Avascular necrosis rarely occurring in the diaphyseal region of long bones may lead to pathological fracture and it’s mandatory to follow-up for the rare possibility of malignant transformation post-surgical fixation of fracture.
Dr. Kishore Ragavendra Rajesh, Department of Orthopedic Surgery, Sri Ramachandra medical college and research institute, Porur, Chennai- 600116, India. E-mail: kishoreragavrajesh@gmail.com
Introduction: Epiphyseal infarcts are likely to be treated early because most are symptomatic. However, metaphyseal and diaphyseal infarcts are silent and are diagnosed incidentally. Sarcomas developing in the necrotic bone are extremely rare, but they have been reported in literature. Proximal third tibial shaft pathological fracture due to avascular necrosis (AVN) is an extremely rare occurrence.
Case Report: A 56-year-old lady presented with complaints of pain and inability to weight bear over the right leg following an alleged history of trivial trauma while doing household activities. The radiograph showed a transverse fracture at the junction of the proximal third and middle third of the shaft of the tibia. In view of the suspicion of pathological fracture, magnetic resonance imaging of the right leg was done which showed features of AVN. A core biopsy of the lesion was done to rule out tumors considering the risk of malignant transformation. Fixation of fracture was done with intramedullary interlocking nailing of the tibia. The 6-month post-operative follow-up clinical, pathological, and radiological outcome showed complete healing of the fracture. The stabilization of fracture alone without augmentation led to fracture healing.
Conclusion: AVN need not always occur in precarious areas such as the head of the femur, proximal radius, and distal fibula. Rarely, AVN of diaphyseal bone can lead to pathological fracture as illustrated in this case report. Fractures can heal following fixation, but the patient has to be followed up for the rare possibility of malignant transformation.
Keywords: Avascular necrosis, proximal tibia avascular necrosis, pathological fracture, core-needle biopsy, imaging.
The most common sites of avascular necrosis (AVN) of bone include the head of the femur, talus, and proximal pole of the scaphoid. AVN can be a crippling disease especially when it occurs in weight-bearing lower limb bones. It can occur due to traumatic or non-traumatic etiology, the latter being due to increased usage of corticosteroids as the most common cause. Pathogenesis in non-traumatic AVN includes inadequate blood supply, bone and bone marrow death, and problems with bone remodeling mechanisms. AVN can also be a cause of pathological fracture apart from an infection, neoplasm, osteoporosis, metabolic disorders, defective bone remodeling mechanisms, or iatrogenic causes (e.g., surgical defect). The disease most often affects bone epiphyses than metaphyses and diaphyses as the former lacks connection between bone epiphyses and local blood vessels and the consequent lack of collateral circulation leads to bone ischemia [1]. Disturbed circulation and ischemia leadnecrosis of osteocytes and damage to bone structure [1]. Epiphyseal infarcts are usually discovered and treated early since most of them are symptomatic. However, metaphyseal and diaphyseal infarcts are silent and are diagnosed incidentally in long bone AVN which itself is a rare entity [2, 3]. Bone tumors, especially sarcoma developing in necrotic bone, are extremely rare, but they have been reported in the literature. Proximal third tibial shaft pathological fracture due to AVN is an extremely rare occurrence which is being discussed in this case report.
A 56-year-old lady presented with complaints of pain and inability to weight bear over the right leg for 1 month following an alleged history of trivial trauma while doing household activities. On examination, there was swelling and tenderness present over the proximal third of the leg along with bone thickening and irregularity of the tibia in that region. Moreover, there was no obvious bony discontinuity or abnormality in that region. Radiographs (frontal and lateral projection) showed an undisplaced transverse fracture at the proximal third-middle third junction of the shaft of the tibia (arrow) (Fig. 1).
In view of the suspicion of pathological fracture, magnetic resonance imaging (MRI) of the right leg was done which showed bone infarct (arrow) and marrow edema (arrowhead) in proximal tibia. Pathological fracture (open arrow) is also visualized (Fig. 2) (Rationale:- CT was not done because MRI was done as many of the bone infarcts are precursors of malignant fibrous histiocytoma (MFH). Hence, it was safer to do a biopsy).
