Difficult open comminuted fracture of distal femur complicated by infection, gap non-union, and extension contracture can be managed with a combination of induced membrane technique with LRS and later on non-vascularized fibula strut graft with plating for a favorable outcome.
Dr. Ganesh R Shetty, Department of Orthopaedics, Dr. Muthus Hospital, Near Jai Shanthi Theatre, Trichy Road, Singanallur, Coimbatore, Tamil Nadu, India. E-mail: drgs701@hotmail.com
Introduction: Distal femur fractures are high-velocity injuries which accounts for 7–10% of all femoral fractures of which 5–10% are open fractures. Despite advances in techniques and implants, treatment remains a challenge, in many situations due to increased risk of infection, non-union and loss of range of motion. Surgical management of such complex injury includes radical debridement with stabilization followed by management of gap non-union with appropriate techniques and restores the range of motion.
Case Report: We present a case of 20-year-old man who had suffered multiple orthopedic trauma following accident. The patient had open comminuted fracture of the right distal femur, closed fracture of the same side tibia shaft, and right side closed both bone forearm shaft fracture. The patient was initially treated with debridement and knee-spanning limb reconstruction system (LRS). The patient developed infection and subsequently osteomyelitis of the distal femur shaft and gap non-union of 8 cm. The patient was operated for two-stage-induced membrane technique (IMT) and bone grafting using LRS followed by non-vascularized fibula strut grafting and plating. Quadriceps contracture was later on treated with quadricepsplasty to get good functional and radiological outcome.
Conclusion: A case of open distal femur comminuted fracture with a very small distal fragment complicated with osteomyelitis and gap non-union. We have shown that the use of IMT followed by non-vascularized fibula strut grafting and plating along with quadricepsplasty can give a very good outcome.
Keywords: Gap non-union, induced membrane technique, limb reconstruction system.
Distal femur fracture is usually associated with high-energy injuries and accounts for 5–10% of all open injuries [1]. It becomes challenging when the distal fragment is very short with inadequate bone stock for a stable internal fixation. Problems are further compounded due to infection leading to osteomyelitis and gap non-union. The current recommended treatment for gap non-union includes distraction osteogenesis (DO), vascularized fibular strut graft, and induced membrane technique (IMT). DO with an external fixator takes a long time for healing with reduced patient (PT) compliance. Vascularized fibular strut graft (vascularized bone transfer [VBT]) is technically demanding and resource intensive [2]. IMT was initially described as bone loss resulting from septic non-union of the leg [3]. Masquelet and Begue described a two-stage IMT for the reconstruction of larger defects (5–18 cm) with satisfactory results [4]. However, IMT has a failure rate of 18% leading to additional union procedure. After these, the overall failure rate is 10.3% [5]. We Demonstrate a case of open communicated fracture of distal femur complicated with osteomyelitis and gap non-union, difficulties we faced in reconstruction using IMT requiring additional bone grafting procedure and quadricepsplasty to get a satisfactory outcome.
We report a case of 20-year-old male patient (PT) with an alleged history of road traffic accident presented with multiple musculoskeletal trauma presented to our casualty after 24 h of injury, initially treated elsewhere. Compound severely comminuted fracture with bone loss of right (RT) distal femur grade 3A (Gustilo-Anderson) AO/OTA C3, closed fracture of tibia shaft RT side AO/OTA B2 and closed fracture of both bone forearm shaft RT side AO/OTA B3 (Fig. 1a and b).
PT was adequately resuscitated and stabilized, and computed tomography scan was done to rule out other injuries. No neurovascular injuries were present in the fractured limbs. Through debridement was done with intramedullary wash and RT leg was stabilized with knee-spanning monorail fixator (limb reconstruction system [LRS]). Forearm fracture was fixed with dynamic compression plate (Fig. 2).
PT was not on regular follow-up and came with pus discharge after 1 month. Debridement was done, distal femur screw was removed, and culture appropriate antibiotics were given. PT did not turn up till after 2 months with osteomyelitis of the distal femur shaft (Fig. 3a).
