Recognizing unique fracture patterns, such as the flip lid phenomenon, understanding the distinctive mechanisms of injury involved, and navigating the challenges in diagnosis are essential for the effective management of unique tibial plateau fractures.
Dr. Janki Sharan Bhadani, Department of Orthopaedics, Paras HMRI Hospital, Patna, Bihar, India. E-mail: jsbhadani@gmail.com
Introduction: Bicondylar fractures are relatively common, yet those involving an elevated lateral tibial condyle fragment pose a unique challenge due to their atypical presentation. Existing classification systems inadequately describe this elevation, leading to varied terminology like “flip lid” or “reverse-Schatzker type” fractures in the literature.
Case Report: We present a case where the anterolateral osteochondral fragment was elevated and inverted, resulting from a rare mechanism where the left knee was crushed between two vehicles without axial force. This unusual mechanism spared typical signs of condylar widening or depression, with the fragment elevating but remaining submeniscal. This presented a challenge for fixation. The rotated fragment was accessed through an anterolateral approach with submeniscal arthrotomy, reduced, and fixed using raft screws of the lateral locking plate. The medial plateau fracture was stabilized through a posteromedial approach using an antiglide plate. Follow-up at 14 months showed satisfactory outcomes.
Conclusion: Unique injury mechanisms can give rise to distinct fracture types. When X-rays depict an elevated rather than depressed articular surface, suspicion should arise for an elevated, "popped up," or flip lid type fragment. Such cases require a high index of suspicion and a thorough preoperative evaluation using both X-rays and CT scans. Submeniscal arthrotomy is essential to assess meniscus integrity and allow direct visualization of the fracture fragment. Successful outcomes in managing these fractures are based on accurate diagnosis, thorough preoperative planning, and adherence to internal fixation principles.
Keywords: Elevated, popped up, flip lid, reverse tibial plateau fractures.
Tibial plateau fractures commonly occur in high-energy trauma, primarily due to road traffic accidents (RTA) [1]. The mechanism of injury is usually axial force along with varus or valgus force which decides the fracture involving medial or lateral or both plateaus. Several classifications are available based on X-ray and computed tomography (CT) to describe such fractures [2]. The most famous and easy to use is the Schatzker classification, with most fracture types fitting into this system. However, a few tibial plateau fractures cannot be classified based on any available recognized classification system, such as reverse Schatzker type IV [3], pivot type [4], and flip lid type [5]. We report a unique bicondylar fracture of the tibial plateau, which cannot be completely described using any available classification system. It is characterized by the anterolateral plateau fractured and everted upside-down without injuring the meniscus, resembling the elevated articular surface of the fractured lateral tibial plateau. The mechanism of injury is also unique in this case, as the proximal tibia is crushed between the bumpers of two vehicles, with no axial force. Pre-operative diagnosis and the decision of surgical approach are crucial for the reduction and fixation of such rare injuries. Neglecting the articular part during surgery can lead to disability, stiffness, and long-term osteoarthritis [6]. The goal of treating this type of fracture is to achieve articular congruity, absolute stability, limb alignment, and management of associated soft tissue injuries [7].
A 26-year-old male sustained an injury to his left knee and was diagnosed with a bicondylar fracture left proximal tibia. Initially managed elsewhere in an above-knee slab, elevation, rest, and analgesics, he was presented to us after 2 weeks. Upon examination, there was wrinkling of the skin suggesting subsidence of swelling and soft tissue compromise at the presentation [8]. Some healed abrasions on the anterior surface of the tibia were noted. Based on X-ray findings, a bicondylar fracture with an elevated lateral tibial condyle fragment was diagnosed, loosely classified as Schatzker type V, and AO/OTA type 31C, without considering the elevated fragment.
On careful evaluation of the CT scan, the anterolateral osteochondral fracture is elevated and almost rotated upside-down (Fig. 1). Luo’s three-column CT-based classification partially described it as type 3 [9, 10]. There is no description of the elevation of fracture fragments in any available classification. Thus, this case cannot be fully described using any of the available classifications. Such a pattern can be challenging to diagnose. Fracture configuration compromised soft tissue envelope, and surgical expertise are crucial in deciding the approach. In this case, a CT scan, showing breaching of the outer cortex in axial view, helped us decide on the anterolateral and posteromedial approach for optimal fragment reduction and plate placing.
The patient is positioned supine, and a tourniquet is applied on the proximal ipsilateral thigh and inflated (tourniquet time 75 mins, pressure 300 mmHg). A sandbag is placed under the knee to make it in slight flexion. The dual incision was used to reduce and fix this fracture. A posteromedial buttress plate through the posteromedial incision was applied. A skin incision at the posteromedial border was made, reduction of the apex of the fracture end and placement of the buttress plate behind the pes anserinus was done. An anterolateral incision was placed. Partial elevation of the iliotibial band from the tibia followed by sub-meniscal arthrotomy was done (Fig. 2). A flipped osteochondral fragment was seen as caught below the capsule with the articular surface facing down and the fractured surface facing up. The fragment was delivered out of the wound. The meniscus was seen intact. However, subchondral impaction of the bone was seen, which had to be elevated such that after fixing the fractured fragment the articular surface would label parallel before the fragment was fixed with an anterolateral plate and raft screw through the plate. An attempt was made to place it properly back into the joint, then the wound was closed in layers. The post-operative period was uneventful.
