The goal of this paper is to illustrate an approach to shoulder pain and to remind clinicians of the rarer entities that may mimic that of rotator cuff pathology as well as to consider red flag differentials in the process of making an eventual diagnosis for the patient.
Dr. Amirzeb Aurangzeb, Department of Orthopaedic Surgery, Changi General Hospital, Singapore. E-mail: amirzeb19@yahoo.com.sg
Introduction: Acute shoulder pain is among the most common presenting complaints in the clinic. Clinicians may find it challenging with the myriad of potential etiologies to explain for the presenting complaint. We present a unique case, where a herpes zoster infection in the C6 dermatome mimicked the presentation of rotator cuff pathology and was admitted to the care of orthopedics. We have also included a detailed literature review on the topic in our study.
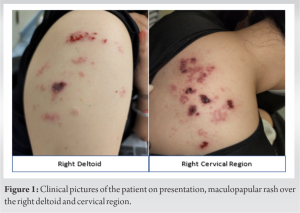
Case Report: The patient was a 38-year-old Chinese female who presented with acute atraumatic right-sided shoulder pain and weakness which was potentially confounded by an attempt of traditional Chinese medicine. Clinical examination revealed that the range of motion was globally reduced and painful in all directions with equivocal impingement testing. Examination of the skin revealed the presence of polymorphous eruption of erythematous papules and vesicles in the right shoulder and C6 region. In this paper, we discuss a possible algorithm to aid clinicians in an acute shoulder pain history with accompanying red flags to look out for. This is accompanied by a detailed literature review on the topic which demonstrates the rarity of this presentation which eventually confounded the initial management of the patient.
Conclusion: A thorough history and physical examination must remain the cornerstone of a clinician’s diagnostic algorithm. Zoster neuropathy at the level of the cervical spine is a rare entity. This case report also emphasizes the need for cognizance of local traditional remedies practiced and their interactions with clinical diagnosis and treatment.
Keywords: Shoulder, zoster, cervical.
Varicella otherwise commonly known as chickenpox disease is a contagious viral illnesses caused by the varicella-zoster virus. Primary varicella infections usually tend to present as a vesicular pruritic rash occurring over the trunk, head, and face. Herpes zoster is classically associated with a localized, painful, and blistering rash that follows a unilateral dermatomal distribution that does not cross the midline [1]. Herpes zoster is most commonly in the thoracic region, followed by the lumbar, cervical, and then sacral region [2,3]. Symptoms tend to be more severe for adults than for children [4]. Herpes zoster disease, or shingles, occurs when the dormant varicella-zoster virus reactivates within the dorsal root ganglia or cranial nerve [5]. Herpes zoster disease is normally managed within a primary care setting, through patient education, contact precaution, and appropriate analgesia. However, when herpes zoster affects less common dermatomes, its manifestation may be atypical and pose a diagnostic conundrum. We present a rare case of a herpes zoster infection in the C6 dermatome closely mimicking that of rotator cuff pathology. The goal of the paper is to illustrate an approach to shoulder pain and to remind clinicians of the rarer entities that may mimic that of rotator cuff pathology as well as to consider red flag differentials in the process of making an eventual diagnosis for the patient.
The patient was a 38-year-old Chinese female with a history uncomplicated childhood varicella disease. She presented to the emergency department with a 7-day history of atraumatic right-sided shoulder pain and weakness. Her symptoms developed acutely and she had significant rest pain and night pain. Symptoms were significant enough to affect her quality of sleep and function including the donning and removing of clothes. The patient had no prior history of fever, myalgia, or malaise. The patient did not complain of stiffness or numbness in the affected upper limb. There was no previous surgery performed on the right shoulder and she did not suffer from any chronic metabolic diseases. Nil red flags were picked up during history taking as well (Fig. 1). Significantly, the patient’s husband attempted acupuncture and a traditional Chinese massage technique known as “gua sha” which involves rubbing down affected areas with sand or a mild excoriating substance. These measures were attempted on the right shoulder without symptomatic relief. It was only after a week of severe discomfort that she presented to the emergency department seeking medical treatment. Clinical examination revealed that her right shoulder range of motion was globally reduced and painful in all directions. There was no significant effusion. Impingement testing was not performed as the patient was in significant pain on movement of the shoulder despite analgesics. Rotator cuff strength testing revealed weakness in supraspinatus, infraspinatus, and subscapularis muscles. Closer inspection revealed a polymorphous eruption of erythematous papules and vesicles with some crusting over the C6 dermatome, extending to the right lateral arm and upper trapezius. This rash was not described to be itchy or painful and was claimed to have been brought about by acupuncture and massage performed by the patient’s husband. It was unclear if the rash originally started before or after the acupuncture efforts from history taking. The initial impression was that of right shoulder rotator cuff impingement syndrome by the Emergency Department physician, with the skin lesions attributed to the excoriating massage by both the patient and the physician. The patient was promptly admitted under the care of orthopedic department.
