Antibiotic-impregnated cement rods with high-potency antibiotics like colistin for local delivery are very effective in resistant cases of long-standing infection. The author recommends extensive debridement with a repeat antibiotic cement rod if the infection is uncontrolled.
Dr. Sanket Tanpure, Department of Orthopaedics, New Thergaon Hospital, Pune, Maharashtra, India. E-mail: sankettanpure55@gmail.com
Introduction: Adult cases of septic arthritis due to concomitant persistent osteomyelitis are incredibly uncommon. This study describes a rare example of septic arthritis in an adult’s knee joint caused by long-term femur osteomyelitis. A cement rod laced with antibiotics proved to be an effective treatment for the illness.
Case Report: A case of septic knee arthritis caused by reactivated chronic osteomyelitis is described in this study. Initial radiographs revealed an osteolytic lesion, prompting further imaging, including a magnetic resonance imaging, which verified the diagnosis. To treat the infected intra-articular knee joint and ream the femoral intramedullary canal, we chose open debridement over arthroscopic surgery based on the patient’s history, physical examination, and imaging data. To close the dead space and remove the infection, a cement rod impregnated with antibiotics was placed into the medullary cavity, in addition to administering long-term antibiotic treatment. This approach was successful in eradicating the infection. Following a period of rehabilitation, the patient regained the ability to walk independently.
Conclusion: Cement rods infused with antibiotics are effective for delivering high doses of antibiotics locally while providing structural support to the bone. Over the last three decades, they have demonstrated encouraging outcomes in treating infections, and due to their affordability, simplicity, and effectiveness, they remain an excellent treatment option. Here, we highlight the use of colistin in making antibiotic-coated cement rods for the eradication of chronic, long-standing infection.
Keywords: Chronic osteomyelitis, septic arthritis, debridement, antibiotic therapy, antibiotic-impregnated cement rod.
Concomitant septic arthritis of the knee along with femoral osteomyelitis in adults is exceptionally rare, with only a few cases documented in the literature [1]. This condition is more frequently observed in pediatric patients [2]. Treatment can be particularly challenging if the surgeon is unaware of the simultaneous presence of both infections. Therefore, maintaining a high level of suspicion and a low threshold for advanced imaging is crucial for early diagnosis. However, in 1.7–7.8% of cases, the infection may persist despite treatment [3]. This persistence can occur if adjacent osteomyelitis is not identified and treated surgically at the time of the initial presentation, causing the joint to be repeatedly seeded with microorganisms. While septic arthritis with adjacent osteomyelitis is well-documented in pediatric patients, it has been rarely reported in adults [4]. This article describes a unique instance of adult septic arthritis in the knee joint caused by persistent femoral osteomyelitis, which was effectively resolved with the use of a cement rod impregnated with antibiotics. The case underscores the importance of maintaining a high index of suspicion, thoroughly understanding initial X-rays for early diagnosis, and performing extensive debridement with an antibiotic cement rod for local delivery of antibiotics.
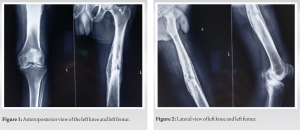
A 45-year-old man presented at our hospital with left knee symptoms that had developed over the course of 10 weeks and had become extremely painful and swollen for the past 5 days, without any apparent cause. The patient had a history of previous femur surgery, although details were unavailable. On presentation, the patient’s left knee exhibited noticeable edema, discomfort, and local warmth. The acute discomfort restricted the range of motion (ROM) of the knee joint to 30° of flexion. The patient appeared generally unwell and had a body temperature of 39°C. Laboratory findings revealed elevated white blood cell (13.5 × 109/L), C-reactive protein (CRP) (250 mg/L), and erythrocyte sedimentation rate (ESR) (72 mm/h). X-rays of the left knee and femur revealed a faint osteolytic lesion and sclerotic border along the intramedullary (IM) canal of the mid-shaft femur (Fig. 1 and 2), suggesting possible adjacent chronic osteomyelitis. This prompted a magnetic resonance imaging (MRI) analysis of the knee and femur, which showed septic arthritis of the knee and peripheral augmentation of granulation tissue in the medullary canal suggestive of chronic osteomyelitis, with no contact between the intra-articular region and the medullary cavity (Fig. 3).
