Neglected anterior dislocation of the hip is a rare finding that may require total hip arthroplasty when the joint is not salvageable although hip arthrodesis and Girdlestone resection can be alternative treatment.
Dr. Mantu Jain, Department of Orthopaedics, All India Institute of Medical Sciences, Bhubaneswar - 751 019, Odisha, India. E-mail: montu_jn@yahoo.com
Introduction: Traumatic hip dislocations frequently result from road traffic accidents and are prevalent in developing nations. Untreated dislocations either due to ignorance or lack of proper treatment become more challenging to manage and have an increased likelihood of developing avascular necrosis (AVN). Over time, closed methods of reduction become impractical, and if the waiting period surpasses 3 months, open reduction likewise becomes unworkable. Anterior dislocations are less common than posterior dislocations, accounting for a frequency of 7–13% of all hip dislocations. Neglected anterior hip dislocations are extremely rare, and therefore, there is a paucity of information about the management of these dislocations and associated injuries. The available treatment options for these particular situations are total hip arthroplasty (THA), Girdlestone surgery, or hip arthrodesis.
Case Report: We describe the case of a 49-year-old male who presented to our hospital with a neglected anterior dislocation of the hip. The patient disclosed a history of hip trauma 8 months ago, initially receiving conservative management. However, due to persistent pain and functional limitations, he sought further medical attention. A physical examination, radiographic evaluation, and computed tomography (CT) scan confirmed the diagnosis. The patient underwent THA using dual anterior and posterior approaches, followed by a comprehensive rehabilitation program.
Conclusion: Anterior dislocation of the hip is a relatively rare condition, and its neglected presentation is even rarer. This case highlights the importance of prompt diagnosis and early intervention in neglected anterior hip dislocations to minimize complications and optimize patient outcomes.
Keywords: Neglected, Anterior dislocation, Total hip arthroplasty
Traumatic hip dislocations are often caused by road traffic accidents (high-energy trauma) and are common in developing countries [1]. Researchers describe the golden period for reduction as occurring within 6 h of injury to prevent future complications [2]. However, these traumas often coexist with multiple injuries, which divert attention from the dislocation. Neglecting such injuries increases their difficulty in treatment and increases the risk of developing AVN. Closed reduction techniques become unfeasible as time passes, and if the wait exceeds 3 months, open reduction also ceases to be viable [1,3]. The potential options for these types of cases are total hip arthroplasty (THA), Girdlestone procedures, or hip arthrodesis [3,4]. Trauma-induced hip dislocations fall into different categories based on their direction. Anterior dislocations are significantly less common than posterior dislocations and account for 7%–13% of all hip dislocations [5]. Reports of chronic traumatic anterior hip dislocation are extremely rare, further subdivided into superior (pubic) types and inferior (obturator) varieties, accounting for only 4% [6]. Reports indicate that injuries associated with anterior hip dislocation, such as impaction fractures of the femoral head, occur at frequencies ranging from 15% to 35% [7]. On the other hand, fractures of the acetabulum are less common, occurring in only 4% of cases [8]. Neglected anterior-type dislocations are extremely rare and occur in acute settings where immediate orthopedic assistance is unavailable, particularly in rural areas. In developing countries, it is common for patients to seek alternate therapies before eventually arriving at hospitals after a prolonged period of trauma, which poses challenges in managing such cases as time progresses.
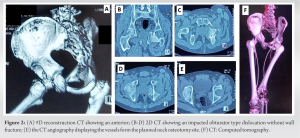
A 49-year-old male presented to our hospital with complaints of persistent left hip pain and an inability to bear weight on the affected leg. The patient reported a history of trauma to the hip region approximately 5 months ago, following a road traffic accident. Initially, he sought some indigenous treatment and received advice on conservative management, which included pain medication and rest. Despite the initial conservative treatment, the patient continued to experience severe pain and limited mobility. He reported having difficulty walking, standing, and performing routines daily. On physical examination, we found the left lower limb externally rotated and fixed in flexion (Fig. 1a). There was tenderness over the anterior aspect of the hip joint, and any attempt at passive movement caused severe pain.

