This article emphasizes prompt diagnosis and effective treatment for elbow septic arthritis as the functional outcome of the affected joints depends on the time interval between the onset of the symptoms and surgical intervention.
Dr. Esra Mustafa Hamed Abdalla, Department of Family Medicine, Michigan, State University, East Lansing, Michigan, USA. E-mail: esramustafahamed@gmail.com
Introduction: Septic arthritis of the elbow is a rare, serious condition that requires prompt medical attention. With proper treatment, most individuals are able to recover fully and regain function in the affected joint. However, without treatment, septic arthritis of the elbow can lead to long-term joint damage and disability.
Case Report: This case report presents a rare occurrence of septic arthritis in the elbow joint of a 23-year-old male patient. The patient presented with pain, swelling, and limited range of motion in the affected joint. After a thorough clinical assessment and diagnostic imaging, a diagnosis of septic arthritis was confirmed. The patient was promptly treated with intravenous antibiotics and joint aspiration to drain the infected fluid. Following treatment, the patient showed significant improvement in symptoms and regained full range of motion in the affected elbow joint.
Conclusion: Prompt drainage and washout of the impacted joint are recommended for both diagnostic and therapeutic reasons. The functional outcome of the affected joints depends on the time interval between the onset of the symptoms and surgical intervention and it is crucial to quickly and precisely identify the presence of microorganisms in the synovial fluid.
Keywords: Elbow, small joint, septic arthritis, adult.
Septic arthritis of the elbow, also known as infectious arthritis or pyogenic arthritis, is very uncommon. In a previous study, it accounted for 6.9% of all cases of SA [1]. It is a serious emergency condition prompting early recognition, appropriate drainage procedures, and antibiotic treatment to minimize irreversible joint damage. This infection is dangerous because it may lead to fulminant sepsis. In the literature, mortality is high at 11.5% with a significant additional morbidity of 31.6% [2]. Septic arthritis classically presents with acute-onset monoarticular joint pain, fever, swelling, and a reluctance or refusal to move the affected joint. Fever may be present in 40–60% of cases but is a non-specific finding [3]. Early intervention in advance of culture results is a safe and reasonable option in patients in whom septic arthritis of the elbow joint is strongly suspected. Any delay in diagnosis or ineffective treatment may increase morbidity and is associated with complications such as osteomyelitis, avascular necrosis, sepsis, bone and cartilage destruction, osteoarthritis, and ankylosis eventually [4]. The most common organisms isolated in septic arthritis are Staphylococcus aureus, Streptococcus pyogenes, and methicillin-resistant S. aureus, accounting for 53%, 15%, and 13% of cases, respectively [2], S. aureus is the most common infecting organism in adults. The knee is the most commonly affected joint in adults followed by the hip. The cornerstones of treatment include adequate drainage and antimicrobials. The initial choice of antibiotics is generally based on epidemiological factors, as well as age, risk factors, and clinical presentation in addition to Gram stain results. The benefits of surgical drainage include the ability to remove nonviable tissue, obtain biopsies after debridement, and evaluate for a potential synovectomy, arthroscopic and open arthrotomy can both be used as treatment options for the management of an acute bacterial septic joint [3]. There are little data available to address the clinical presentation, management, and outcomes of septic arthritis of the elbow joint [5]. Previous clinical studies were limited to children or included immunocompromised patients. A better understanding of the diagnosis and management of septic arthritis of the elbow is needed to improve its prognosis. This paper reports a case of septic arthritis of the elbow in a 23-year-old man treated with open arthrotomy with good clinical outcome.
A 23-year-old man presented to Hassahisa Teaching Hospital’s emergency department with right elbow swelling, fever, and pain. The condition started 4 days before presentation as a spontaneous swelling of the right elbow joint that gradually increased in size, associated with throbbing pain and fever. The pain worsened by joint movement and was relieved by analgesics. The fever was high-grade, intermittent, and relieved by antipyretics. He had no history of trauma or a similar condition. His past medical history included a recently treated urinary tract infection.
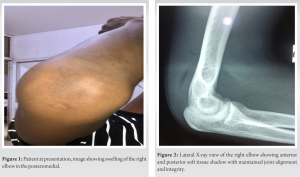
The patient presented with his right elbow flexed at 90, internally rotated, and supported by his left arm. Physical examination revealed redness, swelling, and local heat mainly in the posterior aspect of the right elbow (Fig. 1). There are no draining sinuses or surgical scars. The range of motion of his right elbow was severely restricted. Plain X-rays of the right elbow showed swollen soft tissue without signs of osteolysis (Fig. 2). Laboratory studies demonstrate a white cell count of 48000/mm3, elevated inflammatory markers such as C-reactive protein of 37.8 mg/dL, and an erythrocyte sedimentation rate (ESR) 45. A high-resolution right elbow joint region with complementary color doppler sonography revealed the presence of a particulate turbid joint effusion around the right elbow and the normal appearance of the muscle and vascular structures.
