Meticulous monitoring, patient selection, adherence to surgical protocols, and continuous quality improvement efforts are important to minimize cardiovascular complications and optimize outcomes in patients undergoing cemented hip arthroplasty.
Dr. Indrajeet Kumar, Department of Orthopaedics, IGIMS, Patna-14, India. Email id: indrajeet98ortho@gmail.com
Introduction: Bone cementation has various effects on hemodynamics including potentially fatal bone cement implantation syndrome (BCIS). Most of the studies on BCIS are from developed countries. We have studied the effect of bone cement on hemodynamics in hip arthroplasty in the eastern Indian population and compared it with the available literature.
Materials and Methods: This prospective study was done by a team of orthopedic surgeons and anesthesiologists in a tertiary center in eastern India between March 2020 and December 2022.
Result: Seventy-two patients (Male 38: and Female 34) of age between 25 and 100 years fulfilling the inclusion criteria were included. In 43 patients (28/72, 38.88%) systolic and diastolic blood pressure fell in the range of 10 mmHg, in 22 patients (22/72, 30.56%) fall in blood pressure was in the range of 10–20 mmHg, and more than 20 mmHg fall in blood pressure were seen in seven patients (7/72, 9.72%). SPO2 decreased from 97–100% to 94–96% in 28 patients and 90–93% in six patients, which began to rise after 5 min of cementing and returned to normal after 10 min. Arrhythmias were seen in 16 patients with multiple comorbidity. Two patients had a cardiac arrest and one patient died after 6 h in the intensive care unit.
Conclusion: Pre-operative evaluation, perioperative monitoring of hemodynamic parameters during cementing especially in high-risk patients with multiple comorbidities, and taking essential precautions during cemented arthroplasty are the key to preventing complications like BCIS.
Keywords: Total hip arthroplasty, hemiarthroplasty, bone cement, bone cement implantation syndrome, hemodynamics, Eastern India.
Bone cement implantation has a significant influence on hemodynamics in patients undergoing arthroplasty [1]. However, most of the patients have no clinical symptoms only a few patients have symptoms of bone cement implantation syndrome (BCIS). It is characterized by hypoxia, sudden loss of arterial pressure, pulmonary hypertension, arrhythmias, loss of consciousness, and eventually cardiac arrest [2]. It is a rare and potentially fatal perioperative, reversible time limited phenomena complication of bone cement implantation if not immediately taken care of [3,4]. Therefore, it is important to know about hemodynamics changes during cement implantation and the precautions to be taken before putting the bone cement. Cemented arthroplasty either total or partial is beneficial in osteopenic or osteoporotic bone where deeper penetration of cement provides excellent fixation across a wide surface area [5], where the enlarged metaphyseal region makes it difficult to gain adequate purchase with an uncemented component [6]. A number of meta-analyses and literature reviews have concluded that cemented fixation is the gold standard in total hip arthroplasty (THA) in terms of reoperation rate in all patients regardless of age [7-9]. At present, there is no agreed definition of BCIS and is a less understood phenomenon [10]. Clinical presentation of BCIS begins as a spectrum of signs suggesting hypoxia and hypotension; if these signs are not reversed, it ends with right-sided heart failure and cardiac arrest [11]. This usually occurs during cement intrusion, prosthesis insertion, and joint reduction but could also occur a few hours later. Most of the studies on BCIS are from developed countries; we have studied the effect of bone cement on hemodynamics in hip arthroplasty in the Eastern Indian population and compared it with the available literature.
The aim of this prospective cross-sectional study, conducted by a team of orthopedic surgeons and anesthesiologists at a tertiary center in eastern India from March 2021 to December 2022, is to assess the cardiovascular effects and complications associated with bone cement implantation during orthopedic procedures. The objective is to evaluate the physiological changes in patients aged 25–100 years, both male and female, undergoing bone cement implantation. Moribund patients and those with an ejection fraction of <30% were excluded from the study. The hypothesis is that bone cement implantation may lead to cardiovascular complications, including arrhythmias (such as atrial fibrillation, atrial flutter, AV block, and ventricular arrhythmias), embolism, and acute renal failure.
Specific anesthetic measures aimed to enhance patient safety and minimize the risk of BCIS-related complications include vigilant monitoring of the patient’s vital signs including continuous monitoring of oxygen saturation (SPO2), blood pressure, and heart rate (HR). Adequate anesthesia depth and muscle relaxation are ensured to minimize patient movement, reducing the risk of bone cement extravasation. Proper positioning of the patient, particularly ensuring adequate ventilation and avoiding compression of major vessels, is crucial. Intravenous fluids are administered at an appropriate rate to maintain hydration and hemodynamic stability during the procedure. Proper fluid management and medication administration contribute to optimizing the patient’s physiological status. The anesthetic team remains prepared to manage any emergent complications promptly.