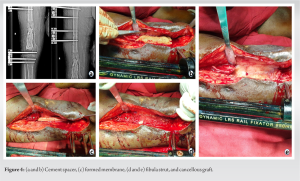
After through debridement, there was a gap of 8 cm in the distal femur (Fig. 3b). At this stage, we planned for two-staged IMT and the void was filled with antibiotic-loaded bone cement (Fig. 3c). As the distal femur segment was very small with inadequate bone stock, stability with internal fixation was doubtfull. Hence, we decided to continue with LRS fixation for the second stage of IMT. At 8 weeks, well-formed membrane was seen, which was incised cement block was removed (Fig. 4a, b, c). Cancellous bone graft (BG) was harvested from proximal tibia from opposite side. Fibula strut graft was kept inside for expanding the volume of BG and provide stability (Fig. 4d and e).
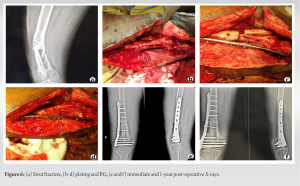
Four months post-bone BG, there was inadequate corticalization of the graft was noted, which was not enough for weight bearing (Fig. 5a and b). Tibia shaft fracture was united. We decided to remove the LRS and after 3 weeks planned for augmentation plating. Post-LRS removal PT had an accidental fall and fracture of the strut proximally (Fig. 6a). BG, fibula strut graft medially, and internal fixation with distal femur LCP were done (Fig. 6b, c, d). Immediate and 1-year post-operative X-rays (Fig. 6e and f).
PT was walking full weight bearing without any discomfort. However, he had severe extensor contracture with only 15 degree of knee flexion possible. Eighteen months after augmentation plating and BG Judet’s quadricepsplasty was done where a sequential release of the intrinsic and extrinsic contracture was done without any lengthening of the quadriceps. Intraoperative full range of motion was achieved (Fig. 7a and b). Three-month post-quadricepsplasty PT had an extensor lag of 30 degree with further flexion up to 110 degree (Fig. 7c, d, e). PT was walking comfortably without any discomfort.
Open fractures of the distal femur are at increased risk of complications such as infections, non-union, knee stiffness, and loss of range of motion [6]. Early through debridement is the key in preventing infection. Soft-tissue stripping, contamination, and altered vascular anatomy make it difficult for the host immune cells to reach the fracture site to deliver the antibiotics administered systemically [7]. Osteomyelitis leading to sequestration of the long segment of bone leads to gap non-union which poses a significant challenge when associated with short juxta-articular fragment. Traditional method of treatment of gap non-union includes allografts, DO, VBT, and IMT. Allografts can be used in large defects but they have a higher rate of complications [8]. Donati et al. reported 35% non-union, 16.4% graft fracture, and 5.4% infection in their series of 128 patients with massive allografts [9]. DO has given satisfactory results; however, the treatment course is long, with PT dissatisfaction with the external fixator, functional limitation with daily activities, and pin tract infections. VBT requires microsurgical skills, which are technically demanding and not available at every hospital [10]. Masquelet first described this technique in 1980s and subsequently many authors have used this technique to reconstruction of critical bone defect (5–25 cm) with satisfactory results [2, 4, 11]. The cement spacer used in IMT prevents fibrous tissue invasion at the recipient site and provides mechanical stability to the construct and antibiotic-loaded bone cement prevents bacterial adhesions when there is a high risk of infection [11, 12]. The membrane induced is the key to IMT success without which BG in a gap larger than 4–6 cm will be resorbed [2, 13, 14]. In our case, we decided to go for IMT due to the large gap non-union due to osteomyelitis. Most of the recent literature favor internal fixation during the second stage of IMT as the use of an external fixator through the second stage has increased the risk of stress fracture and infection [15]. In our case, we continued with knee-spanning LRS in the second stage of IMT as the as the distal fragment was very short with inadequate bone stock for rigid internal fixation. However, in our case, there was inadequate corticalization of the graft. Masquelet pointed out the need of very rigid fixation after the second stage to promote revascularization of the graft and more flexible later to enhance corticalization [3]. In our case, the use of LRS in the second stage which provides relative stability may have led to poor corticalization of the graft which needs to be collaborated with further studies. Nevertheless, IMT helped in building the bone stock in the distal femur which helped us in augmentation plating subsequently. Post-infection and knee-spanning LRS knee joint invariably becomes stiff. Providing functional range of motion is important for the PT to continue his activity of daily living unhindered. In our case, we did Judet’s quadricepsplasty where sequential release was done without any lengthening of the quadriceps to get functional range of motion for a good outcome.