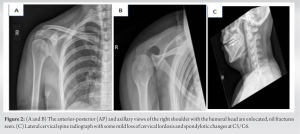
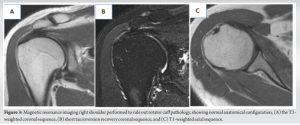
Biochemical evaluation was unremarkable with flat inflammatory markers of total white cell count of 5.7 × 103/UL and C-reactive protein of 2.3 mg/L. Radiographs of the right shoulder and cervical spine were performed, showing no acute fracture or bony injury and preserved subacromial space with congruence of the right glenohumeral and acromioclavicular joints and straightening of the normal cervical lordosis with mild spondylotic changes at the C5/C6 level (Fig. 2). In view of patient’s symptom severity and persistent reduction in right shoulder movement, a magnetic resonance imaging (MRI) of the shoulder was performed (Fig. 3). MRI of the right shoulder was unremarkable and did not demonstrate any shoulder synovitis, effusion, rotator cuff tendonitis, tears, or any significant bony pathology. Dermatologist was referred and polymerase chain reaction swab was performed on the vesicular rash which turned out positive for varicella zoster viral DNA.
On discovering these findings, patient’s analgesia was titrated and optimized, a 7-day course of oral acyclovir was prescribed under the advice of a dermatologist, and she was discharged to primary care for the continued care of the zoster.
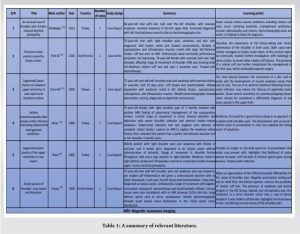
This case is particularly unique as classic cutaneous herpes zoster infection does not classically affect the cervical region. This confounded the management plans for the patient as it was thought to be that of rotator cuff pathology in nature and thus admitted to the care of the orthopedic department. Varicella-zoster viral infection usually results in symptoms of a vesicular itchy and painful rash, malaise as well as fever [6]. However, symptoms may be worser in adults compared to children. The mechanism of how zoster results in paresis is unclear but assumed to be due to the spread of the virus along the nerves with underlying inflammation [7,8]. This may thus explain the weakness that the patient reported on examination. Zoster is usually managed as self-limiting condition with analgesia but anti-virals such as acyclovir can also be used as adjuncts in management [9]. The main pearls of diagnosis come from good clinical history and physical examination. Clinical history should include asking the patient the site, onset, character of pain, radiation of pain, alleviating factors, time of symptoms, exacerbating factors, and pain score. Important considerations to take note would also be the hand dominance, occupation, presence of any trauma or precipitating injury, previous shoulder or spine surgeries, as well as the presence of any other pain or stiffness in other joints to exclude polyarticular disease [6]. In the presence of trauma or injury, additional details on the mechanism and force of injury are crucial as well. Red flags include symptoms such as fever, weight loss, night sweats, respiratory symptoms, and trauma [10]. The patient needs to be adequately exposed for a proper and complete physical examination. Examination of the skin includes looking for rash, masses or swellings, and localized erythema [10]. Assessment includes patient’s active and passive range of movement. Special attention should be given to the muscle strength of the rotator cuffs during each movement. The rotator cuffs should also be evaluated through a series of special tests that evaluate the movement of the glenohumeral joint in the anterior, posterior, and lateral directions. Special attention should be paid to the muscle strength of the rotator cuffs during each movement. Belly lift-off test is commonly done to evaluate the strength of the subscapularis, while Jobe’s and external rotation lag sign evaluates the supraspinatus and infraspinatus. Hornblower’s sign is used to determine teres minor and infraspinatus insufficiency. These tests are further supported by Hawkin’s and Neer’s tests for impingement testing as well as anterior apprehension test for shoulder instability. Patients with diffuse tenderness or global reduction in range of movement in the shoulder tend to be associated with capsulitis or frozen shoulder. Symptoms associated with exquisite tenderness and fever raise the suspicion of septic arthritis. When the pain or stiffness is more gradual in onset, we consider the possibility of glenohumeral osteoarthritis as a differential. Pain at rest or associated weakness in the rotator cuffs increases the likelihood of rotator cuff tears or tendinopathy. When patients report associated symptoms of numbness, paraesthesia, or shooting electric pain down the upper limbs, clinicians should also consider a cervical spine origin. Rotator cuff impingement syndrome is a clinical diagnosis. In this case, since the biochemical markers, X-rays and MRI imaging were not suggestive of an active subacromial or glenohumeral pathology to explain the patient’s symptoms; her symptoms were attributed to the ongoing herpes zoster infection. We performed a detailed literature search on the PubMed database to review other articles of a similar nature. The search interval was set up until 1st January 2024. The search was done using the keywords in English: “herpes zoster shoulder” and “cervical zoster shoulder.” Shortlisted papers were reviewed for their relevance to the subject, namely, on the presence of cervical zoster symptoms with correlation to shoulder pain in the patient. Any studies dated before January 2000 were excluded from the study. A total of 69 articles were identified for initial screening. After duplicate records and records not available in English were removed, 49 records underwent a title screening process. Thirty-four records were excluded based on a title screening process as they were not relevant to the topic discussed. The remainder of the 15 records underwent an abstract screening process and a further nine records were removed due to irrelevance to the topic. The remainder of the six studies is summarized in Table 1.