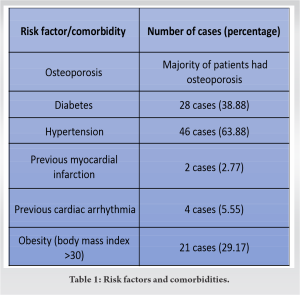
The study parameters include monitoring pulse rate, blood pressure (both systolic and diastolic), mean arterial pressure, peripheral SPO2, and Electrocardiogram (ECG) changes at various time points: Before anesthesia, before cementing, and after cementing, at 0, 5, 10, 15, and 30 min, as well as 24-h and 7-day post-implantation. For patients with multiple comorbidities or severe pre-existing diseases, central venous pressure and invasive blood pressure measurements were also conducted (Table 1). As a preventive measure against BCIS, the femoral canal was done using normal saline lavage using a 20 mL syringe to clean the surgical site and remove fat, blood, and debris before implantation. A cement restrictor was then inserted at an appropriate depth, and the femoral canal was packed with gauze soaked in hydrogen peroxide while the cement was prepared (Table 2). A suction catheter was used during cement filling to minimize the risk of cement extravasation and embolization. Before cementation, peroxide packing was carried out to ensure the sterility of the surgical site and reduce the risk of infection, which could exacerbate BCIS Cement mixing was performed manually, and a cement gun or digital pressure was used for insertion. Cardiovascular complications were recorded following a standard protocol for cementation, including arrhythmias, embolism, and acute renal failure. An increase in serum creatinine to at least 1.5 times a known or anticipated baseline within 7 days or a decrease in urine excretion to <0.5 mL/kg body weight/hour for at least 6 h was considered as acute renal failure. This is the standard protocol for cementation in the study followed by all surgeons during the study.
A total of 72 patients underwent cemented hip arthroplasty at our center during the study period from March 2021 to December 2022, meeting the inclusion criteria. Among them, left-sided arthroplasty was performed in 41 patients, and right-sided in 31 patients, with a slight male predominance (M:F = 38:34). The age of patients ranged from 28 to 98 years, with a mean age of 62.26 years.
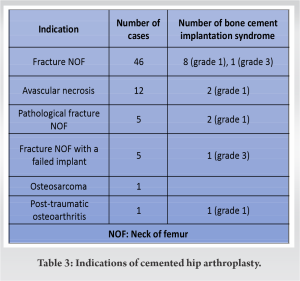
The assessment of patient risk factors and comorbidities were assessed, as these influence the incidence and severity of BCIS by impacting cardiovascular health and bone fragility. Among the patients, the majority had osteoporosis, and 21 patients were obese. Hypertension was present in 46 cases (63.88%). Diabetes affected 28 cases (38.88%). In addition, a history of myocardial infarction and cardiac arrhythmia was noted in 2.77% and 5.55% of patients, respectively, highlighting the need for careful cardiovascular monitoring (Table 1). The indications for cemented arthroplasty included fracture neck of the femur (NOF) in 46 patients, avascular necrosis (AVN) of the femoral head in 12 patients, pathological fracture of the femoral neck in five patients, fracture NOF with the failed implant in situ in five patients, osteosarcoma of the proximal femur in one patient, and post-traumatic osteoarthritis in one patient (Table 3). Cemented bipolar prosthesis was used in 56 cases, including 28 modular, 25 nonmodular, and three with mega prostheses. Cemented total hip replacement was performed in 16 cases (Table 4). The statistical analysis of the data provides valuable insights into the cardiovascular effects and complications associated with cemented hip arthroplasty. There were nine cases in which larger prosthesis were used (three in megaprosthesis and six in revision cases out of which four cases developed Grade 1 BCIS.
