Bilateral proximal tibiofibular joint subluxation can be effectively diagnosed with detailed imaging and managed conservatively, particularly in young athletes with no significant ligament laxity, pain, or dysfunction.
Dr. Vijay Kumar Jain, Department of Orthopaedics, Atal Bihari Vajpayee Institute of Medical Sciences, Dr Ram Manohar Lohia Hospital, New Delhi, India. E-mail: drvijayortho@gmail.com
Introduction: Proximal tibiofibular joint (PTFJ) subluxations are rare and can occur following trauma or sporting events. Idiopathic PTFJ subluxations are more common in females and in patients with generalized ligament laxity. The proper history and clinical examination together with imaging can help in establishing the diagnosis in the majority of cases.
Case Report: We report a rare case of bilateral subluxation of PTFJ and describe the detailed clinical features and magnetic resonance imaging findings. The patient was managed conservatively with good results.
Conclusion: Bilateral subluxation of the PTFJ is a rare clinical entity often associated with specific demographic and physical characteristics, such as young females engaged in high-impact sports. This case underscores the importance of a thorough clinical and imaging evaluation to differentiate it from other causes of lateral knee pain and prominence. Conservative management, including physical therapy and routine follow-ups, has proven effective in managing symptoms and avoiding progression, highlighting the non-operative approach in treating this condition.
Keywords: Proximal tibiofibular joint, subluxation, instability, injury, conservative.
The proximal tibiofibular joint (PTFJ) is a synovial joint between a facet on the lateral tibial condyle and fibular head. Its main function is to dissipate the torsional stresses of the lower leg and lateral tibial bending moments. It also assists in the transmission of axial loads during weight-bearing [1, 2]. The PTFJ is an inherently stable joint, due to strong ligamentous support. A fibrous capsule surrounds the PTFJ articulation, and this is strengthened by anterosuperior and posterosuperior tibiofibular ligaments. The common peroneal nerve is in close proximity to this joint [3]. PTFJ subluxation is rarely reported. Most of the reported cases are due to trauma or after sports activities [4]. Two types of subluxations of PTFJ have been described: Idiopathic and post-dislocation. Idiopathic PTFJ subluxation is more common in young females and in patients with generalized ligament laxity or connective tissue disorders [4-7]. Ogden describes four types of instability or disruption of PTFJ. These were classified as subluxation, anterolateral dislocation, posteromedial dislocation, and superior dislocation [5]. Herein, we report a rare case of bilateral subluxation of PTFJ and describe the detailed clinical features and magnetic resonance imaging (MRI) findings.
A 14-year-old girl, a Karate and Judo player, presented with complaints of bilateral bony prominences on lateral aspects of her knees. When she and her mother first observed the prominences a year ago, she did not seek medical assistance immediately because, at the time, she had no restriction in the range of motion (ROM) of her knees and no pain. The patient then presented with complaints of mild pain in both knees at the site of bony prominence after sports activities. The pain was worse on the right knee than on the left side. She also has a concern regarding the cosmetic appearance due to prominences in both knees. Physical examination revealed no general ligamentous laxity with a Beighton score of 2/9. There was no tenderness at the bony prominences. The proximal fibula was prominent and felt displaced posterolaterally. There was a mild instability of both fibular heads on applying manual force anteroposteriorly. The fibular heads became more obvious on knee flexion and squatting. Her ROM was normal at both knees.
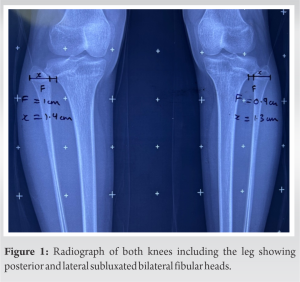
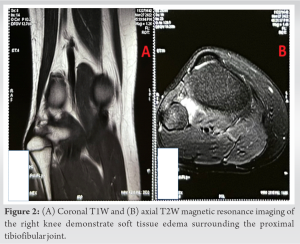
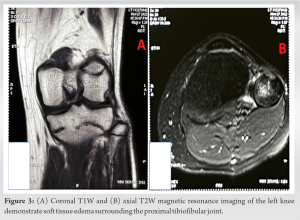
The radiograph of both knees including the leg showed posterior and lateral subluxated bilateral fibular heads (Fig. 1). The maximum width of the fibular head (F) was measured on an anteroposterior view as well as the distance from the lateral tibial border to the lateral cortex of the fibula (x) head along the same line as the maximum width of the fibular head. The ratio of x/F = Y was calculated, Y (right) = 1.40 and Y (left) = 1.44 (the normal value of Y is <1) (Fig. 1). The patient was advised for an MRI study to evaluate joint capsule and superior tibiofibular ligaments (Fig. 2 and 3). All the ligaments and joint capsule were found to be intact. Joint space was normal on both sides and no changes in cartilage were seen on either side. As no other abnormality was found and the patient was involved in sports activities, based on the clinical and radiological report, the patient was diagnosed with bilateral tibiofibular subluxation. The patient was managed conservatively and was advised hamstring stretching exercises and no other treatment was advised as the patient had no functional impairment. The patient was reassured and advised a follow-up with X-rays every 3 months to look for any progression in the degree of subluxation. At 1-year follow-up, the patient remained asymptomatic and showed no signs of progression of subluxation.
PTFJ subluxation cases are reported rarely and are usually associated with generalized ligamentous hyperlaxity and connective tissue disorders [5]. Generalized joint hypermobility in children falls under a spectrum and it is thought to be polygenic in origin with environmental influences, particularly participation in sports and flexibility training [8]. Idiopathic subluxation of the proximal end of the fibula is a self-limiting condition in children, with the symptoms decreasing in severity as the patient approaches skeletal maturity [5]. Bozkurt et al. have reported a case of bilateral congenital subluxation of the PTFJ in a 12 years old in an otherwise normal girl [9].
