Fungal PJI presenting as late infections can mimic early aseptic loosening.
Dr. James C George, Department of Orthopaedic Surgery, Believers Church Medical College Hospital, Pathanamthitta-689 103, Kerala, India. E-mail: drjamescgeorge@gmail.com
Introduction: Fungal prosthetic joint infections (PJIs) are very rare in immunocompetent patients. PJI can present either early, delayed, or as late chronic infections. Diagnosis of fungal PJI presenting late is challenging due to the difficulty in isolation as well as the clinical presentation very similar to an aseptic loosening. There are no clear guidelines regarding the management of these patients.
Case series: We present five cases of Candida parapsilosis PJI presenting as late chronic infections. All five patients were culture-negative preoperatively, immunocompetent, and with good soft-tissue condition. There were three infected knee prostheses and two infected hip hemiarthroplasty. All of them were treated with extensive debridement, meticulous sampling, and extended culture. We treated all of them with long-term antifungals without any disease reactivation or recurrence till the last follow-up.
Conclusion: Fungal infection should be suspected in immunocompetent patients presenting early with features of aseptic loosening but without typical signs of periprosthetic infection. Revision with long-term suppressive therapy can give good results in these patients.
Keywords: Candida, paraspilosis, revision, hemiarthroplasty, fluconazole, culture-negative infection, knee arthroplasty.
Prosthetic joint infections (PJIs) are among the most common causes of revision surgeries in joint arthroplasty. Staphylococcus remains the most common organism isolated while fungal PJI accounts for nearly 1% of total PJI [1]. Among the various fungi that can produce PJI, Candida species is the most common [2,3]. PJI can present either early, delayed, or as late chronic infections. Any infections presenting after 12 months of the initial surgery are considered late presentation as it is usually due to a hematogenous spread or can be due to infection with low virulent organisms. Diagnosis of fungal PJI is very difficult due to the difficulty in isolation [4] as well as the clinical presentation very similar to an aseptic loosening. Only two studies with large cohorts are in the literature on fungal PJI [1,2]. All the remaining are case series and reports. Immunocompromised patients are particularly vulnerable to fungal PJI. Candida albicans and Candida parapsilosis are fungal pathogens frequently reported in the literature. There are no clear guidelines regarding the management of these patients. We present five more cases of C. parapsilosis late PJI in immune-competent patients treated with single-stage revision and fluconazole monotherapy.
Between 2018 and 2023, we had eight female patients and one male patient with fungal PJI. Among them, seven female patients had infected knee arthroplasty whereas the remaining two patients had infected hemiarthroplasty. Among the knee arthroplasty patients, one patient who presented 17 months after surgery did not come for treatment after diagnosis, and yet another patient who presented after a revision knee surgery for loosening at 12 months decided not to go ahead with any further intervention. Both patients isolated C. parapsilosis sensitive to fluconazole. Excluding these two patients, we had seven cases. Among them, two patients with knee arthroplasty who presented with loosening and discharging sinus grew C. albicans and underwent two-stage revision and arthrodesis. Both these patients were immunocompromised. Finally, we treated five immuno-competent patients with late chronic infection with loosening. Informed consent and institutional review board approval were obtained before the evaluation of these patients. Pre-operative synovial fluid analysis was done for all five patients. Ultrasound-guided aspiration was done for hemiarthroplasty patients. Synovial fluid and five tissue samples were done intraoperatively for all patients. The fluid culture was done with an automated blood culture system (Bact/ALERT, bioMerieux, Marcy-l’Étoile, France) and tissue culture was done by mounting on Sabouraud dextrose agar (SDA). Clinical isolates of Candida species obtained from Bact/AlERT were subcultured on SDA after identifying Gram-positive budding yeast on Gram stain of positive culture broth. The suspected colonies of Candida were confirmed through Gram stain and Germ tube test and then were identified with Vitek 2 Compact using Vitek ID-YST cards. Anti-fungal susceptibility testing was performed with Vitek AST-YS08 cards. Five samples were taken for culture from every patient. Positive cultures from at least two samples were required for consideration PJI. When the culture came positive for C. parapsilosis, all patients received 2 weeks of IV fluconazole followed by oral fluconazole 200 mg twice daily for 3 months. A liver function test was done routinely for all patients every 1 month and none of them developed any derangement. We had two patients with hip pain and three patients with knee pain after hemiarthroplasty and total knee arthroplasty, respectively. None of these patients had any fever or any constitutional symptoms to suspect infection. Except for an elevated erythrocyte sedimentation rate (ESR), all of them had a normal blood picture (Table 1). Pre-operative synovial fluid analysis did not grow any microorganisms in any patients. Intraoperative tissue and fluid cultures of all five patients grew C. parapsilosis and was given antifungal therapy with fluconazole for 3 months. None of them developed reactivation till the last follow-up (Tables 2-4).