- Blood pressure changes: There was a fall in both systolic and diastolic blood pressure (DBP) in the range of 10 mmHg in 43 patients (28/72, 38.88%), in the range of 10–20 mmHg in 22 patients (22/72, 30.56%) and more than 20 mmHg in seven patients (7/72, 9.72%), which begin to rise after 5 min of cementing and returned to normal after 10 min. The observed decreases in both systolic and DBP during cemented hip arthroplasty suggest a transient hemodynamic effect associated with the procedure. A paired t-test comparing baseline systolic blood pressure (SBP) measurements to measurements taken at various time points during the procedure revealed a significant decrease in SBP immediately after cementing (P < 0.05) (Table 5). However, SBP returned to baseline levels within 10 min post-cementing. Similarly, DBP showed a significant decrease immediately after cementing (P < 0.05). DBP also returned to baseline levels within 10-min post-cementing. Analysis of variance (ANOVA) was used to assess whether there were significant differences in blood pressure changes among different time points (before anesthesia, before cementing, after cementing, 0-, 5-, 10-, 15-, 30-min, 24-h, and 7-day post-implantation). The results showed significant differences in blood pressure changes over time (P < 0.05), indicating variations in hemodynamic responses throughout the procedure and recovery period. ANOVA was also done to determine whether there were significant differences in blood pressure changes among patient subgroups based on factors such as age, gender, comorbidities, and type of arthroplasty procedure. The analysis revealed no significant differences in blood pressure changes among these patient subgroups (P > 0.05), suggesting that blood pressure responses to cemented hip arthroplasty were consistent across different patient populations.
- Peripheral oxygen saturation (SPO2): One minute after bone cement implantation, SPO2 was decreased from 97–100% to 94–96% in 28 patients, and 90–93% in 6 patients. It reached the lowest level within 5 min of cementing, began to rise 5 min after, and returned to normal 10 min after cementing. No significant changes were seen at 30 min, 24 h, and after 7 days. Paired t-tests comparing baseline SPO2 measurements to SPO2 measurements at various time points during the procedure. There was a transient oxygen desaturation immediately after cementing, followed by a gradual return of SPO2 at baseline levels, within 10-min post-cementing. ANOVA also indicates significant differences in SPO2 changes among different time points (before anesthesia, before cementing, after cementing, 0-, 5-, 10-, 15-, 30-min, 24-h, and 7-day post-implantation). The analysis demonstrated significant differences in SPO2 changes over time (P < 0.05), indicating variations in SPO2 responses throughout the procedure and recovery period.
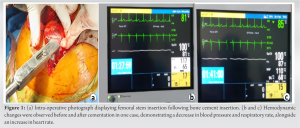
- HR: The slight increase in HR observed in most patients suggests a sympathetic response to the surgical stimulus (Fig. 1). Paired t-tests comparing baseline HR measurements to HR measurements at various time points during the procedure revealed a significant increase in HR immediately after cementing (P < 0.05). However, HR returned to baseline levels within 10-min post-cementing. ANOVA was employed to determine whether there were significant differences in HR changes among different time points (before anesthesia, before cementing, after cementing, 0-, 5-, 10-, 15-, 30-min, 24-h, and 7-day post-implantation). The analysis demonstrated significant differences in HR changes over time (P < 0.05), indicating variations in HR responses throughout the procedure and recovery period.
- ECG changes: We observed changes in ECG rhythm in 16 cases of patients, almost all patients developed sinus tachycardia. One patient with a history of myocardial ischemia exhibited ST segment elevation and T wave flattening. Another patient experienced QT interval prolongation, which resolved without incident. In addition, four patients presented with ventricular ectopy. During the course of observation, two patients experienced flat lines. However, they were successfully revived through cardiopulmonary resuscitation (CPR), with sinus rhythm reversion occurring after 12 and 20 min, respectively. Subsequently, both were intubated and transferred to the intensive care unit (ICU). Tragically, one patient later developed ventricular tachycardia and succumbed within 6 h. Despite attempts at cardioversion, revival was not achieved.
The observed changes in ECG rhythm in patients with multiple comorbidities indicate potential cardiac stress during the procedure. The Chi-square test (χ²) demonstrates a significant association between ECG changes and cardiac complications, emphasizing the importance of monitoring ECG during the procedure to identify patients at risk for adverse cardiac events.
- Cardiac complications: Two patients had a cardiac arrest and resuscitated in the operating theatre, and transferred to the ICU, out of the two, one patient was died after 6 h in ICU (Table 5). The occurrence of cardiac arrest indicates the importance of vigilance and prompt management of cardiovascular complications during cemented hip arthroplasty. To assess the association between patient characteristics and the incidence of cardiac complications, the χ², indicates a significant association between hypertension and the incidence of cardiac complications suggesting that patients with hypertension are more likely to experience cardiac complications during cemented hip arthroplasty. However, no significant associations were found between other risk factors/comorbidities such as osteoporosis, diabetes, previous myocardial infarction, or previous cardiac arrhythmia, and the occurrence of cardiac complications (P > 0.05). These findings emphasize the importance of pre-operative risk assessment and management of hypertension in patients undergoing cemented hip arthroplasty to reduce the risk of cardiac complications.
