up, 14 patients did not have a recurrence of pain and 12 had a recurrence of pain. Out of these 12 patients who had pain recurrence, only four needed surgery and the rest were managed conservatively. Accordingly, out of 30 patients who underwent SNRB, only eight patients needed surgery.
Conclusion: Patients with lumbar radiculopathy caused by lumbar disc prolapse and foraminal stenosis have good clinical outcomes by SNRB. This method had good pain relief for about 86% of patients immediately and prevented surgery for about 73.3% of patients. Out of 26.7% who underwent surgery, the majority had sequestrated discs. Thus, the sequestrated disc is one of the major negative predictors of successful outcomes for SNRB.
Keywords: Lumbar radiculopathy, selective nerve root block, sciatica.
Lumbar radiculopathy is one of the common causes of morbidity worldwide [1]. It is well defined as the radiating pain from the lower back along the course of a nerve which is compressed by a herniated lumbar disc [1, 2]. The pain may also be severe to affect day-to-day activities. The radicular pain may also be associated with sensory dysfunction such as numbness, paresthesia, tingling sensation, and motor deficits such as muscle weakness and loss of reflexes. The radicular pain from the sciatic nerve root along its course is known as sciatica [1,3]. A herniated disc is the most common cause of nerve root compression. Other causes of nerve root compression other than herniated discs include foraminal stenosis, tumors, cysts, and inflammation [1,4]. The majority of patients with radicular pain are treated conservatively with adequate rest, physiotherapy, analgesics, and anti-inflammatory drugs. Patients with continuous pain despite conservative management for 6–8 weeks need the next level of management [4-6]. Surgery is an immediate option for patients only with red flag signs such as acute foot drop and acute bladder incontinence [7]. The effectiveness of surgery for chronic radicular pain with sensory and motor dysfunction without red flag signs has been questioned in the number of literatures [8]. The reluctance to surgery and potential surgical complications such as recurrence, injury to the nerve root, discitis, and also complications due to anesthesia make selective nerve root block (SNRB) an effective alternative for patients with failed conservative management [9]. The pain due to lumbar disc prolapse is due to a pathological process either due to compression of the nerve root mechanically or due to perineural inflammation. Thus, SNRB with corticosteroids has good functional results as the primary pathology for pain is inflammation [9]. This research prospectively study patients treated with SNRB with corticosteroids to assess the effectiveness, limitations, and predictive factors for successful SNRB.
This study was done in the period of August 2020–2022 in patients with lumbar radiculopathy due to disc herniation.
Inclusion criteria
- Failed conservative management
- Visual Analog Scale (VAS) 8/10
- Absence of red flag signs such as acute foot drop and bladder involvement.
Exclusion criteria
- Gross neurological deficit
- Patients with cauda equina syndrome
- Multilevel disc prolapses (>3 levels)
- Previously operated cases
- Patients with bladder involvement
- Radicular pain due to infection and tumors
- Traumatic radiculopathy.
Clinical parameters
Patients are assessed for age, sex, symptom duration, affected side, level of lesion, type of job, the presence and absence of neurological symptoms, VAS, and straight leg raise test, and all these details are documented.
Investigations
X-ray LS spine – anteroposterior and lateral view, magnetic resonance imaging (MRI), and all necessary basic investigations are done.
Follow-up
The VAS scores of all patients studied under this study were documented preoperatively and at 1, 3, and 6 months.
SNRB techniques
After explaining the risks and complications, written consent is obtained from the patient. The patient is made to lie on a radiolucent table in the prone position (Fig. 1a). The oblique view of the spine is obtained in the image intensifier to visualize the “Scotty dog.” The overlying skin is anesthetized with local anesthesia (5 mL of 2% lignocaine). The safe triangle is identified which is inferior to the pedicle and superior to the nerve root. A 23-G spinal needle is introduced into the safe triangle at the neck of the Scotty dog. After confirming the position of the spinal needle in both anteroposterior and lateral views (Fig. 1b), 1 mL of iohexol dye is injected to identify the targeted nerve root (Fig. 1c). The pain is reproduced in all patients to confirm the nerve root.
