1. Prompt recognition and treatment of septic arthritis in neonates are crucial, involving surgical drainage, and antibiotics 2. Arthroscopic debridement is a promising alternative to open arthrotomy, requiring further research for optimal management.
Dr. Saurabh Suman, Department of Orthopaedics, Narayan Medical College and Hospital, Sasaram, Bihar, India. E-mail: saurabhsuman295@gmail.com
Introduction: Septic arthritis (SA) is the inflammation of the joints secondary to an infectious etiology, most commonly affecting the knee, hip, and shoulder. It is often an emergency condition and requires urgent intervention whether medical or surgical at the earliest. This case report highlights one such instance of timely intervention in a challenging scenario.
Case Report: In this case report, we encountered a 29-day-old female neonate born at 38 weeks and 4 days to a primigravida mother with a birth weight of 2.8 kg who was diagnosed with the right knee joint SA with neonatal sepsis. The neonate was also found to be suffering with acyanotic congenital heart disease. Early arthrotomy with exploration of joint with antibiotic cover was the chosen line of treatment.
Conclusion: Arthrotomy is a very good and established method to deal with SA. Early intervention is advised in these cases to ensure proper recovery without any complications.
Keywords: Septic arthritis, neonate, knee joint, arthrotomy.
Septic arthritis (SA) is the inflammation of the joints secondary to an infectious etiology, most commonly affecting the knee, hip, and shoulder. It may develop as a result of hematogenous seeding, direct introduction, or extension from a contiguous focus of infection. Acute SA in children is most often a hematogenous infection [1]. The sluggish blood flow in the metaphyseal capillaries makes growing bones susceptible to infection from hematogenous seeding from any trauma or infection [2]. Staphylococcus aureus and respiratory pathogens are the most common causative agents. In neonates, bacteria such as Escherichia coli are frequently encountered in the birth canal [3,4]. In this, there is irreversible cartilage damage in an involved joint caused by proteolytic enzymes released from inflammatory mediators (PMNs) [5]. It is diagnosed by the combination of radiological and biochemical investigations which include X-ray imaging, USG, magnetic resonance imaging (MRI), total counts, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) along with joint fluid aspirate which is considered as gold standard.
The patient is a 29-day-old female neonate born at 38 weeks and 4 days through full term vaginal delivery to a primigravida mother with a birth weight of 2.8 kg. The neonate had a history of initial episode of fever for 15 days for which she was treated elsewhere and medications administered. This was followed by pain and swelling of the right knee following which the patient was admitted in Narayan Medical College and Hospital, Sasaram. On examination, a painful tender knee joint was noted along with a swelling over the epigastric region of approximately 4 cm × 2 cm × 2 cm with distended bowel and murmur. Blood investigations revealed elevated total counts of 21300/cmm, ESR, and CRP of 70.4 mg/L. Radiological investigations in the form of X-ray showed edematous changes around the knee joint (Fig. 1) while ultrasonography of the right thigh revealed abscess formation of 4.0 × 3.4 × 3.0 cm, volume ~17 cc in the muscular layer of medial and lateral aspects of distal thigh. Contrast-enhanced MRI of the right knee joint was performed which was suggestive of SA with abscess formation involving the right knee joint and associated osteomyelitis of the right distal femoral metaphyses (Fig. 2). Simultaneous investigations were performed to evaluate the murmur; and a provisional diagnosis of acyanotic congenital heart disease (CHD) was made.
Considering all the above reports and facts, a diagnosis of SA of the right knee joint with neonatal sepsis and associated acyanotic CHD was made. As SA is a surgical emergency, the patient was planned for an arthrotomy of the right knee joint at the earliest along with exploration of the joint followed by administration of injectable antibiotics.
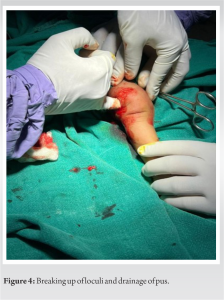
The patient was taken to the operation theater under general anesthesia and parts were thoroughly scrubbed, painted, and draped. Thereafter, an incision of approximately 2 cm was made over the lateral aspect of the knee joint over the most prominent area extending proximally. This incision was deepened to enter the muscular plane on which a sudden gush of the collected abscess was found to be pouring out (Fig. 3). This area was squeezed to excavate the all collections followed by breaking up of loculations using fingers and draining out the pus residue (Fig. 4). Thorough wash was given and then wound closed in layers along with the application of corrugated drain. This drain was removed after 48 h as the drainage was reduced.
The patient was kept on a combination of injectable antibiotics for 4 weeks followed by oral antibiotic cover for one and a half months and the situation of the disease assessed. On post-operative investigations, it was found that the total counts progressively reduced from initial values to 17,600/cmm and later to within the normal range. The CRP value also dropped down from pre-operative value of 70.4 mg/L to 24 mg/L in post-operative period. The general condition of the patient also improved significantly along with its movement at that particular joint.