After hip arthroplasty, patients typically aim for discharge following the second dressing change on the 4th or 5th day post-surgery. However, for patients who developed BCIS, the average hospitalization duration increased to 14 days (ranging from 8 to 25 days), compared to the overall patient hospitalization mean of 7 days (ranging from 3 days to 25 days). Among the 13 patients with BCIS Grade 1, experienced respiratory compromise in four cases, managed medically in the ward. In addition, two patients who developed delirium presented with electrolyte imbalances (hyponatremia), conservatively managed. Except for those who experienced cardiac arrest, no patients required ICU admission. It is noteworthy to mention that there were no cases of acute renal failure, and symptomatic DVT was observed. 13 patients out of 72 sustained either moderate hypoxia (arterial SPO2 <94%) or hypotension (a decrease in systolic arterial pressure [SAP] >20%) and were thus classified as Grade I. No patients were classified as Grade II because none experienced severe hypoxia (arterial SPO2 <88%) or profound hypotension (a decrease in SAP >40%) or unexpected loss of consciousness. Two out of 72 patients experienced cardiovascular failure and required CPR, thus classified as type 3. Understanding the significance of observed changes and their potential implications for outcomes is crucial for optimizing patient care and surgical outcomes in this patient population.
BCIS is a well-known cause of morbidity and is sometimes fatal in patients undergoing cemented arthroplasty of the hip joint [2]. In this study, BCIS was seen in patients with age more than 60 years and with multiple comorbidities. The assessment of risk factors and comorbidities is crucial in managing BCIS during cemented hip arthroplasty [13]. The role of The American Society of Anesthesiologists (ASA) classification system during pre-operative check-up assess a patient’s health status and predict operative risk. This also is one factor that influences decision-making, prosthetic selection (long vs. short prosthesis), type of hemiarthroplasty (cemented vs. cementless) informed consent, and resource allocation. Surgeons and anesthesiologists use ASA classes to identify patients needing additional evaluation, closer monitoring, or post-operative care in higher acuity settings. Risk factors, such as obesity, osteoporosis, angina, COPD, and other cardiopulmonary issues significantly influence the incidence and severity of BCIS [14]. Among these patients, the majority had osteoporosis, which increases the risk of fat and marrow embolization during cement pressurization, thereby elevating the risk of BCIS [15]. Hypertension was present in 46 cases (63.88%), posing a significant risk for hemodynamic instability during surgery [16]. In addition, the use of antihypertensive drugs and medications affecting coagulation must be carefully considered due to their impact on patient stability during surgery [17]. Patients with compromised cardiopulmonary function are particularly susceptible to the adverse effects of BCIS, such as hypoxia and pulmonary hypertension. A thorough medical history, including the assessment of angina, COPD, and other cardiopulmonary issues, is essential. A history of myocardial infarction (2 cases, 2.77%) and cardiac arrhythmia (4 cases, 5.55%) indicates underlying cardiac vulnerabilities. These conditions can worsen the cardiovascular collapse associated with severe BCIS and necessitate careful intraoperative monitoring and management. Diabetes affected 28 cases (38.88%), complicating perioperative management due to potential microvascular issues and impaired wound healing, which may also affect the body’s response to embolic events associated with BCIS. Twenty-one patients with obesity (BMI > 30) were identified, increasing the risk of BCIS due to factors such as heightened blood loss, compromised cardiovascular function, and venous stasis [14]. Donaldson and colleagues proposed a severity classification of BCIS: Grade 1 was defined as moderate hypoxia (arterial SPO2 <94%) or hypotension [a decrease in SAP >20%], Grade 2 as severe hypoxia (arterial SPO2 <88%) or hypotension (a decrease in SAP >40%) or unexpected loss of consciousness, and finally, Grade 3, which was defined as cardiovascular collapse requiring CPR [18]. The severity of BCIS directly correlates with mortality risk, with higher mortality rates observed in cases of moderate-to-severe BCIS. Patients with poor baseline health are at higher risk of mortality even with less severe forms of BCIS [13]. Early recognition, prompt intervention, and appropriate supportive care are vital for improving outcomes and reducing mortality associated with this potentially life-threatening complication. The choice between short and long prostheses can significantly affect the incidence and severity of BCIS [18]. Long prostheses, due to their larger surface area, increased bone cement volume, and the need for more extensive surgical manipulation, may pose a higher risk of BCIS compared to short prostheses [19]. In our study, involving nine cases where larger prostheses were used, four cases