Polyethylene liner wear is a common cause for aseptic loosening in hemi and total hip arthroplasties and awareness regarding its diagnosis and management is essential with increasing numbers of hip replacements surgeries
Dr. Dhruva Angachekar, Department of Orthopaedics, Gleneagles Hospital, Mumbai, Maharashtra, India. E-mail: drdhruva55@gmail.com
Introduction: Aseptic component loosening is a common cause of revision surgery post a hip replacement surgery. Polyethylene wear is a known cause of this loosening which results due to osteolysis of the bone stock surrounding the implant. Most patients have catastrophic wear through failure which manifests as discomfort, noise in the joint, and eccentric femoral head location with increasing leg length discrepancy. However, sometimes clinical presentation may be quite late while liner erosion leads to subluxation of the femoral head which is seen on radiographic imaging. We present a case of rapid polyethylene liner wear leading to femoral head subluxation in a case of bipolar hemiarthroplasty of the hip.
Case Report: A 70-year-old female patient underwent a bipolar hemiarthroplasty of the right hip for a transcervical neck of femur fracture 5 years ago. She presented to us with a subluxated femoral head within the cup on radiographs with clinical limp and pain. She was taken up for revision total hip replacement surgery.
Conclusion:Routine clinical and radiographic follow-ups should be done post-total or hemi hip replacement surgeries to catch polyethylene wear signs and symptoms in the early stage which could then be treated with a simple liner exchange rather than an extensive revision surgery. Whenever dealing with osteoporotic bone, we need to keep a low threshold for extended trochanteric osteotomy for cement removal from the femoral canal.
Keywords: Hip arthroplasty, revision surgery, polyethylene liner wear, extended trochanteric osteotomy.
Polyethylene liner wear leading to failure of primary hip replacement surgeries is a well-known complication [1]. The wear debris stimulates an immune response during which the particles are phagocytosed by the macrophages and a cycle of direct and indirect osteolysis is set up which leads to subsequent component loosening [2]. Attempts have been made over the years to reduce the amount of polyethylene particles generated due to wear, with efforts directed at investigating substitute-bearing surfaces and enhancing wear by raising polyethylene crosslinking and reducing polyethylene oxidation [3]. A meta-analysis comparing the wear rates of polyethylene liners between ceramic and metal femoral heads used in total hip replacements showed no significant difference in the wear rates between ceramic on poly and metal on poly articulations [4]. Some of the factors which affect liner wear include foreign body debris, reduced thickness of the polyethylene liner, non-articular backside wear, increased activity of the patient, amount of crosslinking in the polymer, removal of oxidation, the processing and sterilizing method used for the polyethylene, femoral head size and component malposition [5]. Catastrophic wear through failure manifests as discomfort, noise in the joint, and with an eccentric femoral head position with a growing disparity in leg length [6]. Nonetheless, the majority of patients exhibiting severe wear manifest during standard follow-up appointments and qualify for a revision complete hip replacement [7]. We present a case of a 70-year-old female who underwent a bipolar hemi replacement of the hip 5 years ago and now presented to us with advanced liner wear and was taken up for revision total hip arthroplasty.
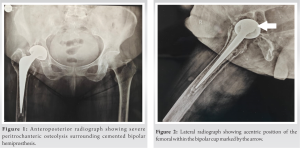
A 70-year-old female visited our outpatient department with complaints of right hip pain and an antalgic gait. She gave a history of undergoing a bipolar hemi replacement of the right hip for a transcervical neck of femur fracture 5 years ago. She had also undergone a bilateral total knee replacement 9 years ago. Her radiographs showed (Fig. 1 and 2) severe osteolysis around the stem in the trochanteric region with subluxation of the head within the liner cup. We decided to go for a revision total hip arthroplasty after assessing her general health condition.
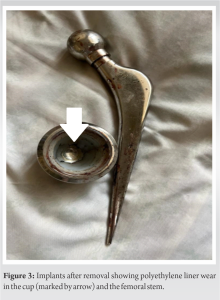
The surgery was done in a lateral decubitus position with a modified Hardinge approach. On reaching the capsule, there was severe scarring along with blackish staining of the tissues due to metallosis. The implant was dislocated and while trying to dislodge the femoral head, the entire stem came out along with it. On inspecting the cup, we saw a complete erosion of the polyethylene liner in the posterosuperior region (Fig. 3). The implants were of an unknown company with the femoral head measured to be of size 44 mm.