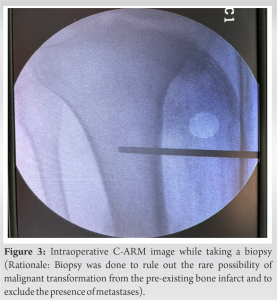
Further, core biopsy of the lesion was done under an image intensifier to rule out a tumor considering the risk of malignant transformation (Fig. 3). On light microscopy, areas of ischemic bone fragments with necrosis and hemorrhage admixed with fragments of lamellar bone and marrow elements were seen. There was no evidence of active infection, granuloma, or malignancy. The final histopathology report of AVN was rendered (Fig. 4).
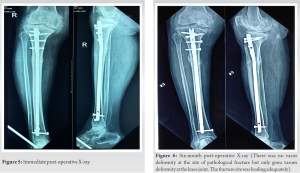
Bone aspirate from the right proximal tibia was sent for culture and sensitivity testing which showed no growth. Surgical fixation of the pathological fracture was done with closed intramedullary interlocking nailing of the tibia (Fig. 5).
The patient was started on full weight-bearing mobilization with walker support post-surgery. The 6-month post-operative follow-up, clinical, and radiological outcome was satisfactory. There was no varus deformity at the site of pathological fracture but only genu varum deformity at the knee joint. The fracture site was healing adequately. The stabilization of fracture alone without augmentation led to fracture healing (Fig. 6).
The incidence of osteonecrosis (ON) occurring in the tibia is relatively rare [4]. There is no evident sex predilection. There are several etiologies contributing to AVN. However, the pathogenesis of ON has triggered considerable debate, with no widely held consensus among experts. It has been generally agreed that the final common pathway of bone destruction is interruption of the bone supply and subsequent failure to deliver necessary nutrients to the bone [5].
As per Zhang et al., the number of osteonecrotic lesions was directly related to the dosage of steroids and that a very high dose, a peak dose of more than 200 mg, or a cumulative methylprednisolone equivalent dose of more than 4000 mg is a significant risk factor for multifocal ON with both epiphyseal and diaphyseal lesions. Patients with diaphyseal ON had received a significantly greater cumulative methylprednisolone equivalent dose than those with epiphyseal ON. Multifocal ON should be suspected in a patient with a diagnosis of ON in a shaft of a long bone [6]. Not all infarcts are symptomatic and patients remain symptom-free for a long time, which is especially true for diaphyseal and metaphyseal AVN [2, 3]. According to Stacy et al., bone infarcts can have a variety of appearances on radiographs, ranging from subtle ill-defined radiolucencies to more classic appearance of well-defined shell-like sclerosis [7]. Types of bone infarcts based on X-ray appearances (Table 1) [7]. Since the most common cause of pathological fractures in the elderly is metastatic lesions, the MRI images have to be carefully studied to differentiate necrotic lesions from metastasis (Table 2). AVN may rarely complicate to development of malignancy. Hence, in our patient, we preferred to do a core-needle biopsy to rule out malignant transformation. As this transformation is indolent, most secondary tumors occur in metaphyseal and diaphyseal regions (as epiphyseal infarcts are symptomatic at an early stage) [8, 9]. Most tumors occur in the proximal tibia and distal femur [7]. It is suggested that the transformation occurs due to local inflammation and the reparative process caused by the infarct. When the inflammatory processes become chronic, the likelihood of malignant transformation of reparative cells increases. Some of the histologic types such as MFH and fibrosarcomas, myxofibrosarcoma, and osteosarcoma affect areas where another lesion was already present; these include bone infarcts. The margin of the infarct where these processes are intensive might be prone to malignant transformation [10, 11]. MFHs penetrate the bone cortex easier than primary bone tumors because they arise from the periphery of the centrally located infarct. The avascular, necrotic infarct area makes it relatively immune to tumor penetration [7]. Till date, there are no published data on the prevalence of bone infarcts, so the percentage of bone infarcts that undergo sarcomatous degeneration is also unknown. The incidence of bone sarcoma arising in association with infarct is low, with percentages of 0.6–1% reported. However, the incidence may be underestimated because there may be cases in which bone sarcoma obscures the original bone infarct and the infarct is overlooked [7]. Moreover, uncomplicated bone infarcts are often asymptomatic, their prevalence is likely underestimated. The time interval between bone infarct and the development of bone sarcoma is unknown because the time of initial bone infarction is usually unknown. Sarcoma on X-ray presents as areas of osteolysis and is frequently associated with the periosteal reaction, a soft-tissue mass or a pathological fracture [7].