developed Grade 1 BCIS. We have studied the effect of bone cement on hemodynamics in hip arthroplasty in 72 patients (M:F= 38:34) and the mean age was 62.26 years (age range 28–98) (Table 1). A similar study done by Qi et al. on 128 patients had slight female predominance (M:F = 54:74) and more elderly patients (mean age 83.5, age range 75–92) unlike our study. Qi et al. also had shown that both SBP and DBP have fallen significantly just after cementing, and begin to rise and became normal within 5–10 min after cementing [1]. Qi et al., also studied the relation to SPO2 with cementing and found that it decreased significantly just 1 min after the cement implantation, reached the lowest point at 4 min, began to rise after that, and returned to normal 10 min after implantation [1]. We also had similar findings in our study. We have noticed a decrease in SPO2 in all cases just after cementing the femoral canal, Nolan also found a 10–15% decrease in PaO2 following implantation of both acetabular and femoral components [20]. Astawa explained that a temporary substantial reduction occurs in PaO2 occurs in a few whiles there is no reduction in a few [21]. Soleimanha et al., have not noticed any statistically significant change in SpO2, pCo2, and PaO2 levels during cementing [22]. There was an initial decrease in blood pressure after cementing which began to rise after 5 min in our study. Fujita et al. found an increase in blood pressure for about 4 min after cementation on the acetabular side and for 2 min after cementation on the femoral side [23]. Nolan found a 20% increase in mean arterial pressure after insertion of the femoral stem in cemented type THA [20]. The increase in blood pressure may be due to microembolization which may be the reason for pulmonary hypertension. Miyamoto et al. concluded that there is no significant intraoperative blood pressure change during cemented hemiarthroplasty if the standard modern cement technique was used, thus bone cement is safe in elderly patients even with lots of medical comorbidities [24]. In Qi study, found a slight increase in HR without statistical significance [1]. Which is similar to our findings. Changes in ECG i.e., the incidence of arrhythmia during surgery were found in 16 cases (21.2%). Soleimanha et al., have reported arrhythmia, only in those having a history of cardiovascular disease [22]. In Olesen’s study of patients undergoing cemented hemiarthroplasty, the overall incidence of BCIS was 28%. Although it is fatal in a limited number of cases [25]. In our study cardiac arrest has occurred in two cases (2.77%). Out of which one patient was revived and one resulted in death. 30-day and long-term mortality were significantly higher after a moderate or severe episode of BCIS [25]. We have not noticed any other mortality later within 1 year period. A patient who develops BCIS requires longer hospitalization, as seen in our patients as well [13]. Cemented hip arthroplasty, especially in cases with fractures or AVN, can pose a higher risk of BCIS Fracture NOF and AVN, due to compromised bone integrity and the extensive use of bone cement [13]. The risk is heightened in patients undergoing procedures for fracture neck of the femur, pathological fractures, and other indications where bone integrity is compromised (Table 3). The type of arthroplasty procedure can influence the likelihood and severity of BCIS. We have used modular as well as non-modular implants in almost equal numbers of patients and have roughly similar hemodynamic changes in both groups of patients (Table 4). Literature suggests that the incidence and severity of BCIS can indeed vary between modular and non-modular implants due to differences in surgical techniques and the volume of cement used [26,27]. Modular implants often involve a two-stage process where components are assembled in situ. This might reduce the amount of cement used at any 1 time, potentially lowering the immediate risk of a large embolic load compared to non-modular implants. The staged nature of modular implant insertion can allow for better control over the cementing process, potentially reducing the severity of BCIS if it occurs. Non-modular implants are typically inserted as a single unit, often requiring a larger volume of cement to be used at once. This can increase the risk of BCIS due to the sudden release of embolic material into the bloodstream. The single-step nature of non-modular implant insertion can lead to a more abrupt hemodynamic change, possibly resulting in more severe manifestations of BCIS. Thus, when planning hip arthroplasty procedures, especially in high-risk patients, surgeons might prefer modular implants to mitigate the risk of BCIS. In addition, meticulous surgical techniques and careful monitoring during the cementing process are crucial regardless of the implant type to minimize the risk and severity of BCIS. Jet lavage and making femoral boreholes, are methods aimed at minimizing the potential for bone cement embolization. These were not employed in any case of the study. Instead, we have done femoral canal lavage using a 20 mL syringe with normal saline in all the cases