IMT is a very simple and cost-effective way of treating gap non-union PT following infection. Time taken to heal is irrespective of the length of the gap union as compared to DO. It is very much cost effective as compared to vascularized fibula graft which is technically demanding too. IMT is not without its caveats and may not give the desired results when all the principles are not followed. Risk of additional procedures to get a complete union must be kept in mind while planning for big gap non-union surgery.
Through meticulous debridement is the first step in the management of any open fracture. Infected gap non-union is a nightmare for both surgeon and PT. In reconstructive surgeries for massive gap non-union, PT must be counseled in-depth about the lengthy and staged procedures as his compliance is of paramount importance for a successful outcome. IMT is a simple, less demanding cost-effective technique for the management of gap non-union. In our case, we used IMT with knee-spanning LRS continued through the second stage to manage the gap non-union which significantly reduced the void and aided in subsequent plating of distal femur. Post-traumatic stiff knee can be managed with judet’s quadricepsplasty to provide good functional outcome.
References
- 1.Reátiga J, Arzuza L, Guzmán J, Molina J, Ríos X. Fibular strut graft placement for an open distal femur fracture with a critical bone defect: A case report. Trauma Case Rep 2022;42:100712. [Google Scholar]
- 2.Musa RA, Shah DU, Makwana VR, Hadiya AK, Shah PK, Bhavsar NM. Masquelet’s induced membrane technique for the reconstruction of post-traumatic, open-grade distal femur fracture with bone defect. J Orthop Trauma Rehabil 2021;. https://doi.org/10.1177/2210491721992 [Google Scholar]
- 3.Masquelet AC. Induced membrane technique: Pearls and pitfalls. J Orthop Trauma 2017;31:S36-8. [Google Scholar]
- 4.Masquelet AC, Begue T. The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am 2010;41:27-37; table of contents. [Google Scholar]
- 5.Morelli I, Drago L, George DA, Gallazzi E, Scarponi S, Romanò CL. Masquelet technique: Myth or reality? A systematic review and meta-analysis. Injury 2016;47:S68-76. [Google Scholar]
- 6.Kumar MD, Singh R, Khiyani R, Kaur K, Svareen. Evaluation of results of open distal femur fractures with primary fixation and antibiotic impregnated collagen. Chin J Traumatol 2019;22:328-32. [Google Scholar]
- 7.Mukhopadhaya J, Jain AK. AO principles of fracture management. Indian J Orthop 2019;53:217-8. [Google Scholar]
- 8.Gannamani S, Rachakonda KR, Tellakula Y, Takkalapally H, Maryada VR, Gurava Reddy AV. Combining non-vascularized fibula and cancellous graft in the masquelet technique: A promising approach to distal femur compound fracture management with large defects. Injury 2024;55:111233. [Google Scholar]
- 9.Donati D, Di Bella C, Colangeli M, Bianchi G, Mercuri M. The use of massive bone allografts in bone tumour surgery of the limb. Curr Orthop 2005;19:393-9. [Google Scholar]
- 10.Hsu CA, Chen SH, Chan SY, Yu YH. The induced membrane technique for the management of segmental tibial defect or nonunion: A systematic review and meta-analysis. Biomed Res Int 2020;2020:5893642. [Google Scholar]
- 11.Giannoudis PV, Faour O, Goff T, Kanakaris N, Dimitriou R. Masquelet technique for the treatment of bone defects: Tips-tricks and future directions. Injury 2011;42:591-8. [Google Scholar]
- 12.Azi ML, Teixeira AA, Cotias RB, Joeris A, Kfuri M. Induced-membrane technique in the management of posttraumatic bone defects. JBJS Essent Surg Tech 2019;9:e22. Erratum in: JBJS Essent Surg Tech 2020;10:e0099ER. [Google Scholar]
- 13.Alford AI, Nicolaou D, Hake M, McBride-Gagyi S. Masquelet’s induced membrane technique: Review of current concepts and future directions. J Orthop Res 2021;39:707-18. [Google Scholar]
- 14.Wang P, Wu Y, Rui Y, Wang J, Liu J, Ma Y. Masquelet technique for reconstructing bone defects in open lower limb fracture: Analysis of the relationship between bone defect and bone graft. Injury 2021;52:988-95. [Google Scholar]
- 15.Sun SH, Tsai WW, Shiu SI, Chen CH. Induced membrane technique for large bone defects: A systematic review and individual participant data meta-analysis. Medicine (Baltimore) 2022;101:e29292. [Google Scholar]