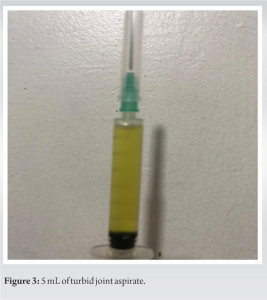
The patient underwent arthrocentesis, from which a total of 5 mL of macroscopically inflammatory synovial fluids was obtained (Fig. 3) and sent to culture and sensitivity test which revealed later Gram-positive cocci (S. aureus) sensitive to doxycycline and ciprofloxacin, due to lack of local facilities, no biochemistry or microscopic analysis of the fluid was performed.
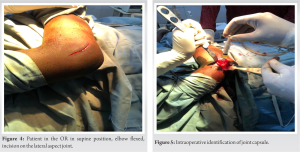
Based on these findings, a diagnosis of septic arthritis of the right elbow was made and the patient was prepared and transferred to the theater. Under aseptic conditions and general anesthesia, open arthrotomy and debridement of the right elbow were performed. The patient was in a supine position with the left upper limb hanging down on an arm board and the right limb flexed 90° at the elbow. An incision was made over the lateral epicondyle and extended 5cm proximally and 2.5 cm distally (Fig. 4).
The joint capsule was visualized by separation of the triceps from the extensor carpi radialis longus anteriorly (Fig. 5). The capsule was then incised carefully, and the pus was evacuated. The joint was irrigated with 3000 mL saline, (Fig. 6), and the skin was closed loosely over drains (Fig. 7). To protect the elbow, a splint was fixed for a period of 1 week.
On the 3rd day of the surgery, the culture of the first aspiration of the joint revealed S. aureus. The antibiotic was changed to ciproflacxain infusion for 5 days and he was discharged with oral ciproflacxain plus doxycycline which continued for 4 weeks. He came for follow-up after 1 week, the wound was reexamined, and no signs of infection were found. The arm sling was removed and physiotherapy was started at 2-week follow-up. CRP was 12 and ESR was 40. Regular follow-up visits thereafter went uneventful, the last being 1-month post-operative with full elbow ROM, good wound healing, normalization of septic screening, CRP was 9, and ESR was 25. Plan for follow-up after 3 months.
Septic arthritis can affect anyone at any age, but it is more common in residents of deprived areas, the elderly, very young children, and smokers. Males account for a disproportionately high proportion, possibly due to higher rates of traumatic injury [6]. Risk factors vary according to the patient population. In a young population like this case, risk factors include diabetes, rheumatoid arthritis, intravenous drug use, acquired or pharmacologic immunosuppression, skin infection, penetrating trauma, and arthroscopic procedures [7]. Our patient had none of these factors other than being a male. Previous studies found that septic arthritis of the elbow can occur in otherwise healthy patients and causative factors and predisposing conditions to septic elbow were not identified in the majority of cases [8]. Infection of the elbow is rare. The presentation is variable, unpredictable and can easily be mistaken for other elbow conditions. A high index of suspicion is necessary for its diagnosis irrespective of patient age and medical status because patients usually present with subtle findings and have inconclusive laboratory results and there are few diagnostic algorithms available. Orthopedic surgeons must connect the history, clinical examination with laboratory and radiographic studies to exclude other diseases and get the right diagnosis as soon as possible as time is a crucial factor in septic arthritis, delayed diagnosis can lead to severe joint destruction and poor outcome. Clinical assessment is the most important factor in making the diagnosis and guiding the management process. Joint pain, joint swelling, and fever are the only findings that occur in more than 50% of patients [9]. The sensitivity of these symptoms in predicting diagnosis was 85%, 78%, and 57%, respectively. When it comes to laboratory findings, CRP levels of >10 mg/l and ESRs of >30 mm/h have a reported high combined sensitivity of up to 96% for acute septic arthritis [10]. In our case, the diagnosis was made clinically and was supported by high CRP and ESR levels. Joint aspiration and culture of the synovial fluid later confirmed our diagnosis. CRP is an acute phase protein that peaks after 48 h and decreases within 1 week if management is scessful. In this patient, it dropped from 37 at presentation to 14 after 1 week.