as it helps in reducing the pulmonary physiological disturbance and embolic load, and it should be carried out before cementing the medullary cavity [28-31]. In all cases, the femoral canal is plugged with a well-fitting cement restrictor for good filling, and pressurization and decreases physiological disturbance during cement and prosthesis insertion [32,33]. Intraoperative blood loss was 300 ± 150 mL. There was no intraoperative fracture. Operative time was 87.2 ± 17.2 min. High-risk factors for the development of BCIS include old age, compromised cardiac function and physical reserve, higher grades of ASA levels, pulmonary hypertension, secondaries, pathological fractures, concomitant hip fractures, intertrochanteric fractures, and significant cardiovascular and respiratory disease [23,34]. Enlarged porous cavities in osteoporosis fracture type, metastatic bone disease, and femoral canal diameter of more than 21 mm, increase the risk of emboli generation. In our study, majority of patients had osteoporosis, 28 patients had diabetes (38.88%), 46 had hypertension (63.88), 2 had a previous myocardial infarction (2.77%), and four had h/o cardiac arrhythmia (5.55%). Medications such as H1 and H2 antagonists, methylprednisolone, inotropes, vasopressors, and some alterations in surgical technique, can prevent the progression of BCIS [15]. Tomé Roca et al. suggested extreme cautions for patients with cardiac defects that favor communication between the pulmonary and systemic circulation [35]. Patients with comorbidities and other risk factors were monitored closely during and after bone cementation [23]. Fluid resuscitation to maintain preload and inotropes to support ventricular contractility is recommended. Rapid and aggressive resuscitation including CPR, administering 100% oxygen, rapid drug administration using a central venous line, prompt supportive care, and communication between the orthopedic surgeon and anesthesiologist is the cornerstone of treating BCIS [15, 28]. Following the above guidelines, we were able to save one out of two patients who suffered cardiac arrest. Anticoagulation, percutaneous removal, cardiopulmonary bypass and surgical removal, corticosteroids, and antibiotics are a few of the treatment options [36]. There was the use of inotropes anticoagulation, corticosteroid, and antibiotics in addition to close monitoring of fluid and vitals done in ICU in both the patients who developed BCIS. Rarely polymethyl methacrylate bone cement produces an inflammatory response in a few allergic patients, which may result in pain, loosening of the cemented implant, swelling, skin reactions such as blisters and fistula formation. [37-39] Potential bone cement allergens include acrylates, benzoyl peroxide, N, N-dimethyl-p-toluidine, and gentamicin. It is imperative to identify such patients and patients with modify their treatment by using cementless procedures [37]. We have noticed skin reactions such as redness and swelling around the suture line in 18 of our cases during the first dressing on the 3rd day, after stopping the antibiotics after the fourth dose on the 2nd day. There was no associated warmth in seven of such cases, which subsided during subsequent dressing by themselves. Thus, retrospectively diagnosis was more in favor of allergic reaction by cement than infection in seven cases. This was supported by Ceynowa et al. study, he mentioned that cement skin allergy may take several days for the symptoms to appear [38, 39]. Fluid-filled blisters were noticed in two of the cases. Both of them subsided by themselves. The limitation of our study is a smaller number of patients, in our study, a heterogeneous group of patients in terms of age, comorbidities (28 patients have diabetes (38.88%), 46 have hypertension (63.88), h/o previous myocardial infarction in 2 (2.77%), h/o previous cardiac arrhythmia in 4 (5.55 %) patients. The above risk factors and comorbidities may cause bias in applying our result to large groups of the population.
BCIS is characterized by a decrease in SPO2, HR, blood pressure, arrhythmias, an increase in pulmonary vascular resistance, and sometimes cardiac arrest. Cementation of the femoral canal during arthroplasty in the elderly affects hemodynamics, which can result in cardiac arrest and even death. An orthopedic surgeon and anesthesiologist must be aware of high-risk factors, follow preventive measures, as well as knowing when and how to intervene to reduce this effect and further mishappening. Close monitoring of vitals and taking essential precautions during bone cement implantation in hip arthroplasty is the key to preventing potentially fatal complications, especially in high-risk patients.
Our study highlights the significance of vigilant hemodynamic monitoring during cemented hip arthroplasty. Pre-operative assessment and adherence to surgical protocols are crucial in minimizing the risk of cardiovascular complications such as BCIS. Although diligent monitoring and strict adherence to established protocols, clinicians can enhance patient outcomes and minimize the likelihood of adverse events occurring during cemented hip arthroplasty.