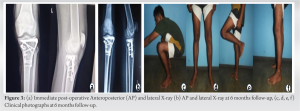
The range of motion exercise started on the 3rd post-operative day, after the subsidence of surgical pain. Partial weight-bearing started after 5–6 weeks and full weight-bearing started after 11–12 weeks post-operatively. Upon follow-up in the 5th month, the radiological union was visible. The range of motion of the left knee is 0–100°, painless with no crepitus (Fig. 3). He can do almost all his household activities though he was not able to use the Indian toilet and had difficulty sitting with the crossed leg on the floor. During the final follow-up at 14 months, the range of motion is increased to 0–110°. He can walk, play games, and run without any difficulty (Fig. 4).
There are a few unclassified fractures described in the literature like this case. Ho et al. reported a flip type of lateral tibial plateau fracture where the osteochondral fragment was elevated but unlike our case, it was not rotated upside-down and associated with lateral meniscus tear [5]. Chang et al. described a pivot-type lateral tibial plateau fracture, but unlike us, the flipped fracture fragment is associated with anterior cruciate ligament injury and no medial condyle fracture [4]. Another fracture that is not classified by the available classification system is known as the “reverse-Schatzker type IV” fracture. This term was first used by Yeoh et al., caused by instant fracture dislocation and characterized by valgus knee position with lateral plateau dislocated completely out and medial plateau in position [3]. This case can be described as a bicondylar fracture with the extreme type of flip lid or pivot fracture of the lateral plateau where the articular fragment of the lateral condyle is completely rotated upside down. The most common mechanism resulting in tibial plateau fracture is a valgus force with axial load, usually after a RTA [11]. The mechanism of injury is unique; in this case, the patient also sustained a fracture due to RTA when the proximal tibia compressed between two 2-wheelers with no axial force. Therefore, there was no condylar widening or depression rather the fracture fragment popped up and stayed submeniscal [12]. The elevated articular surface raises the challenge of diagnosis. Keeping a high degree of suspicion and the CT scan should be ideal for dealing with diagnostic dilemmas and pre-operative planning. CT helps in classifying the fracture and formulation of the surgical plan based on the sagittal, axial, and coronal cut of the CT scan [9, 10]. Associated meniscus injury is not uncommon in tibial plateau fractures. Kolb et al. reported that there is more than 80% risk of lateral meniscal lesions/impingement, in the case of significant widening or depression of lateral tibial plateau fracture [13]. It was suspected here due to the elevated lateral plateau fragment [14]. The magnetic resonance imaging (MRI) scan is recommended to rule out ligamentous or meniscal injury pre-operatively [15]. Arthroscopy as well as submeniscal arthrotomy is a well-known method for inspection of tibial plateau fracture as well as to diagnose ligament and meniscus tear intraoperatively as performed by Ho et al. [5, 16, 17]. Neither MRI nor arthroscopy was done in this case. We have done lateral submeniscal arthrotomy to confirm the diagnosis intraoperatively as well as inspection of the meniscus which was found to be intact. Unlike our case, Ho et al. also needed to repair the meniscus arthroscopically [5]. A dual plate was used in this case as recommended for bicondylar fracture. The lateral locking plate is neither ideal nor the screws through the plate would have an adequate grip and stabilizing effect on the opposite tibial plateau fracture fragment [18]. The risk of loss of reduction if a single plate is used for bicondylar fracture fixation [19-21].
This case presents a unique fracture pattern due to a distinct injury mechanism. The exact cause is challenging to determine but likely involves both valgus and varus forces, without axial force, as the knee was caught between two motorbikes. The rotated and elevated fracture fragment raises suspicion of meniscus injury, prompting consideration for pre-operative MRI or arthroscopy. Successful management relies on accurate diagnosis, achievable even with limited resources through careful imaging interpretation. Intraoperative confirmation can be obtained through submeniscal arthrotomy. Addressing the reduction of such fragments poses a challenge, but fixation becomes relatively straightforward with internal fixation, aiming for absolute stability.
Recognizing and addressing unique fracture patterns are crucial for the effective management of complex tibial plateau fractures. Understanding the distinct mechanisms of injury involved, which may deviate from typical presentations, can aid in accurate diagnosis and treatment planning. Clinicians should remain vigilant and consider advanced imaging modalities like CT scans and arthroscopy to confirm the diagnosis and ensure optimal management and satisfactory outcomes of such fractures.