Long bone AVN need not always occur in precarious areas such as the head of the femur, proximal radius, and distal fibula. Rarely, AVN of a diaphyseal region of bone may lead to pathological fracture as illustrated in this case report. Infarct-associated sarcomas are rare occurring in chronic, mature infarcts, especially common in lower limbs around the knee joint. These patients do not have any defined risk factor for development in AVN, but a large set of patients might have multifocal AVN. Fractures can heal following fixation, but the patient has to be followed up for the rare possibility of malignant transformation.
Even though AVN rarely occurs in diaphyses of long bones, it may lead to pathological fractures. Surgeons should not hesitate to do higher investigations and biopsy to rule out the rarest possibility of malignant transformation.
References
- 1.Konarski W, Poboży T, Hordowicz M, Śliwczyński A, Kotela I, Krakowiak J, et al. Bone infarcts and tumorigenesis-is there a connection? A mini-mapping review. Int J Environ Res Public Health 2022;19:9282. [Google Scholar]
- 2.Torres FX, Kyriakos M. Bone infarct-associated osteosarcoma. Cancer 1992;70:2418-30. [Google Scholar]
- 3.Endo M, Yoshida T, Yamamoto H, Ishii T, Setsu N, Kohashi K, et al. Low-grade central osteosarcoma arising from bone infarct. Hum Pathol 2013;44:1184-9. [Google Scholar]
- 4.McLeod JM, Ng A, Kruse DL, Stone PA. Nontraumatic osteonecrosis of distal tibia: A case presentation and review of literature. J Foot Ankle Surg 2017;56:158-66. [Google Scholar]
- 5.Powell C, Chang C, Eric Gershwin M. Current concepts on the pathogenesis and natural history of steroid-induced osteonecrosis. Clin Rev Allergy Immunol 2011;41:102-13. [Google Scholar]
- 6.Zhang NF, Li ZR, Wei HY, Liu ZH, Hernigou P. Steroid induced osteonecrosis: The number of lesions is related to the dosage. J Bone Joint Surg Br 2008;90:1239-43. [Google Scholar]
- 7.Stacy GS, Lo R, Montag A. Infarct associated bone sarcomas: Multimodality imaging findings. Am J Roentgenol 2015;205:W432-41. [Google Scholar]
- 8.Goel R, GMC K. Low grade central osteosarcoma arising from bone Infarct: A case report. Int J Innov Sci Res Technol 2018;3:358–60. [Google Scholar]
- 9.Sivrioglu AK, Aribal S, Onder H. Secondary multifocal osteosarcoma developing in the background of bone infarct. BMJ Case Rep 2017;2017:bcr2017220293. [Google Scholar]
- 10.Kayser D, Walton Z, Bruner E, Chapin RW. Myxofibrosarcoma: First report of myxofibrosarcoma of bone arising at a bone infarct. Skeletal Radiol 2017;46:1143-7. [Google Scholar]
- 11.Yalcinkaya U, Cetintas SK, Bilgen MS, Yazici Z, Sevinir B, Aydinli U. Secondary osteosarcoma diagnosed in a single institution (7 cases in 10 years). Acta Med Mediterr 2015;31:875-81. [Google Scholar]