The treatment of an osteochondroma of the hip is a challenge. Total joint replacement is an option for satisfactory resolution.
Dr. Rubén Daniel Arellano Pérez Vertti, Department of Orthopaedic Surgery, Autonomous University of Coahuila, Faculty of Medicine, Torreón, Avenida Morelos 900 Oriente, Torreón, Coahuila, Mexico. E-mail: arellanodaniel1969@gmail.com
Introduction: Osteochondroma is the most common benign bone tumor (20–50%). It is located predominantly in the metaphysis of the long bones, and much less frequently, the proximal femur and acetabulum. Osteochondroma can eventually lead to hip osteoarthritis and limit patients’ functional activities. Determining optimal treatment can be difficult due to the high risk of avascular necrosis in surgical resections.
Case Report: A 44-year-old male from Sabinas Coahuila, Mexico, a priest by profession, who presents for consultation with right inguinal pain of 18 months’ duration. The patient had been treated conservatively with rest, non-steroidal anti-inflammatory drugs, and physical therapy without showing improvement in his symptoms. The anteroposterior radiograph of the pelvis and axial tomography showed an oval bone excrescence with well-defined margins in the acetabular and intra-articular region of the hip, which caused a decrease in joint space but without soft tissue infiltration. Tumor resection and total hip replacement were the treatment options. The histopathological study concluded an osteochondroma. After 25 months of post-operative follow-up, radiographic studies show no evidence of lesion recurrence. The functional improvement is 98 points on the Harris scale; the patient typically performs his daily living and work activities.
Conclusion: Treating intra-articular osteochondroma of the hip can be challenging for the orthopedic surgeon. For osteochondroma resulting in secondary osteoarthrosis of the hip joint, total hip replacement should be considered an effective method to restore function and assist in returning the patient to previous activities. Thorough pre-operative planning is mandatory to prevent intra- or immediate post-operative risk.
Keywords: Hip, intra-articular osteochondroma, total hip replacement.
Osteochondroma, or cartilaginous exostosis, is the most common benign primary tumor of long bones (20–50%) [1]. Up to 85% of lesions present as solitary, and 15% occur in the context of hereditary multiple exostoses. They can be sessile or pedunculated lesions, and their prevalence is one case per 50,000 inhabitants of the general population [2]. They predominantly arise in childhood and are located in the metaphyses of long bones such as the distal femur, proximal tibia, proximal humerus, and fibula [3]. Similarly, and with a very rare incidence, they can be located in the proximal femur and acetabulum; most cases with intra-articular involvement have been observed in skeletally immature patients and cases with hereditary multiple exostoses [2, 3]. The intra-articular condition of the hip reported in adult patients without evidence of dysplasia is even less frequent [2]. Intra-articular injuries can alter the hip’s normal anatomy, causing acetabular dysplasia, subluxation, or dislocation [1]. Lesions that grow on the lateral part of the femur generally cause pain due to compression of adjacent structures such as muscles, blood vessels, or skin, limiting movement secondary to impingement, bursitis, or esthetic discomfort [3]. Another consequence of the intra-articular location in the hip is the development of osteoarthritis, which can limit patients’ functional activities [4, 5]. The local recurrence of the solitary lesion is usually <2% [6], while the probability of malignant degeneration of a solitary osteochondroma is <1% [5]. Most descriptions of how to treat these tumors are in skeletally immature patients [2, 3, 7] who aim to preserve the joint. In these reports, authors describe open resection and dislocation of the hip with different techniques, such as anterior dislocation with the Ganz technique, resection with the Smith-Petersen approach, direct lateral approach, posterior approach, acetabular osteotomies such as Bernese, Dega, and Shelf, if there is an association with hip dysplasia [6, 7]. The technique of arthroscopic resection of hip osteochondroma by Fernández et al was also reported for the 1st time in 2009, with good results in the short and medium term [8]. However, there are no reports describing tumor resection and placement of a total hip prosthesis as the first treatment option in young adult patients who developed hip osteoarthritis secondary to an intra-articular osteochondroma. Medium-term functional results have been good with this treatment technique [9, 10]. Determining the optimal treatment of this pathological entity can be difficult because some techniques, such as open surgical resection, could increase the risk of avascular necrosis of the hip [4]. There is also a dilemma about solving the condition through tumor resection and placement of total hip prosthesis, especially in the young adult population. In this case report, we present a young adult patient diagnosed with intra-articular osteochondroma of the right hip, treated with tumor resection and total hip joint replacement surgery.
He is a 44-year-old male patient, originally from Sabinas Coahuila, Mexico, a priest by profession, who comes to the orthopedic service complaining of pain in the right inguinal region and a faltering gait for 18 months. Initially, the patient received conservative treatment through rest, restriction of some activities, non-steroidal anti-inflammatory drugs, and physical therapy. However, the patient showed no evidence of improvement in his symptoms.