After confirming the nerve root both fluoroscopically using dye (Fig. 1d-g) and reproduction of pain, 2 mL of 0.5% bupivacaine (light) along with 80 mg of triamcinolone injected around the targeted nerve root (one or two levels). A sterile dressing is done. The patient is observed for about 1 h and advised to rest for 1 day. Postoperatively allowed for activities within the comfort and one dose of gabapentin at night is continued for the next 2 weeks. Patients are then followed for 1st, 3rd, and 6th months. During follow-up, the pre-injection X-rays and MRI of patients who had good pain relief and who had recurrence are assessed again and documented separately to study the factors deterring the outcome and also to select appropriate patients [10, 11]. The statistical analyses were made through descriptive analysis using OriginPro8 software.
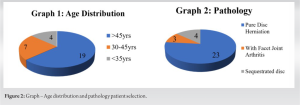
In our study, a total of 30 patients were selected with above-mentioned criteria and underwent SNRB by a single surgeon as described above and followed up for up to 6 months. Out of the selected 30 patients, 17 (56.6%) were female and 13 (43.3%) were male. 19 (63.3%) patients were aged above 45 years old (standard deviation [SD] ± 6.79), 7 (23.3%) patients were in age between 30 and 45 years old (SD ± 2.87), and 4 (13.3%) patients were below the age of 30 years old (SD ± 1.63) (Fig. 2 and Graph 1). In the study group, 18 (60%) patients had right-sided sciatica and 12 (40%) patients had left-sided sciatica. SNRB is done at a single level for 21 (70%) patients and at two levels for 9 (30%) patients. In this group, four patients had sequestrated discs, three patients had facet joint arthritis, and the remaining patients had only disc herniation (Fig. 2).
All patients who underwent SNRB were studied immediately after the procedure and followed up after the 1st, 3rd, and 6th months of the procedure using VAS score. Overall, from these 30 patients, 26 (86.6%) patients had immediate recovery and 4 (13.3%) patients did not respond. Out of 26 patients who had an immediate recovery, 14 (46.6%) patients did not have any recurrence of pain and the other 12 patients had the pain recurrence at the 6th-month follow-up. Of these 12 patients who had a recurrence of pain, 8 (26.6%) were improved with further conservative management and four failed to respond with conservative management. Out of the 30 patients who had undergone SNRB, only 8 (26.6%) needed surgery (four who did not recover immediately and four who had recurrence of pain and failed to respond with further management) (Fig. 3). This study shows no difference in outcome with respect to age, gender side, though the sequestrated disc disease did not respond well with SNRB.
The majority of patients with radicular pain are treated with conservative treatment [12]. Cases with red flag signs usually need surgery as immediate intervention. Surgery is usually advised for patients who have failed conservative management [12-16]. Due to the risk and complications of surgery such as dura rupture, cerebrospinal fluid leakage, infection, and a high chance of recurrence and also due to the cost of surgery, most patients are reluctant to have surgery [5,8]. In view of this, there is a need for treatment modality between conservative treatment and surgery. Fluoroscopic-guided selective nerve root serves this purpose to some extent. This non-surgical management does not need general anesthesia, long hospital stays, and cost-effective compared to surgery [17-20]. The majority of studies have shown that SNRB has excellent short-term results and can be used to delay surgery in the majority of cases without any red flag signs. However, the chances of recurrence at long-term follow-up are high in the study done by Kim et al. and there is a significant reduction in the VAS score immediately after the procedure for most of the patients [21]. VAS score reduced immediately for the majority of patients in our study also [10,22,23]. Kanayama et al. studied that patient with facet joint arthritis has poorer outcomes with SNRB than with patients who have only lumbar disc herniation (LDH) [12]. The present study also has similar results, and patients with facet joint arthritis have poor outcomes. Studies have shown that patients with higher pre-injection VAS scores and significant sensory disturbances have not responded as well as patients with lower pre-injection VAS scores and without significant sensory disturbances. We had similar results; patients with higher pre-injection VAS scores had an immediate need for surgery. Lee et al. studied MRI-based findings for clinical outcomes for SNRB and found that LDH in the foraminal–extraforaminal zone had good outcomes. In our study, we found that patients with sequestrated discs have poor clinical outcomes and also found that the level of disc herniation and side of herniation has no significant relation with outcome [24]. Kanna et al. studied the relation between radiculogram appearance and clinical outcome, and they found that four clinical patterns arm, arrow, linear, and splash pattern interestingly in our study patients with splash patterns have poor clinical outcomes. The MRI of patients with splash patterns is studied retrospectively and there is no significant correlation between MRI findings and splash patterns [25]. Although there are several studies for SNRB, the inclusion and exclusion criteria of these studies vary a lot. There are no standard criteria for selecting and excluding patients with SNRB. However, according to the majority of studies including our study, most patients who have failed to respond by conservative management and without any severe acute symptoms responded well to SNRB immediately [6,26-28]. The chance of recurrence of pain at 6-month follow-up is higher, only 20–30% of patients have long-term pain relief [2]. Thus, according to available literature and technology, SNRB can used to delay surgery in a greater number of people but its role in preventing surgery and predictors of successful long-term outcomes needs to be studied further with standardized inclusion and exclusion criteria. With some contraindications such as active infection over the injection site, allergic to contrast material was used to avoid adverse effects such as anaphylaxis.