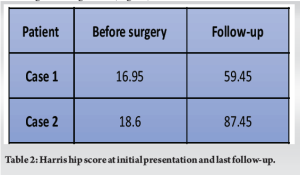

Case 1 was a 79-year-old man, with type 2 diabetes mellitus, benign prostatic hyperplasia, and coronary artery disease with progressive hip pain becoming worse for 3 months. He had undergone an uncemented bipolar hemiarthroplasty 14 months ago. His radiograph showed a subluxated hip prosthesis with a well-integrated uncemented femoral stem (Fig. 1a). The femoral stem was extracted with an extended trochanteric osteotomy. Revision surgery was performed with DePuy Pinnacle Acetabulum and Solution stem after meticulous debridement. The patient was followed up for 2.5 years without any reactivation (Fig. 1b). At the last follow-up, his Harris Hip score was 59.45 (Table 2). He developed a cerebrovascular accident (major stroke) and passed away due to reasons unrelated to the revision surgery.
Case 2 was a 70-year-old lady with right hip pain for 4 months after an uncemented bipolar hemiarthroplasty done for a neck of femur fracture 18 months back. X-ray showed grade 3 protrusio hip (Fig. 2a). The femoral stem was well fixed without any loosening. The stem was retained and acetabular protrusio was filled with allograft and the cup was revised with a Depuy Pinnacle cup. Her Harris Hip score improved to 87.45 at the 3 years at follow-up without any reactivation (Table 2). X-ray showed good integration (Fig. 2b).
Case 3 was a 65-year-old diabetic lady who presented to us 25 months after left knee arthroplasty surgery, pain effusion reduced flexion range (90°) for the last 6 months. Knee radiographs showed tibial loosening in all zones as per Knee Society guidelines and in 1–4 zones of the femur (Fig. 3a and b). After thorough debridement, she underwent a revision knee arthroplasty using bone cement incorporated with gentamycin and vancomycin. Her post-operative knee society scores at 4.5-year follow-up are shown in Table 3.
Case 4 was a 64-year-old lady without any medical comorbidities presented with an 18-month history of knee effusion and painful knee flexion to 70°. Her knee arthroplasty was done 3 years back (Fig. 3c). She underwent revision knee surgery with azithromycin-loaded bone cement. Her knee society score improved (Table 3) and the radiograph did not show any loosening at the 4-year follow-up (Fig. 3d). Case 5 was a 60-year-old lady presented 21 months after knee arthroplasty with recurrent effusion and pain. The radiology was normal with well-fixed implants. The lower end of the incision scar was tender and erythematous. Her aspirate did not grow any microorganisms. Her pain and effusion were not reduced after anti-inflammatory medicines and empirical antibiotics for 10 days. Her joint was aspirated again and cultured which grew C. parapsilosis at 7 days. She underwent debridement and implant retention. Intraoperative tissue cultures were also positive for Candida. At the final follow-up of 18 months, she had no loosening or recurrence of infection.
Fungal PJI is rare and the limited literature available makes it difficult to adopt a planned approach to its management. Since fungal PJI most commonly is associated with the immunocompromised state, a healthy patient with a loosened implant without any signs of sepsis can get labeled as aseptic loosening [5]. However, post-operatively, it may turn out to be culture-positive after extended culture and meticulous tissue sampling. This unexpected positive culture (UPC) is not very uncommon in literature. Neufeld had encouraging results with a prevalence of 9.2% (110) of 1196 aseptic THA revisions with a 2- and 5-year infection-free implant survival of 93.1% and 86.8%, respectively [6]. Another article with fewer patients where pre-operative cultures after aspiration were negative showed a prevalence of 44% (7 out of 16) of UPC among hemiarthroplasty patients [5]. All patients had an elevated ESR similar to that observed in our patients. To date, there is no fungal UPC published in the literature. Our study must be the first fungal UPC published so far. Diagnosis of fungus is also quite challenging. All our patients except for a rise in ESR appeared as aseptic loosening or rather culture-negative infections. Parvizi et al. have outlined new evidence-based and validated criteria for the diagnosis of PJI preoperatively and intraoperatively [7]. Our patients did not fit into the pre-operative criteria but did have two intraoperative cultures positive for the same C. parapsilosis after extended culture in BACTALERT and Sabouraud dextrose agar. Even though C. albicans is the most common fungal PJI, Klatte found that all of his fungal PJI of the knee were infected with C. parapsilosis [8]. Azzam et al. [3] in their meta-analysis also identified C. parapsilosis as the most common organism, representing 39% of infections [2]. Hwang et al. detected C. parapsilosis in 50% of their 30 fungal PJI. Our series with culture-negative low-grade PJI presenting late also showed C. parapsilosis as the most common pathogen. Bacterial PJI can be treated with two-stage or single-stage exchange arthroplasty. Two meta-analyses have shown that one-stage exchange arthroplasty may provide superior outcomes, including lower reinfection rates and superior function, in a selected group of patients (absence of severe immunocompromised state and significant soft-tissue or bony compromise and concurrent acute sepsis) [9]. The rate of recurrent infection ranged from 0% to 18%, at a minimum of 2-year follow-up [9]. For fungal PJIs, most authors recommend a two-stage revision. The rates of recurrent infection vary widely and may be up to 25% [3], especially in patients with discharging sinus and immunocompromised states. The patients reported here were not immunocompromised and had a near-normal soft-tissue envelope. The five patients in our series with single-stage revision surgery did not develop any reinfection till the last follow-up. Apart from the prophylactic antibiotics, most culture-negative patients receive antibiotics till the definitive culture reports arrive. Fugal cultures take 7–10 days to be ready and therefore the definitive antifungal treatment will be delayed for 1 week. Oral fluconazole has a high bioavailability equivalent to amphotericin. Oral fluconazole is less toxic and has shown good synovial fluid and serum concentrations comparable to amphotericin while treating Candida infections [10, 11]. The Infectious Diseases Society of America recommends giving antifungals for 6–12 months for osteomyelitis and 6 weeks for septic arthritis. We gave intravenous fluconazole (200 mg twice daily) for 2 weeks and oral fluconazole for 3 months. All the patients had normal CRP preoperatively. Postoperatively the CRP elevated and normalized by 6 weeks. There was no loosening or reactivation of infection during the follow-up.