Initial attempts at removing the bone cements were unsuccessful so considering the osteoporotic nature of her bone; we performed an extended trochanteric osteotomy (ETO) for ease of cement removal. Acetabular reaming was done and a 46 mm Continuum multihole acetabular cup was fixed after checking alignment and version with three acetabular locking screws and a 10° polyethylene liner over it (Zimmer Biomet, Warsaw, Indiana, USA). Femoral reaming was done and a Wagner diaphyseal long stem was used with a 32 mm metal minus three femoral head (Zimmer Biomet, Warsaw, Indiana, USA). The ETO was fixed by passing four stainless steel cerclage wires at different levels (Fig. 4). Stability was checked and closure was done. The patient was mobilized after 24 h with pain control by multi-modal analgesia.
Following a primary total or hemi hip arthroplasty, 0.95–5.71% of patients require revision surgery [8]. Aseptic loosening was found to be a major cause (55%) of revision hip replacements in complication analysis of world arthroplasty registers [9]. Osteolysis mostly results from an immunologic reaction to particulate debris, which in turn causes gradual bone loss and implant loosening. Although osteolysis is not always the result of wear debris, it is more likely to happen when the rate of wear particles produced surpasses the ability of the individual to eliminate the debris; this usually happens when wear rates are ≥0.1 mm/y [2]. Of 128 hips, Min et al. found that 14 (10.9%) had metallosis and polyethylene wear through. The authors explained this high rate by pointing out that “non-Western” populations have eccentric leg motions [6]. A similar case was reported by Needham et al. where the patient presented with a 3rd time atraumatic hip dislocation. On taking up the patient for revision surgery failure of the acetabular components was noted, with total wear through of the titanium shell and polyethylene lining. The femoral head made of alumina ceramic was undamaged, albeit it had some surface wear and dark metallic discoloration [7]. Similar to these cases, our case also had severe capsular thickening and black staining of tissues due to metallosis. Our case also showed a severe polyethylene line wear and mild erosion of the metal outer head. Manzano et al. in his case report of polyethylene liner failure in total hip arthroplasties bilaterally noted that the femoral head appeared eccentric on radiographs and the patient presented to them with a limp and severe hip pain. Similar radiographic findings and complaints were noted in our case. They carried out staged bilateral revision hip replacements using similar acetabular cups, polyethylene liners, and femoral stems as have been used in our case. The patient had a good clinical result postoperatively [10]. Given the substandard nature of the primary implant and cost constraints, the liner must have been of non-cross-linked polyethylene which would explain the accelerated wear. Non-cross-linked polyethylene liners are known to have higher wear rates as compared to highly cross-linked polyethylene liners. In a prospective randomized control trial, Engh et al. compared the 10-year results of polyethylene liners that were crosslinked and non-crosslinked. They found that during a 10-year period, 94.7% of non-cross-linked polyethylene and 100% of cross-linked polyethylene survivorship occurred. Osteolysis risk has been linked to a polyethylene wear rate of >0.1 mm/year [11]. Cement removal from the femoral canal is very difficult when there is little bone stock due to severe osteolysis. Penetration of the cortex and disturbing cortical continuity is very likely in such situations. We suggest having a low threshold for performing an ETO in such cases to reduce surgical time as well and preventing possible complications. Miner et al. in his critical review of ETO in revision arthroplasties reviewed 166 cases of ETO and concluded that effective and secure extraction of cement-free or cement-bonded stems is made possible by ETO, which heals steadily and produces outstanding outcomes in terms of revision stem ingrowth [12]. Nineteen hips had received a revision total hip arthroplasty due to mechanical failure and 3 were awaiting revision, according to Pellegrini et al.’s study on the 104 hips that were reachable for clinical and radiological follow-up at a mean post-operative follow-up of 12.2 years. In their study, the total percentage of mechanical failure was 21.2%. They found that when bipolar hemiarthroplasty is used to treat hip arthritis, there is a significant risk of migration, osteolysis discomfort, and ultimately revision total hip replacement [13]. From this case, we want to highlight that bipolar hemiprosthesis has a poor long-term survival rate and is best avoided in young patients. According to an American Association of Hip and Knee Surgeons survey, the majority of surgeons advise either an annual or biennial follow-up following total hip arthroplasty [14]. Frequent monitoring identifies impending component failure and may lessen morbidity related to catastrophic failure and the subsequent revision. Highlights of the 2023 American Joint Replacement Registry annual report show that hemiarthroplasty remains the most performed procedure from neck of femur fractures. There is an increase of cement use in primary hip replacements for femoral component fixation. They noted an increase in the use of ceramic on polyethylene articulations (72.56%) as well as highly cross-linked polyethylene (95.88%) [15]. These recent statistics highlight the importance of this clinical case report.