Patients with lumbar radiculopathy caused by lumbar disc prolapse and foraminal stenosis have good clinical outcomes by SNRB. This non-surgical management had good pain relief immediately for about 86% of patients and prevented surgery for about 73.3% of patients. Out of 26.7% who underwent surgery, the majority had sequestrated discs. Thus, the sequestrated disc is one of the major negative predictors of successful outcomes for SNRB.
SNRB holds an important position in managing intervertebral disc prolapse with radiculopathy. However, it has some limitations such as sequestrated disc disease, lysthesis which gives symptomatic relief for patients with chronic radiculopathic pain.
References
- 1.Alexander CE, Varacallo M. Lumbosacral radiculopathy. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/nbk430837 [Last accessed on 2022 Sep 07]. [Google Scholar]
- 2.Arun Kumar K, Jayaprasad S, Senthil K, Lohith H, Jayaprakash KV. The outcomes of selective nerve root block for disc induced lumbar radiculopathy. Malays Orthop J 2015;9:17-22. [Google Scholar]
- 3.Wenger HC, Cifu AS. Treatment of low back pain. JAMA 2017;318:743-4. [Google Scholar]
- 4.Koes BW, Van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ 2007;334:1313-7. [Google Scholar]
- 5.Chou R, Loeser JD, Owens DK, Rosenquist RW, Atlas SJ, Baisden J, et al. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: An evidence-based clinical practice guideline from the American Pain Society. Spine (Phila Pa 1976) 2009;34:1066-77. [Google Scholar]
- 6.Pfirrmann CW, Oberholzer PA, Zanetti M, Boos N, Trudell DJ, Resnick D, et al. Selective nerve root blocks for the treatment of sciatica: Evaluation of injection site and effectiveness--a study with patients and cadavers. Radiology 2001;221:704-11. [Google Scholar]
- 7.Kikuchi S. Anatomical and experimental studies of nerve root infiltration. Nihon Seikeigeka Gakkai Zasshi 1982;56:605-14. [Google Scholar]
- 8.Negrini S, Giovannoni S, Minozzi S, Barneschi G, Bonaiuti D, Bussotti A, et al. Diagnostic therapeutic flow-charts for low back pain patients: The Italian clinical guidelines. Eura Medicophys 2006;42:151-70. [Google Scholar]
- 9.Skovrlj B, Gilligan J, Cutler HS, Qureshi SA. Minimally invasive procedures on the lumbar spine. World J Clin Cases 2015;3:1-9. [Google Scholar]
- 10.Beynon R, Elwenspoek MM, Sheppard A, Higgins JN, Kolias AG, Laing RJ, et al. The utility of diagnostic selective nerve root blocks in the management of patients with lumbar radiculopathy: A systematic review. BMJ Open 2019;9:e025790. [Google Scholar]
- 11.Kim SB, Jeon TS, Park WK, Jo SK, Kim YS, Hwang CM. Transforaminal selective nerve root blocks for treating single lumbosacral radiculopathy: The short-term outcome and efficiency. J Korean Orthop Assoc 2009;44:619-26. [Google Scholar]
- 12.Kanayama M, Oha F, Hashimoto T. What types of degenerative lumbar pathologies respond to nerve root injection? A retrospective review of six hundred and forty one cases. Int Orthop 2015;39:1379-82. [Google Scholar]
- 13.Heliövaara M, Impivaara O, Sievers K, Melkas T, Knekt P, Korpi J, et al. Lumbar disc syndrome in Finland. J Epidemiol Community Health 1987;41:251-8. [Google Scholar]