Extensive review of the literature has revealed no differentiating criteria between idiopathic PTFJ subluxation and traumatic dislocation but clinical, MRI, and radiographic evidence can help in diagnosing cases [9]. Clinical observations of bilaterality and instability in the anteroposterior plane, along with MRI results of intact fibular ligament and radiological findings of joint capsules, point to a PTFJ subluxation as of congenital origin [9]. Clinically, bilateral osteochondroma at the fibular heads or nearby can present similarly with fibular head prominences due to abnormal swelling or displacement of the fibular head by the swelling. The X-rays in these cases can easily confirm the diagnosis of osteochondromas. Chronic PTFJ instability due to trauma may cause lateral knee pain and instability with popping and catching which may be confused with a lateral meniscus injury. In acute PTFJ dislocation, there will be a history of direct trauma or sporting activity. There will be a history of trauma with a classic pattern of injury due to a slightly flexed knee and plantar flexed and rotated foot. There will be direct tenderness and more prominence of fibular head-on-knee flexion can give a clue to the diagnosis [6]. In the present case, only mild pain was the primary complaint and evaluated by radiographs and MRI which gives some clues for the differential diagnosis of subluxation of PTFJ. The radiographic findings of PTFJ subluxation include posterior displacement and lateral subluxation of the fibular heads [9]. Collateral ligament integrity, pathological signals in tendinous or ligamentous structures, assessment of articular cartilage size, narrowing of joint spaces, and subchondral erosions are all information that may be obtained on MRI [9]. In our case, the MRI finding was normal. Surgery is seldom necessary to treat PTFJ subluxation since it is a self-limiting problem. Subluxation symptoms can be managed non-surgically with activity modification, bracing, and knee strengthening exercises or surgically in situations of severe instability [10-12]. A symptomatic persistent subluxation or chronic recurrent dislocation necessitates open reduction and internal fixations using cortical fixation devices, screws, K wire, or an adjustable loop [13]. Patients experiencing severe pain and disability at PTFJ fusion or arthrodesis of the proximal tibiofibular joint may be considered [11,12,14]. As reported by Bozkurt et al. [9], we managed our patients conservatively.
Subluxation of PTFJ is rare and can occur in conjunction with ligament laxity. History of trauma or sports events must be ruled out in every case. The patients are usually asymptomatic and cosmesis may be the concern, especially in females. Radiographs and MRIs can help in diagnosis in the majority of cases. No treatment is usually required for asymptomatic cases.
In young athletes presenting with lateral knee pain and bony prominences, consider bilateral PTFJ subluxation, particularly in the absence of generalized ligament laxity, and pursue conservative management with imaging support for effective symptom control and functional preservation.
References
- 1.Bozkurt M, Yilmaz E, Atlihan D, Tekdemir I, Havitçioğlu H, Günal I. The proximal tibiofibular joint: An anatomic study. Clin Orthop Relat Res 2003;406:136-40. [Google Scholar]
- 2.Wang CT, Hing LT. Proximal tibiofibular joint: An overview. J Orthop Trauma Rehabil 2016;20:2-7. [Google Scholar]
- 3.Espregueira-Mendes JD, da Silva MV. Anatomy of the proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc 2006;14:241-9. [Google Scholar]
- 4.Andersen K. Dislocation of the superior tibiofibular joint. Injury 1985;16:494-8. [Google Scholar]
- 5.Ogden JA. Subluxation and dislocation of the proximal tibiofibular joint. JBJS. 1974;56:145-54. [Google Scholar]
- 6.Horan J, Quin G. Proximal tibiofibular dislocation. Emerg Med J 2006;23:e33. [Google Scholar]
- 7.Nieuwe Weme RA, Somford MP, Schepers T. Proximal tibiofibular dislocation: A case report and review of literature. Strategies Trauma Limb Reconstr 2014;9:185-9. [Google Scholar]
- 8.Remvig L, Jensen DV, Ward RC. Epidemiology of general joint hypermobility and basis for the proposed criteria for benign joint hypermobility syndrome: Review of the literature. J Rheumatol 2007;34:804-9. [Google Scholar]
- 9.Bozkurt M, Yilmaz E, Havitçioğlu H, Günal I. Bilateral congenital subluxation of the proximal tibiofibular joint with magnetic resonance imaging findings: A case report. Knee Surg Sports Traumatol Arthrosc 2002;10:340-2. [Google Scholar]
- 10.Miller TL, Curatolo C. Proximal tibiofibular joint instability: An underrecognized cause of lateral knee pain and mechanical symptoms. J Am Acad Orthop Surg 2023;31:e412-23. [Google Scholar]
- 11.Sekiya JK, Kuhn JE. Instability of the proximal tibiofibular joint. J Am Acad Orthop Surg 2003;11:120-8. [Google Scholar]
- 12.Kruckeberg BM, Cinque ME, Moatshe G, Marchetti D, DePhillipo NN, Chahla J, et al. Proximal tibiofibular joint instability and treatment approaches: A systematic review of the literature. Arthroscopy 2017;33:1743-51. [Google Scholar]
- 13.McNamara WJ, Matson AP, Mickelson DT, Moorman CT. Surgical management of proximal tibiofibular joint instability using an adjustable loop, cortical fixation device. Arthrosc Tech 2018;7:e271-7. [Google Scholar]
- 14.Sijbrandij S. Instability of the proximal tibio-fibular joint. Acta Orthop Scand 1978;49:621-6. [Google Scholar]