The culture of SF continues to be the gold standard for the diagnosis of SA. A review of published cases of septic arthritis found that S. aureus is the most common cause of native septic arthritis and it was cultured in 64% [11]. In view of the 11% mortality rate for septic arthritis [2], prompt initiation of appropriate antibiotic therapy and careful selection of treatment for each patient is essential to improve the prognosis of septic arthritis. Appropriate antibiotic treatment is the mainstay therapy in septic arthritis. In this patient, when a diagnosis of septic arthritis of the right elbow was made, the patient was admitted and the antibiotics regimen was based on likely causative organisms and was modified by results of culture and sensitivity testing after surgery. Because S. aureus is the most common pathogen in general, we used second-generation cephalosporin as an empirical antibiotic choice. We shifted to doxycycline as the sensitivity testing confirmed the sensitivity of S. aureus to doxycycline and ciprofloxacin. At least 2 weeks of intravenous antibiotics followed by oral treatment for 2–4 weeks was given under the recommended guideline. A previous study reported that in cases of typical Gram-positive infection, 2 weeks of intravenous antibiotic administration was enough to restore clinical symptoms and normalization of biological inflammatory markers [12]. Adequate drainage of a septic joint is the cornerstone of successful treatment. without drainage, rapid destruction of the joint proceeds quickly. Open drainage and lavage (arthroscopically or through arthrotomy) are strongly recommended. Head-to-head comparisons have not yet provided decisive answers regarding the benefits of one surgical modality over another [13]. So far, to our knowledge, no studies are available comparing arthroscopy and open arthrotomy exclusively in infections of the elbow. By comparison, a retrospective review of 46 cases of septic arthritis in 46 patients found the arthroscopic treatment to be indicated in all patients who have septic arthritis of native joints [14]. Arthrotomy is the best procedure for bacteria deeply embedded in a joint and for loculations. It is especially helpful for drainage of the shoulders and hips. Böhler et al. found open arthrotomy to be superior to arthroscopy for septic arthritis of the shoulder [15]. There is ongoing discussion regarding the selection of surgical procedures. It may be based on the surgeon’s preference most of the time, where comfort and expertise may influence the decision of the surgeon. However, secondary infection in open wounds is the most common complication for open drainage techniques.
Septic arthritis is a potentially devastating disease that may cause permanent disability or even death. Prompt drainage and washout of the impacted joint are recommended for both diagnostic and therapeutic reasons. The functional outcome of the affected joints depends on the time interval between the onset of the symptoms and surgical intervention and it is crucial to quickly and precisely identify the presence of microorganisms in the synovial fluid.
This report describes a rare case of septic arthritis of the elbow, a potentially life-threatening condition that requires prompt diagnosis and treatment to prevent further complications. The report hopes to contribute to the expedient recognition of this condition, which is crucial to the preservation of arm function for these patients.
References
- 1.Kennedy N, Chambers ST, Nolan I, Gallagher K, Werno A, Browne M. Native joint septic arthritis: Epidemiology, clinical features, and microbiological causes in a New Zealand population. J Rheumatol 2015;42:2392-7. [Google Scholar]
- 2.Weston VC, Jones AC, Bradbury N, Fawthrop F, Doherty M. Clinical features and outcome of septic arthritis in a single UK Health District 1982-1991. Ann Rheum Dis 1999;58:214-9. [Google Scholar]
- 3.Hassan AS, Rao A, Manadan AM, Block JA. Peripheral bacterial septic arthritis: Review of diagnosis and management. J Clin Rheumatol 2017;23:435-42. [Google Scholar]
- 4.Farby G, Meire E. Septic arthritis of the hip in children: Poor results after late and inadequate treatment. J Pediatr Orthop 1983;3:461-6. [Google Scholar]
- 5.Van den Ende KI, Steinmann SP. Arthroscopic treatment of septic arthritis of the elbow. J Shoulder Elbow Surg 2012;21:1001-5. [Google Scholar]
- 6.Brusch, J. Medscape. Septic Arthritis; 2016. Available from: [Last accessed on 2017 Apr 04]. [Google Scholar]
- 7.Costales C, Butler-Wu SM. A real pain: Diagnostic quandaries and septic arthritis. Journal of Clin Microbiol 2017;56:e01358-17. [Google Scholar]
- 8.Moon JG, Bilaris S, Jeong WK, Kim JH. Clinical results after arthroscopic treatment for septic arthritis of the elbow joint. Arthroscopy 2014;30:673-8. [Google Scholar]
- 9.Margaretten ME, Kohlwes J, Moore D, Bent S. Does this adult patient have septic arthritis? JAMA 2007;297:1478-88. [Google Scholar]
- 10.Levine MJ, McGuire KJ, McGowan KL, Flynn JM. Assessment of the test characteristics of C-reactive protein for Septic arthritis in children. J Pediatr Orthop 2003;23:373-7. [Google Scholar]
- 11.Gobao VC, Alfishawy M, Smith C, Byers KE, Yassin M, Urish KL, et al. Risk factors, screening, and treatment challenges in Staphylococcus aureus native septic arthritis. Open Forum Infect Dis 2021;8:593. [Google Scholar]
- 12.Coakley G, Mathews C, Field M, Jones A, Kingsley G, Walker D, et al. BSR and BHPR, BOA, RCGP and BSAC guidelines for management of the hot swollen joint in adults. Rheumatology (Oxford) 2006;45:1039-41. [Google Scholar]
- 13.Donatto KC. Orthopedic management of septic arthritis. Rheum Dis Clin North Am 1998;24:275-86. [Google Scholar]
- 14.Aïm F, Delambre J, Bauer T, Hardy P. Efficacy of arthroscopic treatment for resolving infection in septic arthritis of native joints. Orthop Traumatol Surg Res 2015;101:61-4. [Google Scholar]
- 15.Böhler C, Pock A, Waldstein W, Staats K, Puchner SE, Holinka J, et al. Surgical treatment of shoulder infections: A comparison between arthroscopy and arthrotomy. J Shoulder Elbow Surg 2017;26:1915-21. [Google Scholar]