All immunocompetent patients presenting with an early prosthetic loosening should be evaluated for fungal elements if the culture is negative. C. parapsilosis is a common fungal PJI, especially in knee joints. Single-stage revision and fluconazole monotherapy have prevented the reactivation and recurrence of C. parapsilosis in immunocompetent patients with good soft tissues in our series.
Meticulous debridement of all revision surgeries is required in an immunocompetent patient with suspected aseptic loosening considering emerging positive fungal cultures. Send samples for extended cultures and fungal cultures for all prosthetic loosening presenting early irrespective of normal-appearing blood picture.
References
- 1.Theil C, Schmidt-Braekling T, Gosheger G, Idelevich EA, Moellenbeck B, Dieckmann R. Fungal prosthetic joint infection in total hip or knee arthroplasty: A retrospective single-centre study of 26 cases. Bone Joint J 2019;101:589-95. [Google Scholar]
- 2.Hwang BH, Yoon JY, Nam CH, Jung KA, Lee SC, Han CD, et al. Fungal peri-prosthetic joint infection after primary total knee replacement. J Bone Joint Surg Br 2012;94:656-9. [Google Scholar]
- 3.Azzam K, Parvizi J, Jungkind D, Hanssen A, Fehring T, Springer B, et al. Microbiological, clinical, and surgical features of fungal prosthetic joint infections: A multi-institutional experience. J Bone Joint Surg Am 2009;91 Suppl S6:142-9. [Google Scholar]
- 4.Basu S, Bose C, Ojha N, Das N, Das J, Pal M, Khurana S. Evolution of bacterial and fungal growth media. Bioinformation 2015;11:182-4. [Google Scholar]
- 5.Neufeld ME, Lanting BA, Shehata M, Howard JL, MacDonald SJ, Teeter MG, et al. Prevalence and outcomes of unexpected positive intraoperative cultures in presumed aseptic revision hip arthroplasty. J Bone Joint Surg Am 2021;103:1392-401. [Google Scholar]
- 6.Cichos KH, Detweiler M, Parvizi J, McGwin G Jr., Heatherly AR, Ghanem ES. The fate of positive intraoperative cultures following conversion total hip arthroplasty. Hip Int 2022;32:17-24. [Google Scholar]
- 7.Parvizi J, Tan TL, Goswami K, Higuera C, Della Valle C, Chen AF, et al. The 2018 definition of periprosthetic hip and knee infection: An evidence-based and validated criteria. J Arthroplasty 2018;33:1309-14.e2. [Google Scholar]
- 8.Klatte TO, Kendoff D, Kamath AF, Jonen V, Rueger JM, Frommelt L, et al. Single-stage revision for fungal peri-prosthetic joint infection: A single-centre experience. Bone Joint J 2014;96:492-6. [Google Scholar]
- 9.Thakrar RR, Horriat S, Kayani B, Haddad FS. Indications for a single-stage exchange arthroplasty for chronic prosthetic joint infection: A systematic review. Bone Joint J 2019;101-B 1 Suppl A:19-24. [Google Scholar]
- 10.Rex JH, Bennett JE, Sugar AM, Pappas PG, Van der Horst CM, Edwards JE, et al. A randomized trial comparing fluconazole with amphotericin B for treatment of candidemia in patients without neutropenia. Candidemia study group and the national institute. N Engl J Med 1994;331:1325. [Google Scholar]
- 11.Brammer KW, Farrow PR, Faulkner JK. Pharmacokinetics and tissue penetration of fluconazole in humans. Rev Infect Dis 1990;12 Suppl 3:318-26. [Google Scholar]