Radiographic evaluation, including anteroposterior views of the pelvis, revealed an anterior dislocation of the left hip joint (Fig. 1b). We performed a computed tomography (CT) scan to assess the extent of the bony injury and aid in surgical planning. The CT scan showed that the patient had an anterior hip dislocation of the obturator type, along with inferior acetabular rim fractures (Fig. 2). There was an impaction fracture in the femoral head, as well as a deformity in the femoral head hinging under the inferior acetabular labarum.
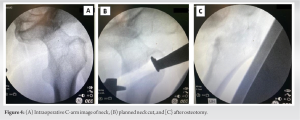
After obtaining informed consent, the patient underwent THA of the left hip joint. We used a Smith-Petersen approach in the supine position under spinal anesthesia to access the hip joint (Fig. 3). We exposed the femur’s neck and cut it for a hip arthroplasty (Fig. 4). Next, we positioned the patient laterally and initiated the acetabular preparation using the posterior approach. We removed the dense fibrous tissue covering the acetabulum and surrounding labrum. Next, we proceeded with serial reaming to reveal the bleeding cancellous bone, after which we positioned and secured an acetabulum shell of the appropriate size using three screws. A polyethylene liner was placed and locked. A non-cemented stem was fixed in the femur after serial broaching. The hip joint was reduced, and stability was checked throughout the range of motion and found satisfactory. The wound was thoroughly washed and closed in layers.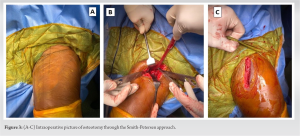
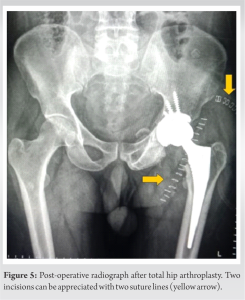
The patient was on immobilization with an abduction brace for 2 weeks postoperatively to facilitate the healing of the soft-tissues surrounding the hip joint. After 2 weeks, we removed the sutures and initiated a comprehensive rehabilitation program for the patient, which included range-of-motion exercises and gradual weight-bearing as tolerated. Physical therapy sessions were conducted to improve muscle strength, joint stability, and functional independence. Post-operative radiograph was satisfactory (Fig. 5).
At the 1-year follow-up, the patient reported significant improvement with good functional outcomes (Harris hip score of 83). The patient regained a near-normal range of motion and was able to walk without support, although with a slight limp.
Anterior traumatic hip dislocations are relatively less common than posterior dislocations. Information regarding these dislocations and their associated injuries is scarce. Consequently, there is a limited availability of recommendations regarding the suitable treatment approach for these fractures (operative versus non-operative) [9]. The unreduced obturator variety of anterior hip dislocation is an uncommon occurrence. Early diagnosis can effectively manage the dislocation through closed reduction and immobilization, leading to satisfactory outcomes [10]. However, the surgeon has few options if there is a delay of more than 3 months. The time between injury and reduction strongly influences the occurrence of femoral head necrosis. Failure to perform reduction within 6 h after the injury can lead to a 50% incidence of femoral head necrosis [11]. Researchers have observed impaction defects at varying frequencies, from 15% to 35%, and have linked them to a higher incidence of post-traumatic hip osteoarthritis [12]. While THA is considered a viable treatment option in such situations, certain authors have mentioned alternative approaches such as subtrochanteric osteotomy, the Girdlestone procedure, hip arthrodesis, or hemiarthroplasty.