Table 1 demonstrates the current literature around the topic discussed. We have included a summary of the article as well as pertinent learning outcomes from each article in the table. As seen from the table, most of the existing relevant literature to the report consists of isolated case reports or short case series with a considerable lack of empirical studies or systematic reviews. In the absence of empirical data, case reports or series are the main resource for clinicians with their ability to provide an accurate description of patient experience, clinical manifestations, diagnostic challenges faced, and treatment outcomes with important pearls of knowledge for future decision-making. Within the context of the limited literature that surrounds the topic as such, our case report adds to the repertoire of knowledge and brings about valuable insights into an effective clinical examination of the shoulder.
A thorough history and physical examination must remain the cornerstone of a clinician’s diagnostic algorithm. Zoster neuropathy at the level of the cervical spine is a rare entity whose manifestation can outfox even the most experienced clinicians. Shoulder pain disproportionate to the history with cutaneous signs should always prompt the consideration of a herpes zoster infection. This case report also emphasizes the need for cognizance of local traditional remedies practiced and their interactions with clinical diagnosis and treatment.
This case study clearly underlines the need for a proper diagnostic approach to a patient presenting with shoulder pain. The need for accurate triage, history-taking, and physical examination could have reduced the chances of an initial misdiagnosis and management of the patient under a different discipline.
References
- 1.Sampathkumar P, Drage LA, Martin DP. Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc 2009;84:274-80. [Google Scholar]
- 2.Dayan RR, Peleg R. Herpes zoster-typical and atypical presentations. Postgrad Med 2017;129:567-71. [Google Scholar]
- 3.Koshy E, Mengting L, Kumar H, Jianbo W. Epidemiology, treatment and prevention of herpes zoster: A comprehensive review. Indian J Dermatol Venereol Leprol 2018;84:251-62. [Google Scholar]
- 4.Ayoade F, Kumar S. Varicella-Zoster. Treasure Island, FL: StatPearls Publishing; 2022. [Google Scholar]
- 5.Nair PA, Patel BC. Herpes Zoster. Treasure Island, FL: StatPearls Publishing; 2022. [Google Scholar]
- 6.Yang S, Kim TU, Kim DH, Chang MC. Understanding the physical examination of the shoulder: A narrative review. Ann Palliat Med 2021;10:2293-303. [Google Scholar]
- 7.Liu Y, Wu BY, Ma ZS, Xu JJ, Yang B, Li H, et al. A retrospective case series of segmental zoster paresis of limbs: Clinical, electrophysiological and imaging characteristics. BMC Neurol 2018;18:121. [Google Scholar]
- 8.Yoleri O, Olmez N, Oztura I, Sengül I, Günaydin R, Memiş A. Segmental zoster paresis of the upper extremity: A case report. Arch Phys Med Rehabil 2005;86:1492-4. [Google Scholar]
- 9.Opstelten W, Eekhof J, Neven AK, Verheij T. Treatment of herpes zoster. Can Fam Physician 2008;54:373-7. [Google Scholar]
- 10.Artus M, Holt TA, Rees J. The painful shoulder: An update on assessment, treatment, and referral. Br J Gen Pract 2014;64:e593-5. [Google Scholar]
- 11.Melikoglu M, Melikoglu MA. An unusual cause of shoulder pain; Herpes zoster induced brachial plexopathy, a case report and review of the literature. J Back Musculoskeletal Rehabil 2013;26:243-5. [Google Scholar]
- 12.Park S, Ganji P, Ji J, Park SH. Transient motor paresis caused by herpes zoster. J Shoulder Elbow Surg 2016;25:e309-12. [Google Scholar]
- 13.Chen G, Tuan S, Liou I, Huang H, Hu Y, Wu S. Segmental zoster paresis of unilateral upper extremity. A case report and literature review. Medicine (Baltimore) 2020;99:e20466. [Google Scholar]
- 14.Aktas I, Akgun K, Gunduz OH. Axillary mononeuropathy after herpes zoster infection mimicking subacromial impingement syndrome. Am J Physical Med Rehabil 2008;87:859-61. [Google Scholar]
- 15.Yaszay B, Jablecki CK, Safran MR. Zoster paresis of the shoulder. Case report and review of the literature. Clin Orthop Relat Res 2000;377:112-8. [Google Scholar]