Polyethylene liner wear resulting in the need for a revision hip replacement is a complication which should be kept in mind. It is best to avoid the use of non-cross-linked polyethylene and bipolar hemiprosthesis in young patients as they have high failure rates in the long term. We should keep a low threshold for performing ETO in revision surgeries with severe osteolysis and poor bone stock.
Polyethylene liner wear is a complication which should be anticipated if non-cross-linked polyethylene liner or a bipolar hemiprosthesis is used for the treatment of hip pathologies in younger patient group. Regular annual clinical and radiographic evaluations are recommended to screen for this complication as it may be asymptomatic for a long time and finally resulting in a catastrophic failure.
References
- 1.Learmonth ID, Young C, Rorabeck C. The operation of the century: Total hip replacement. Lancet 2007;370:1508-19. [Google Scholar]
- 2.Kurcz B, Lyons J, Sayeed Z, Anoushiravani AA, Iorio R. Osteolysis as it pertains to total hip arthroplasty. Orthop Clin North Am 2018;49:419-35. [Google Scholar]
- 3.Urban JA, Garvin KL, Boese CK, Bryson L, Pedersen DR, Callaghan JJ, et al. Ceramic-on-polyethylene bearing surfaces in total hip arthroplasty. Seventeen to twenty-one-year results. J Bone Joint Surg Am 2001;83:1688-94. [Google Scholar]
- 4.Gosling OB, Ferreri TG, Khoshbin A, Whitehouse MR, Atrey A. A systematic review and meta-analysis of survivorship and wear rates of metal and ceramic heads articulating with polyethylene liners in total hip arthroplasty. Hip Int 2020;30:761-74. [Google Scholar]
- 5.Ries MD. Complications in primary total hip arthroplasty: Avoidance and management: Wear. Instr Course Lect 2003;52:257-65. [Google Scholar]
- 6.Min BW, Song KS, Kang CH, Won YY, Koo KH. Polyethylene liner failure in second-generation Harris-Galante acetabular components. J Arthroplasty 2005;20:717-22. [Google Scholar]
- 7.Needham J, Burns T, Gerlinger T. Catastrophic failure of ceramic-polyethylene bearing total hip arthroplasty. J Arthroplasty 2008;23:627-30. [Google Scholar]
- 8.Badarudeen S, Shu AC, Ong KL, Baykal D, Lau E, Malkani AL. Complications after revision total hip arthroplasty in the medicare population. J Arthroplasty 2017;32:1954-8. [Google Scholar]
- 9.Sadoghi P, Liebensteiner M, Agreiter M, Leithner A, Böhler N, Labek G. Revision surgery after total joint arthroplasty: A complication-based analysis using worldwide arthroplasty registers. J Arthroplasty 2013;28:1329-32. [Google Scholar]
- 10.Manzano G, Levin RA, Mayor MB, Schwarzkopf R. Catastrophic failure of the acetabular polyethylene liner in ceramic-on-polyethylene total hip arthroplasty. J Orthop Case Rep 2014;4:51-6. [Google Scholar]
- 11.Engh CA Jr., Stepniewski AS, Ginn SD, Beykirch SE, Sychterz-Terefenko CJ, Hopper RH Jr., et al. A randomized prospective evaluation of outcomes after total hip arthroplasty using cross-linked marathon and non-cross-linked Enduron polyethylene liners. J Arthroplasty 2006;21:17-25. [Google Scholar]
- 12.Miner TM, Momberger NG, Chong D, Paprosky WL. The extended trochanteric osteotomy in revision hip arthroplasty: A critical review of 166 cases at mean 3-year, 9-month follow-up. J Arthroplasty 2001;16:188-94. [Google Scholar]
- 13.Pellegrini VD Jr., Heiges BA, Bixler B, Lehman EB, Davis CM 3rd. Minimum ten-year results of primary bipolar hip arthroplasty for degenerative arthritis of the hip. J Bone Joint Surg Am 2006;88:1817-25. [Google Scholar]
- 14.Teeny SM, York SC, Mesko JW, Rea RE. Long-term follow-up care recommendations after total hip and knee arthroplasty: Results of the American Association of Hip and Knee Surgeons’ member survey. J Arthroplasty 2003;18:954-62. [Google Scholar]
- 15.Ryan SP, Stambough JB, Huddleston JI, Levine BR. Highlights of the 2023 American joint replacement registry annual report. Arthroplast Today 2024;26:101325. [Google Scholar]