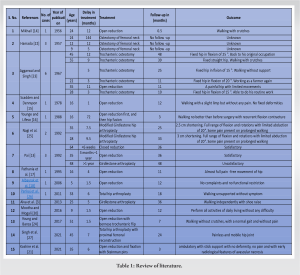
Closed reduction has been less commonly used compared to open reduction in cases of dislocations, mainly due to the increased difficulty of achieving reduction. Delays in receiving the appropriate treatment typically influence the success of the reduction process. Pai [13] documented three cases of neglected anterior dislocations, but they did not specify if any of these cases included obturator dislocations. In only one of these cases, closed reduction was successful, with neglect lasting <3 weeks. The first ever reported case of neglected anterior dislocation of the hip was by Mikhail in 1956, where they used open reduction to manage a 1-year-old dislocation [14]. Although they were able to achieve hip reduction, they did not report any long-term functional results. Seven cases of old obturator dislocations that had not been reduced were studied by Scadden and Dennyson [15], Younge and Lifeso [16], Pathania et al. [17], Albayrak et al. [18], Li et al. [19], Mootha AK et al. [20], and Koshire et al. [21]. All of them were treated with open reduction. Among these patients, three showed substantial improvement and were able to perform routine work without pain. Two patients achieved relatively satisfactory results with a slight limp and some pain; one patient had a poor outcome and required hip fusion; and one patient developed AVN, necessitating THA at a later date. Hamada [22] reported in 1957 that they managed four cases with a simple corrective osteotomy to improve limb functioning. Aggarwal and Singh (1967) documented six anterior obturator dislocations, treating them with trochanteric osteotomy in five cases and open reduction in one [23]. All patients had poor outcomes, including hip flexion deformities and restricted mobility. Young and Banza used Bernese trochanteric flip osteotomy in a 6-week-old neglected anterior dislocation and reported fair outcomes [24]. Nagi et al. [25] documented two cases of unreduced obturator dislocations, in which the patients underwent a modified Girdlestone arthroplasty. To preserve the option of a THA in the future, if necessary, the procedure involved a subcapital osteotomy. Following the surgery, both patients exhibited shortened legs but showed a complete range of motion in rotation and flexion, although with restricted abduction capabilities. In their study, Alva et al. (2013) presented a case of a 5-month-old neglected anterior dislocation of the hip in a 25-year-old man [3]. Pre-operative MRI scanning detected AVN. To address the condition, they opted for a modified Girdlestone procedure following the technique described by Nagi et al. [25]. Over a 3-year period, they assessed the patient’s progress and found a “fairly stable hip” with only 2.5 cm of shortening [3]. Pankaj et al. managed a 33-year-old male patient with an unreduced obturator dislocated hip, who had experienced a deformity in his right hip due to a road traffic accident 6 months earlier, by THA [26]. Singh et al. [27] conducted a study where they reported a 45-year-old male patient who had an anterior hip dislocation and a pertrochanteric femoral fracture, both of which had gone untreated for 7 months. The management involved THA and proximal femoral reconstruction. After a follow-up period of 2 years, the hip joint became painless and mobile, indicating the success of the procedure. Anterior hip dislocations are associated with other hip injuries such as femoral head impaction fractures or acetabulum fractures, which can contribute to the development of post-traumatic hip osteoarthritis. The dislocation event may compress the femoral head against the anterior acetabular rim, leading to impaction defects within the femoral head or an avulsion or fracture of the anterior acetabular rim or wall. Studies have particularly reported severe osteoarthritic changes and unfavorable clinical outcomes in patients with impaction fractures deeper than 4 mm [28]. Tehranzadeh et al. [29] investigated the osteochondral impaction of the femoral head in dislocations using CT scans on a group of 35 patients. The study revealed that 67% of posterior dislocations and 100% of anterior dislocations showed femoral head impaction. In cases of anterior dislocation, the femoral head impaction occurred in the posterosuperior and lateral regions of the femoral head. This impaction bears a resemblance to Hillsach’s shoulder lesion. In addition, Dussault et al. [30] observed that contact against the anteroinferior margin of the acetabular rim caused the impaction of the femoral head in obturator dislocations. Table 1 provides the details of the literature review. Patients with good outcomes had a relatively short neglect time, lasting up to 6 months. On the other hand, those with fair or poor outcomes had considerably longer neglect times. This is consistent with other studies’ findings, which emphasize the critical role of neglect time as a prognostic factor in these cases. When the neglect extends beyond 3 months, as was the case in our situation with approximately 6 months of neglect, open reduction becomes a challenging option. Since our patient was middle age, wanted a painless, mobile, and stable hip, and there were no economic constraints, we decided to go for THA. In our case, the impaction involved the entire superolateral half of the femoral head, indicating that the inferior margin of the acetabulum was the cause of the impingement. The femoral head was hinging under the inferior acetabular labrum, and we expected difficulty in dislocating the hip joint. Therefore, we decided to use the anterior Smith-Petersen approach to open the hip joint and perform a neck cut. We decided to leave the head in its original position because the neck lodged very close to the femoral vessels. We, then, performed THA using the posterior approach.