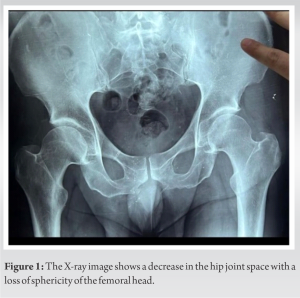
During the physical examination, we noted limping on the patient due to a 2.5 cm shortening of the right lower extremity, hypotrophy of the abductor and quadriceps muscles, pain, crepitation, and decreased passive mobility of the hip in all ranges explored. Faber and Log Roll’s physical tests were positive. An initial 40-point score on the Harris scale showed the hip’s functional status. The patient denied the presence of fever, weight loss, general malaise, or recent trauma. In the anteroposterior radiographic image study of the pelvis (Fig. 1), a slight decrease in the upper joint space was observed, with lower femoral osteophytes, acetabular subchondral sclerosis, and femoral head flattening.
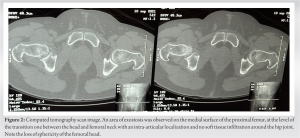
Computed axial tomography showed (Fig. 2) an area of exostosis on the medial surface of the proximal femur, at the level of the transition zone between head and neck, and intra-articular extension, without infiltration of soft planes. Analysis of biochemical tests in blood and urine showed no relevant results. We proposed to carry out tumor resection and placement of a total hip prosthesis. The patient signed informed consent to authorize the surgical procedure and allow publication of the findings.
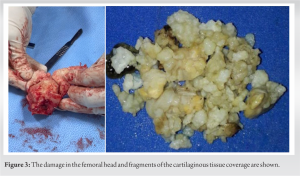
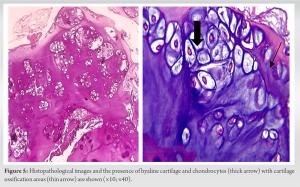
The intraoperative findings showed a bone mass of 2 cm × 1 cm in diameter, firm in consistency, with a layer of cartilaginous-looking tissue. The tumor lesion was completely removed and sent for histopathology studies (Fig. 3).
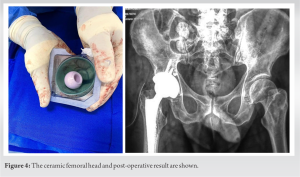
A cemented femoral stem with a cementless acetabular cup and ceramic femoral head was inserted (Fig. 4). The histopathological study showed benign mesenchymal neoplasia constituted by the proliferation of hyaline cartilage, which shows a configuration in nests, chondrocytes with oval, normochromic nuclei, clear cytoplasm, without nuclear atypia, multiple foci of cartilage ossification, and vascularized fibro connective tissue compatible with osteochondroma [11], (Fig. 5).
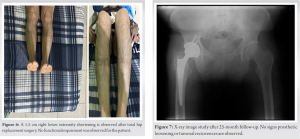
The patient was discharged from the hospital 24 h after the intervention, ambulating with a walker. After 25 months of follow-up, the patient walks with a slight limp due to a residual shortening of 1.5 cm (Fig. 6), but without pain, correct femoral anteversion, and full range of motion. The evaluation with the Harris scale showed a score of 98.
The anteroposterior pelvis radiograph showed an adequate post-operative result without observing osteolysis lines or loosening of prosthetic components (Fig. 7).
Finally, the patient is currently incorporated into his daily living and work activities without any limitations (Fig. 8).
Osteochondroma is the most common benign tumor bone lesion, usually located in the metaphysis of long bones. Frequently, it appears as a solitary lesion; only 15% of cases present as multiple lesions [2]. Clinical presentation in the hip is rare and may present as solitary lesions in the proximal femur; even less common is the location in the acetabulum [12, 13]. An osteochondroma involving the hip joint, diagnosed at an early stage, can be treated with various resection methods [6, 7]. In young patients like the one we present in this report, the association of joint degeneration is a finding that carries the possible need for total joint replacement as a primary treatment option [8]. In the patient, we present in this report, surgical resection was not considered the only treatment, given that the patient had osteoarthritis in the hip, as could be observed in the tomography study and the macroscopic characteristics of the acetabulum and femoral head. In 2020, the first series of cases of multiple osteochondroma in hips of patients with an average age of 53 years and treated with resection surgery and total joint replacement of the hip was published [9]. Before this study, there were few published case reports of patients treated with total hip replacement [14-16]. In the patient’s case, we report here that tumor resection and total hip replacement were carried out with a cemented femoral stem, a non-cemented acetabular cup, and a ceramic femoral head, showing a favorable evolution at 25 months of follow-up. Finally, today, there is no consensus on how to approach these intra-articular lesions. It is essential to consider the tumor’s specific characteristics, the surgeon’s experience, and the technological resources available as fundamental aspects of therapeutic decision-making.