References
- 1.Qi X, Zhang Y, Pan J, Ma L, Wang L, Wang J. Effect of bone cement implantation on haemodynamics in elderly patients and preventive measure in cemented hemiarthroplasty. Biomed Res Int 2015;2015:568019. [Google Scholar]
- 2.Razuin R, Effat O, Shahidan MN, Shama DV, Miswan MF. Bone cement implantation syndrome. Malays J Pathol 2013;35:87-90. [Google Scholar]
- 3.Maggs J, Wilson M. The relative merits of cemented and uncemented prostheses in total hip arthroplasty. Indian J Orthop 2017;51:377-85. [Google Scholar]
- 4.Hines CB. Understanding bone cement implantation syndrome. AANA J 2018;86:433-41. [Google Scholar]
- 5.Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone 1993;14:231-42. [Google Scholar]
- 6.Murray DW. Cemented femoral fixation: The North Atlantic divide. Bone Joint J 2013;95-B:51-2. [Google Scholar]
- 7.Troelsen A, Malchau E, Sillesen N, Malchau H. A review of current fixation use and registry outcomes in total hip arthroplasty: The uncemented paradox. Clin Orthop Relat Res 2013;471:2052-9. [Google Scholar]
- 8.Corbett KL, Losina E, Nti AA, Prokopetz JJ, Katz JN. Population-based rates of revision of primary total hip arthroplasty: A systematic review. PLoS One 2010;5:e13520. [Google Scholar]
- 9.Morshed S, Bozic KJ, Ries MD, Malchau H, Colford JM Jr. Comparison of cemented and uncemented fixation in total hip replacement: A meta-analysis. Acta Orthop 2007;78:315-26. [Google Scholar]
- 10.Khanna G, Cernovsky J. Bone cement and the implications for anaesthesia. Br J Anaesth 2012;12:213-6. [Google Scholar]
- 11.Hines CB, Collins-Yoder A. Bone cement implantation syndrome: Key concepts for perioperative nurses. AORN J 2019;109:202-16. [Google Scholar]
- 12.Zhou AK, Girish M, Thahir A, An Lim J, Tran C, Patel S, et al. The role of hydrogen peroxide in hip arthroplasty: A narrative review. J Perioper Pract 2022;32:178-82. [Google Scholar]
- 13.Weingärtner K, Störmann P, Schramm D, Wutzler S, Zacharowski K, Marzi I, et al. Bone cement implantation syndrome in cemented hip hemiarthroplasty-a persistent risk. Eur J Trauma Emerg Surg 2022;48:721-9. [Google Scholar]
- 14.Schwarzkopf E, Sachdev R, Flynn J, Boddapati V, Padilla RE, Prince DE. Occurrence, risk factors, and outcomes of bone cement implantation syndrome after hemi and total hip arthroplasty in cancer patients. J Surg Oncol 2019;120:1008-15. [Google Scholar]
- 15.Dradjat RS, Pradana AS, Putra DP, Hexa Pandiangan RA, Cendikiawan F, Mustamsir E. Successful management of severe manifestation bone cemented implantation syndrome during hemiarthroplasty surgery in patient with multiple comorbidities: A case report. Int J Surg Case Rep 2021;78:331-5. [Google Scholar]
- 16.Bruynzeel H, Feelders RA, Groenland TH, van den Meiracker AH, van Eijck CH, Lange JF, et al. Risk factors for hemodynamic instability during surgery for pheochromocytoma. J Clin Endocrinol Metab 2010;95:678-85. [Google Scholar]
- 17.Ganotakis ES, Papadakis JA, Vrentzos GE, Mikhailidis DP. The effects of antihypertensive therapy on haemostatic parameters. Curr Pharm Des 2003;9:2445-64. [Google Scholar]
- 18.Donaldson AJ, Thomson HE, Harper NJ, Kenny NW. Bone cement implantation syndrome. Br J Anaesth 2009;102:12-22. [Google Scholar]
- 19.Al-Husinat L, Jouryyeh B, Al Sharie S, Al Modanat Z, Jurieh A, Al Hseinat L, et al. Bone cement and its anesthetic complications: A narrative review. J Clin Med 2023;12:2105. [Google Scholar]
- 20.Nolan J. Arterial oxygenation and mean arterial blood pressure in patients undergoing total hip replacement: Cemented versus uncemented components. Anaesthesia 1994;49:293-9. [Google Scholar]
- 21.Astawa P. Hemodynamic changes in patients undergoing cemented total hip replacement surgery: A literature review. Bali Med J 2020;9:520-3. [Google Scholar]
- 22.Soleimanha M, Sedighinejad A, Haghighi M, Nabi BN, Mirbolook AR, Mardani-Kivi M. Hemodynamic and arterial blood gas parameters during cemented hip hemiarthroplasty in elderly patients. Arch Bone Jt Surg 2014;2:163-7. [Google Scholar]