References
- 1.Mohamed J, Bouaicha W, Lamouchi M, Ammar AB, Jaziri S, Daas S. Comparison of the results of the synthesis of Schatzker II and III tibial plateau fractures by screwing versus plate. Int Orthop 2023;47:2073-83. [Google Scholar]
- 2.Huitema JM, Van der Gaast N, Jaarsma RL, Doornberg JN, Edwards MJ, Hermans E. The effect of addition of 2DCT scans and 3DCT scans for the classification of tibial plateau fractures: A systematic review. Eur J Trauma Emerg Surg 2023;50:71-9. [Google Scholar]
- 3.Yeoh T, Iliopoulos E, Trompeter A. An unclassified tibial plateau fracture: Reverse Schatzker type IV. Chin J Traumatol 2018;21:211-5. [Google Scholar]
- 4.Chang EY, Berkes MB, Baker JC. The pivot fracture: An unusual tibial plateau fracture found in association with acute ACL injury. Skeletal Radiol 2022;51:1697-705. [Google Scholar]
- 5.Ho W, Chih WH, Yeh ML, Lin SF, Su WR, Chiang CH. “Flip lid” type of lateral tibia plateau fracture with a meniscus radial tear: A case report. Trauma Case Rep 2021;34:100496. [Google Scholar]
- 6.Jagdev SS, Pathak S, Kanani H, Salunke A. Functional outcome and incidence of osteoarthritis in operated tibial plateau fractures. Arch Bone Jt Surg 2018;6:508-6. [Google Scholar]
- 7.Prat-Fabregat S, Camacho-Carrasco P. Treatment strategy for tibial plateau fractures: An update. EFORT Open Rev 2016;1:225-32. [Google Scholar]
- 8.Borens O, Kloen P, Richmond J, Roederer G, Levine DS, Helfet DL. Minimally invasive treatment of pilon fractures with a low profile plate: Preliminary results in 17 cases. Arch Orthop Trauma Surg 2009;129:649-59. [Google Scholar]
- 9.Luo CF, Sun H, Zhang B, Zeng BF. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma 2010;24:683-92. [Google Scholar]
- 10.Fleming TA, Torrie PA, Murphy TA, Dodds AL, Engelke DM, Curwen CH, et al. The influence of pre-operative computed tomography (CT) on surgical approach and fixation for fractures of the tibial plateau. J Orthop 2023;42:50-3. [Google Scholar]
- 11.Malik S, Herron T, Mabrouk A, Rosenberg N. Tibial plateau fractures. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. [Google Scholar]
- 12.Hua K, Jiang X, Zha Y, Chen C, Zhang B, Mao Y. Retrospective analysis of 514 cases of tibial plateau fractures based on morphology and injury mechanism. J Orthop Surg Res 2019;14:267. [Google Scholar]
- 13.Kolb JP, Regier M, Vettorazzi E, Stiel N, Petersen JP, Behzadi C, et al. Prediction of meniscal and ligamentous injuries in lateral tibial plateau fractures based on measurements of lateral plateau widening on multidetector computed tomography scans. Biomed Res Int 2018;2018:5353820. [Google Scholar]
- 14.Lv H, Li W, Wang Y, Chen W, Yan X, Yuwen P, et al. Prediction model for tibial plateau fracture combined with meniscus injury. Front Surg 2023;10:1095961. [Google Scholar]
- 15.Thürig G, Korthaus A, Frosch KH, Krause M. The value of magnetic resonance imaging in the preoperative diagnosis of tibial plateau fractures: A systematic literature review. Eur J Trauma Emerg Surg 2023;49:661-79. [Google Scholar]
- 16.Buckley RE, Schneider P, Duffy PJ, Puloski S, Korley R, Martin CR. A sub-meniscal arthrotomy improves the medium-term patient outcome of tibial plateau fractures. Knee Surg Sports Traumatol Arthrosc 2019;27:837-44. [Google Scholar]
- 17.Hermanowicz K, Mrozek T, Góralczyk A, Malinowski K. Arthroscopy-assisted management of schatzker type III lateral tibial plateau fracture with interference screw fixation. Arthrosc Tech 2021;10:e1197-202. [Google Scholar]
- 18.Barei DP, O’Mara TJ, Taitsman LA, Dunbar RP, Nork SE. Frequency and fracture morphology of the posteromedial fragment in bicondylar tibial plateau fracture patterns. J Orthop Trauma 2008;22:176-82. [Google Scholar]
- 19.Musahl V, Tarkin I, Kobbe P, Tzioupis C, Siska PA, Pape HC. New trends and techniques in open reduction and internal fixation of fractures of the tibial plateau. J Bone Joint Surg Br 2009;91:426-33. [Google Scholar]
- 20.Wu CC, Tai CL. Plating treatment for tibial plateau fractures: A biomechanical comparison of buttress and tension band positions. Arch Orthop Trauma Surg 2007;127:19-24. [Google Scholar]
- 21.Çağlar C, Akcaalan S, Özaslan Hİ, Bozer M, Emre F, Uğurlu M. Comparative analysis of single lateral locked plate and double locked plate application in the treatment of bicondylar tibial plateau fractures. Cureus 2021;13:e19298. [Google Scholar]