The approach to treating delayed, unreduced anterior obturator dislocation has been somewhat empirical, but no definitively superior method has been proven. However, in the case of our patient, we highly recommend THA based on the increased risk of further complications, such as AVN, particularly in conjunction with an indentation fracture of the femoral head. THA is considered a suitable option to address these issues and improve the patient’s overall outcome. While THA is a favorable option in current medical practice, previously described treatment methods such as trochanteric osteotomy and the modified Girdlestone procedure remain relevant in situations where access to expert medical care may be limited. In addition, these methods may be considered when dealing with sedentary patients who choose to undergo THA at a later time.
A neglected anterior dislocation of the hip is a rare presentation. One can attempt an open reduction before the onset of AVN in the early period. However, neglect for longer periods and those associated with head or acetabular fractures warrant further procedures such as Girdlestone arthroplasty, arthrodesis, or THA.
References
- 1.Kumar S, Dahuja A, Narula MS, Garg S, Kaur R. Neglected hip dislocation: An unusual presentation, its management and review of the literature. Strategies Trauma Limb Reconstr 2017;12:189-92. [Google Scholar | PubMed]
- 2.Jain M, Swaroop S, Doki SK. Neglected posterior hip dislocation in adults presenting after one year managed successfully with single stage total hip arthroplasty: A case series. J Orthop Case Rep 2021;11:84-8. [Google Scholar | PubMed]
- 3.Alva A, Shetty M, Kumar V. Old unreduced traumatic anterior dislocation of the hip. BMJ Case Rep 2013;2013:bcr2012008068. [Google Scholar | PubMed]
- 4.Garrett JC, Epstein HC, Harris WH, Harvey JP Jr., Nickel VL. Treatment of unreduced traumatic posterior dislocations of the hip. J Bone Joint Surg Am 1979;61:2-6. [Google Scholar | PubMed]
- 5.El Masry AM. Anterior hip dislocation with ipsilateral displaced fracture neck of femur treated by open reduction and internal fixation: Case report and review of the literature. Strategies Trauma Limb Reconstr 2017;12:205-10. [Google Scholar | PubMed]
- 6.Hani R, Kharmaz M, Berrada MS. Traumatic obturator dislocation of the hip joint: A case report and review of the literature. Pan Afr Med J 2015;21:55. [Google Scholar | PubMed]
- 7.Erb RE, Steele JR, Nance EP Jr., Edwards JR. Traumatic anterior dislocation of the hip: Spectrum of plain film and CT findings. AJR Am J Roentgenol 1995;165:1215-9. [Google Scholar | PubMed]
- 8.Epstein HC, Harvey JP Jr. Traumatic anterior dislocation of the hip, management and results - An analysis of fifty-five cases. J Bone Joint Surg Am 1972;43-A:1561-2. [Google Scholar | PubMed]
- 9.Sahin V, Karakas ES, Aksu S, Atlihan D, Turk CY, Halici M. Traumatic dislocation and fracture-dislocation of the hip: A long-term follow-up study. J Trauma 2003;54:520-9. [Google Scholar | PubMed]
- 10.Gokulprasath S, Tarun Prashanth K. Anterior hip dislocation with ipsilateral subtrochanteric femur fracture in a young adult - a rare case report. J Orthop Case Rep 2020;10:63-6. [Google Scholar | PubMed]
- 11.Tekin AÇ, Çabuk H, Büyükkurt CD, Dedeoğlu SS, İmren Y, Gürbüz H. Inferior hip dislocation after falling from height: A case report. Int J Surg Case Rep 2016;22:62-5. [Google Scholar | PubMed]