- 14.Jacobs WC, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R, et al. Surgery versus conservative management of sciatica due to a lumbar herniated disc: A systematic review. Eur Spine J 2011;20:513-22. [Google Scholar]
- 15.Solberg TK, Nygaard OP, Sjaavik K, Hofoss D, Ingebrigtsen T. The risk of “getting worse” after lumbar microdiscectomy. Eur Spine J 2005;14:49-54. [Google Scholar]
- 16.Vad VB, Bhat AL, Lutz GE, Cammisa F. Transforaminal epidural steroid injections in lumbosacral radiculopathy: A prospective randomized study. Spine (Phila Pa 1976) 2005;27:11-6. [Google Scholar]
- 17.Datta S, Manchikanti L, Falco FJ, Calodney AK, Atluri S, Benyamin RM, et al. Diagnostic utility of selective nerve root blocks in the diagnosis of lumbosacral radicular pain: Systematic review and update of current evidence. Pain Physician 2013;16:SE97-124. [Google Scholar]
- 18.Mallinson PI, Tapping CR, Bartlett R, Maliakal P. Factors that affect the efficacy of fluoroscopically guided selective spinal nerve root block in the treatment of radicular pain: A prospective cohort study. Can Assoc Radiol J 2013;64:370-5. [Google Scholar]
- 19.Cooper G, Lutz GE, Boachie-Adjei O, Lin J. Effectiveness of transforaminal epidural steroid injections in patients with degenerative lumbar scoliotic stenosis and radiculopathy. Pain Physician 2004;7:311-7. [Google Scholar]
- 20.Herron LD. Selective nerve root block in patient selection for lumbar surgery: Surgical results. J Spinal Disord 1989;2:75-9. [Google Scholar]
- 21.Kim J, Hur JW, Lee JB, Park JY. Surgery versus nerve blocks for lumbar disc herniation: Quantitative analysis of radiological factors as a predictor for successful outcomes. J Korean Neurosurg Soc 2016;59:478-84. [Google Scholar]
- 22.Wagner AL. Selective lumbar nerve root blocks with CT fluoroscopic guidance: Technique, results, procedure time, and radiation dose. AJNR Am J Neuroradiol 2004;25:1592-4. [Google Scholar]
- 23.McCormick Z, Cushman D, Casey E, Garvan C, Kennedy DJ, Plastaras C. Factors associated with pain reduction after transforaminal epidural steroid injection for lumbosacral radicular pain. Arch Phys Med Rehabil 2014;95:2350-6. [Google Scholar]
- 24.Lee JW, Kim SH, Lee IS, Choi JA, Choi JY, Hong SH, et al. Therapeutic effect and outcome predictors of sciatica treated using transforaminal epidural steroid injection. AJR Am J Roentgenol 2006;187:1427-31. [Google Scholar]
- 25.Kanna RM, Shetty AP, Rajasekaran S. Predictors of successful outcomes of selective nerve root blocks for acute lumbar disc herniation. Global Spine J 2019;9:473-9. [Google Scholar]
- 26.Zhang YG, Sun Z, Zhang Z, Liu J, Guo X. Risk factors for lumbar intervertebral disc herniation in Chinese population: A case-control study. Spine (Phila Pa 1976) 2009;34:E918-22. [Google Scholar]
- 27.Luoma K, Vehmas T, Raininko R, Luukkonen R, Riihimäki H. Lumbosacral transitional vertebra: Relation to disc degeneration and low back pain. Spine (Phila Pa 1976) 2004;29:200-5. [Google Scholar]
- 28.Wigh RE, Anthony HF Jr. Transitional lumbosacral discs. Probability of herniation. Spine (Phila Pa 1976) 1981;6:168-71. [Google Scholar]