At present, the patient has no complaints with respect to the right knee joint and has recovered fully. Her movements are also within normal range and no tenderness was noted. Furthermore, the patient’s knee joint showed no evidence of further damage due to SA.
SA poses a significant threat, especially in neonates, where the immune system is still developing and may not respond as vigorously to infection. Given the potential for rapid joint destruction and systemic spread of infection, SA is considered a medical emergency that requires immediate attention [5]. Conventionally, the mainstay of treatment for SA has been arthrotomy, a surgical procedure involving the open exploration and drainage of the affected joint. This approach allows for the direct visualization of the joint, enabling the surgeon to remove infected tissue and drain any accumulated pus or fluid. Alongside surgical intervention, broad-spectrum antibiotics are administered to combat the underlying infection [6]. Despite its effectiveness, arthrotomy has drawbacks, including increased risk of post-operative complications, longer recovery times, and potential damage to surrounding tissues. In recent years, arthroscopic debridement has emerged as a less invasive alternative. This technique involves making small incisions around the joint and inserting a tiny camera (arthroscope) and surgical instruments. The arthroscope provides a clear view of the joint interior, allowing for precise debridement of infected tissue and removal of debris without the need for a large incision. Studies comparing arthroscopic debridement to open arthrotomy have shown promising results. Böhler et al. and Acosta-Olivo et al. (2021) found that arthroscopic treatment resulted in shorter hospital stays, faster recovery times, and comparable rates of infection control compared to open surgery. In addition, arthroscopic debridement may offer better preservation of joint function and reduced risk of post-operative complications such as stiffness and scarring [7, 8]. While arthrotomy remains a viable treatment option for SA, arthroscopic debridement offers a minimally invasive alternative with comparable efficacy and potentially better outcomes in terms of recovery and joint function. Further research and clinical studies are warranted to establish the long-term benefits and optimal use of arthroscopic techniques in the management of SA [9,10].
Considering the scenarios and the current status with respect to the disease, open arthrotomy and exploration of the joint is still one of the best modalities in the treatment of SA of the joint. Early intervention and usage of broad-spectrum antibiotic coverage is another key point which helps in proper recovery and leads to reduced complications and sequelae of this disease. This topic further demands extensive research with a significantly larger population to come to a specific conclusion as to the efficacy of these methods.
This case report underscores the importance of early recognition and management of neonatal SA to prevent joint damage and systemic complications. Prompt diagnosis, aided by imaging and laboratory tests, is crucial. Surgical intervention, such as arthrotomy and joint exploration, alongside appropriate antibiotics, is vital for successful outcomes. While open arthrotomy has traditionally been favored, recent studies suggest that arthroscopic debridement may offer benefits. Multidisciplinary collaboration among orthopedic surgeons, pediatricians, and infectious disease specialists is essential. Further research comparing these approaches is warranted to optimize treatment strategies.
References
- 1.Shirtliff ME, Mader JT. Acute septic arthritis. Clin Microbiol Rev 2002;15:527-44. [Google Scholar]
- 2.Pääkkönen M. Septic arthritis in children: Diagnosis and treatment. Pediatric Health Med Ther 2017;8:65-8. [Google Scholar]
- 3.Agarwal A, Aggarwal AN. Bone and joint infections in children: Septic arthritis. Indian J Pediatr 2016;83:825-33. [Google Scholar]
- 4.Morrey BF, Bianco AJ Jr., Rhodes KH. Septic arthritis in children. Orthop Clin North Am 1975;6:923-34. [Google Scholar]
- 5.Wall C, Donnan L. Septic arthritis in children. Aust Fam Physician 2015;44:213-5. [Google Scholar]
- 6.Al Saadi MM, Al Zamil FA, Bokhary NA, Al Shamsan LA, Al Alola SA, Al Eissa YS. Acute septic arthritis in children. Pediatr Int 2009;51:377-80. [Google Scholar]
- 7.Böhler C, Dragana M, Puchner S, Windhager R, Holinka J. Treatment of septic arthritis of the knee: A comparison between arthroscopy and arthrotomy. Knee Surg Sports Traumatol Arthrosc 2016;24:3147-54. [Google Scholar]
- 8.Acosta-Olivo C, Vilchez-Cavazos F, Blazquez-Saldana J, Villarreal-Villarreal G, Pena-Martinez V, Simental-Mendia M. Comparison of open arthrotomy versus arthroscopic surgery for the treatment of septic arthritis in adults: A systematic review and meta-analysis. Int Orthop 2021;45:1947-59. [Google Scholar]
- 9.Montgomery NI, Epps HR. Pediatric septic arthritis. Orthop Clin North Am 2017;48:209-16. [Google Scholar]
- 10.Balabaud L, Gaudias J, Boeri C, Jenny JY, Kehr P. Results of treatment of septic knee arthritis: A retrospective series of 40 cases. Knee Surg Sports Traumatol Arthrosc 2007;15:387-92. [Google Scholar]