- 12.Epstein HC. Traumatic dislocations of the hip. Clin Orthop Relat Res 1973;92:116-42. [Google Scholar | PubMed]
- 13.Pai VS. The management of unreduced traumatic dislocation of the hip in developing countries. Int Orthop 1992;16:136-9. [Google Scholar | PubMed]
- 14.Mikhail IK. Unreduced traumatic dislocation of the hip. J Bone Joint Surg Br 1956;38-B:899-901. [Google Scholar | PubMed]
- 15.Scadden WJ, Dennyson WG. Unreduced obturator dislocation of the hip. A case report. S Afr Med J 1978;53:601-2. [Google Scholar | PubMed]
- 16.Younge D, Lifeso R. Unreduced anterior dislocation of the hip in a child. J Pediatr Orthop 1988;8:478-80. [Google Scholar | PubMed]
- 17.Pathania VP, Kumar A, Ghosh D. Unreduced anterior dislocation of the hip: A case report. Med J Armed Forces India 1995;51:72-3. [Google Scholar | PubMed]
- 18.Albayrak M, Doğan A, Sürel YB. Traumatic obturator hip dislocation in a five-year-old boy: Open reduction after a six-week delay in diagnosis. Acta Orthop Traumatol Turc 2006;40:260-3. [Google Scholar | PubMed]
- 19.Li WZ, Wang JJ, Ni JD, Song DY, Ding ML, Huang J, et al. Old unreduced obturator dislocation of the hip: A case report. World J Clin Cases 2021;9:3979-87. [Google Scholar | PubMed]
- 20.Mootha AK, Mogali KV. A rare case of neglected traumatic anterior dislocation of hip in a child. J Orthop Case Rep 2016;6:40-2. [Google Scholar | PubMed]
- 21.Koshire SR, Koshire RR, Jain S. A 6-month-old neglected obturator inferior variety of anterior hip dislocation in a young male managed with an intermediary salvage measure without the need for osteotomy or excision arthroplasty with a resultant ambulatory natural hip a case report. J Orthop Case Rep 2021;11:57-60. [Google Scholar | PubMed]
- 22.Hamada G. Unreduced anterior dislocation of the hip. J Bone Joint Surg Br 1957;39-B:471-6. [Google Scholar | PubMed]
- 23.Aggarwal ND, Singh H. Unreduced anterior dislocation of the hip. Report of seven cases. J Bone Joint Surg Br 1967;49:288-92. [Google Scholar | PubMed]
- 24.Young S, Banza L. Neglected traumatic anterior dislocation of the hip. Open reduction using the Bernese trochanter flip approach - a case report. Acta Orthop 2017;88:348-50. [Google Scholar | PubMed]
- 25.Nagi ON, Dhillon MS, Gill SS. Chronically unreduced traumatic anterior dislocation of the hip: A report of four cases. J Orthop Trauma 1992;6:433-6. [Google Scholar | PubMed]
- 26.Pankaj A, Sharma M, Kochar V, Naik VA. Neglected, locked, obturator type of inferior hip dislocation treated by total hip arthroplasty. Arch Orthop Trauma Surg 2011;131:443-6. [Google Scholar | PubMed]
- 27.Singh A, Kumar P, Singh S, Singh RN, Telagareddy K. Primary complex total hip arthroplasty in neglected anterior hip dislocation with comminuted pertrochanteric femur fracture. Arthroplast Today 2021;10:63-7. [Google Scholar | PubMed]
- 28.DeLee JC, Evans JA, Thomas J. Anterior dislocation of the hip and associated femoral-head fractures. J Bone Joint Surg Am 1980;62:960-4. [Google Scholar | PubMed]
- 29.Tehranzadeh J, Vanarthos W, Pais MJ. Osteochondral impaction of the femoral head associated with hip dislocation: CT study in 35 patients. AJR Am J Roentgenol 1990;155:1049-52. [Google Scholar | PubMed]
- 30.Dussault RG, Beauregard G, Fauteaux P, Laurin C, Boisjoly A. Femoral head defect following anterior hip dislocation. Radiology 1980;135:627-9. [Google Scholar | PubMed]