Intra-articular hip osteochondroma diagnosed before joint wear requires resection through different surgical techniques. For young adult patients with intra-articular osteochondroma of the hip resulting in secondary osteoarthritis, total joint replacement should be considered as an effective method to relieve pain, restore function, and facilitate return to activities. Careful pre-operative planning is mandatory to minimize the probability of intraoperative or immediate post-operative complications.
Complete tumor resection, together with the placement of a total hip prosthesis, can be considered a valid and reliable option in the treatment of intra-articular hip osteochondroma that is associated with degenerative joint changes in young adult patients.
References
- 1.Calafiore F, Fidanza A, Venosa M, Fabiani R, Logroscino G. Hip joint osteochondroma treated with short stem total hip arthroplasty: A case report. Acta Biomed 2023;94:e2023188. [Google Scholar]
- 2.Nehme AH, Haidamous GF, Abdelnour HG, BouMounsif JN, Wehbe JW, Moucharafieh RC. Surgical hip dislocation for management of acetabular osteochondroma in an adult. Case Rep Orthop 2017;2017:8481563. [Google Scholar]
- 3.Tepelenis K, Papathanakos G, Kitsouli A, Troupis T, Barbouti A, Vlachos K, et al. Osteochondromas: An updated review of epidemiology, pathogenesis, clinical presentation, radiological features and treatment options. In vivo 2021;35:681-91. [Google Scholar]
- 4.Wang SI, Park EH, Yoon SJ, Kim JR. Intra articular osteochondroma of the posteroinferior femoral neck associated with hip joint osteochondromatosis: A case report. Mol Clin Oncol 2017;7:915-8. [Google Scholar]
- 5.Shah VI, Pachore JA, Mungra DL, Shetty GM, Patil J. Giant solitary acetabular osteochondroma with a 30-year-old neglected fracture neck femur treated with total hip arthroplasty: A case report. J Orthop Rep 2024;3:100313. [Google Scholar]
- 6.Bottner F, Rodl R, Kordish I, Winkelmann W, Gosheger G, Lindner N. Surgical treatment of symptomatic osteochondroma. A three-to eight-year follow-up study. J Bone Joint Surg Br 2003;85:1161-5. [Google Scholar]
- 7.Makhdom AM, Jiang F, Hamdy RC, Benaroch TE, Lavigne M, Saran N. Hip joint osteochondroma: Systematic review of the literature and report of three further cases. Adv Orthop 2014;2014:180254. [Google Scholar]
- 8.Fernández CA, Carril EC, Fernández AR, Huaraca CM, Cubells MM, Cisneros LG, et al. Arthroscopic treatment of a femoral osteochondroma as a cause of femoroacetabular impingement. Rev Esp Artrosc Cir Articul 2022;29:199-204. [Google Scholar]
- 9.Yoon JY, Park CW, Park YS, Yoo JJ, Kim HJ. Total hip arthroplasty for secondary coxarthrosis in patients with hereditary multiple exostoses: Minimum 5-year follow-up results and surgical considerations. Clin Orthop Surg 2020;12:435-41. [Google Scholar]
- 10.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 1969;51:737-55. [Google Scholar]
- 11.Rosai J. Rosai and Ackerman’s Surgical Pathology E-Book. Amsterdam: Elsevier Health Sciences; 2011. [Google Scholar]
- 12.Garcia RJ, Takata ET, Alves MT, Pires OG, Basile R. Acetabular osteochondroma. Acta Ortop Bras 2005;13:93-4. [Google Scholar]
- 13.Vaishya R, Vijay V, Swami S, Vaish A. Isolated acetabular osteochondroma of the hip. Acta Orthop Traumatol Turc 2017;51:420-4. [Google Scholar]
- 14.Kim WJ, Park JS, Won SH, Lee HS, Lee DW, Jang BW, et al. Total hip arthroplasty in hereditary multiple exostoses with secondary osteoarthritis: A case report. Medicine 2019;98:e18175. [Google Scholar]
- 15.Santoso A, Utomo P, Im CJ, Park KS, Yoon TR. Minimally invasive total hip arthroplasty in a patient with hereditary multiple exostoses: A case report. Malays Orthop J 2018;12:53-6. [Google Scholar]
- 16.Kanda A, Kaneko K, Obayashi O, Mogami A. Total hip arthroplasty using a polished tapered cemented stem in hereditary multiple exostosis. Case Rep Orthop 2016;2016:4279060. [Google Scholar]