- 23.Fujita H, Okumura T, Hara H, Toda H, Harada H, Nishimura R, et al. Monitoring of blood pressure during total hip arthroplasty using the interface bioactive bone cement (IBBC) technique. J Orthop Sci 2015;20:347-56. [Google Scholar]
- 24.Miyamoto S, Nakamura J, Iida S, Shigemura T, Kishida S, Abe I, et al. Intraoperative blood pressure changes during cemented versus uncemented bipolar hemiarthroplasty for displaced femoral neck fracture: A multi-center cohort study: The effect of bone cement for bipolar hemiarthroplasty in elderly patients. Arch Orthop Trauma Surg 2017;137:523-9. [Google Scholar]
- 25.Olsen F, Kotyra M, Houltz E, Ricksten SE. Bone cement implantation syndrome in cemented hemiarthroplasty for femoral neck fracture: Incidence, risk factors, and effect on outcome. Br J Anaesth 2014;113:800-6. [Google Scholar]
- 26.Chulsomlee K, Prukviwat S, Tuntiyatorn P, Vasaruchapong S, Kulachote N, Sirisreetreerux N, et al. Correlation between shape-closed femoral stem design and bone cement implantation syndrome in osteoporotic elderly femoral neck fracture undergoing cemented hip arthroplasty: A retrospective case-control study in 128 patients. Orthop Traumatol Surg Res 2023;109:103450. [Google Scholar]
- 27.Jaffe JD, Edwards CJ, Hamzi R, Khanna AK, Olsen F. Bone cement implantation syndrome: Incidence and associated factors in a United States setting. Cureus 2022;14:e31908. [Google Scholar]
- 28.Byrick RJ, Bell RS, Kay JC, Waddell JP, Mullen JB. High-volume, high-pressure pulsatile lavage during cemented arthroplasty. J Bone Joint Surg Am 1989;71:1331-6. [Google Scholar]
- 29.Christie J, Robinson CM, Singer B, Ray DC. Medullary lavage reduces embolic phenomena and cardiopulmonary changes during cemented hemiarthroplasty. J Bone Joint Surg Br 1995;77:456-9. [Google Scholar]
- 30.Breusch SJ, Reitzel T, Schneider U, Volkmann M, Ewerbeck V, Lukoschek M. Cemented hip prosthesis implantation--Decreasing the rate of fat embolism with pulsed pressure lavage. Orthopade 2000;29:578-86. [Google Scholar]
- 31.Malchau H, Herberts P, Soderman P, Oden A. Prognosis of Total Hip Replacements. Update and Validation of Results from The swedish National Hip Arthroplasty Register 1979-1998. In: Presented at the 67th Annual Meeting of the American Academy of Orthopaedic Surgeons, Orlando; 2000. [Google Scholar]
- 32.Heisel C, Norman T, Rupp R, Pritsch M, Ewerbeck V, Breusch SJ. In vitro performance of intramedullary cement restrictors in total hip arthroplasty. J Biomech 2003;36:835-43. [Google Scholar]
- 33.McCaskie AW, Barnes MR, Lin E, Harper WM, Gregg PJ. Cement pressurisation during hip replacement. J Bone Joint Surg Br 1997;79:379-84. [Google Scholar]
- 34.Segerstad MH, Olsen F, Patel A, Houltz E, Nellgård B, Ricksten SE. Pulmonary haemodynamics and right ventricular function in cemented vs uncemented total hip arthroplasty-A randomized trial. Acta Anaesthesiol Scand 2019;63:298-305. [Google Scholar]
- 35.Tomé Roca JL, López Martín R, Baca Morilla Y, de la Linde Valverde C. Paradoxical intraoperative embolism in a patient with Eisenmenger syndrome undergoing hip arthroplasty. Rev Esp Anestesiol Reanim (Engl Ed) 2019;66:439-42. [Google Scholar]
- 36.Sinha N, Padegal V, Satyanarayana S, Santosh HK. Pulmonary cement embolization after vertebroplasty, an uncommon presentation of pulmonary embolism: A case report and literature review. Lung India 2015;32:602-5. [Google Scholar]
- 37.Kaplan K, Della Valle CJ, Haines K, Zuckerman JD. Preoperative identification of a bone-cement allergy in a patient undergoing total knee arthroplasty. J Arthroplasty 2002;17:788-91. [Google Scholar]
- 38.Bircher A, Friederich NF, Seelig W, Scherer K. Allergic complications from orthopaedic joint implants: The role of delayed hypersensitivity to benzoyl peroxide in bone cement. Contact Dermatitis 2012;66:20-6. [Google Scholar]
- 39.Ceynowa M, Zerdzicki K, Klosowski P, Zrodowski M, Pankowski R, Roclawski M, et al. The cement-bone bond is weaker than cement-cement bond in cement-in-cement revision arthroplasty. A comparative biomechanical study. PLoS One 2021;16:e0246740. [Google Scholar]