We decided to treat the patient with surgical debridement of the intra-articular knee joint infection, IM reaming, and implantation of an antibiotic-coated cement rod. This approach aimed to address both the chronic osteomyelitis of the medullary canal and the septic arthritis of the knee. Extensive surgical debridement was performed to remove the infected granulation tissue surrounding the knee joint. Following the technique described by Shyam et al. [5], we prepared an antibiotic-impregnated cement rod. The distal end of a 2.5-mm flexible IM rod was twisted into a loop to facilitate retrieval. A mixture of 2 g vancomycin and 2.4 g tobramycin was added to the bone cement. The incisions were subsequently closed after the rod was placed into the medullary canal. Post-operative X-rays confirmed the satisfactory placement of the antibiotic-impregnated cement rod (Fig. 4). After a week of continuous passive motion machine treatment, knee flexion exercises, and limited weight bearing, the patient was discharged. Despite negative culture reports, the patient received intravenous antibiotics and underwent sequential evaluation of ESR.
One month after discharge, the patient returned for a follow-up visit, presenting with swelling over the distal third of the thigh and difficulty walking. He was readmitted to the hospital, where basic blood tests revealed elevated blood counts, ESR, and CRP, along with fever, suggesting uncontrolled infection. After obtaining informed consent, extensive surgical debridement was performed around the knee joint. The previous rod was removed under C-arm guidance, and a 2-mm flexible IM rod with its distal end twisted into a loop was used. A combination of 40 g of bone cement, 2 g of vancomycin, and 2 million IU of colistin was used to create antibiotic-impregnated bone cement. Two slices of bone cement, measuring 6 × 3 cm and 4 × 3 cm, were placed in the mid-thigh region after multiple lateral cortex drillings (Fig. 5). Intravenous colistin was administered under the guidance of a physician. Post-operative X-ray confirmed the placement of the antibiotic-impregnated cement rod with two slices of bone cement (Fig. 6). Two weeks after surgery, full weight bearing was permitted. Culture reports from specimens collected from the IM canal and joint synovium revealed Klebsiella, which was susceptible to vancomycin and colistin. The patient received intravenous antibiotics for 2 weeks before being discharged with a prescription for oral antibiotics for an additional 4 weeks, until inflammation markers, including ESR and CRP, returned to normal levels. The patient experienced immediate pain relief after surgery. The antibiotic-coated rod and bone cement slices were removed after 6 weeks.
At the 13-month follow-up, the patient remained pain-free, with a ROM of 0–100° and the ability to walk independently. ESR and CRP levels were within normal ranges, and there were no clinical signs of reinfection.
It is rare for individuals to have both femoral osteomyelitis and concurrent septic arthritis of the knee. Unfortunately, septic arthritis with adjacent osteomyelitis is frequently overlooked or takes longer to diagnose, particularly when radiographic evidence of osteomyelitis is weak or absent from the initial imaging. The early identification of this illness is further complicated by its rarity [4]. Even with appropriate surgical debridement and antibiotic therapy, failure to identify accompanying osteomyelitis can impede clinical results and result in joint reinfection [6]. Although several theories have been proposed, the precise etiology of this pathology remains unknown. These theories include contiguous spread, direct inoculation, and the dissemination of infection through a hematogenous pathway between the femoral metaphyseal and epiphyseal arteries [7]. Since there were no periarticular bone abnormalities in the distal femur on the initial MRI to imply direct connectivity between the knee joint and femur, as reported in a case by Jeong et al. [1], the underlying mechanism in the current case is more likely to be hematogenous spread. Intraoperatively, antibiotic rods can be fashioned using a variety of techniques, such as manually rolling cement [5], using commercially available molds, and utilizing a chest tube as a mold [8]. The manual rolling method, described by Shyam et al. [5], was employed in our cases, which involved manually rolling a 2.5 mm guide wire with an antibiotic cement mixture. Once the cement cooled, it formed a cylindrical antibiotic rod. The antibiotic rod can also be molded using a method described by Paley and Herzenberg [8]; however, they noted that extracting the chest tube from the cement rod can be challenging. In a comparative analysis of manufacturing methods, Kim et al. postulated that melting from the cement’s exothermic reaction is the cause of the chest tube’s difficulty in peeling. It is recommended to apply mineral oil to the chest tube’s interior before adding cement. In their study, the use of mineral oil reduced the peeling time to 7.5 min, which was 22.5 min faster than without it. In addition, cooling the chest tube in saline before peeling facilitated the process. The “twin Kocher peel technique,” involving two Kocher forceps placed perpendicularly at one end of the chest tube and rotated away, can make peeling more efficient and safer [9]. To further assist peeling, Mauffrey et al. recommended creating a 2 cm longitudinal incision at one end of the hollow chest tube during the initial step [10]. These procedures should be considered to ensure a smoother cement rod production process. IM infections resulting from tibia or femur fractures have been treated using an antibiotic-impregnated cement IM nail [11] or rod [8]. These rods fill gaps and provide high concentrations of certain antibiotics in the medullary canal. However, the durability of the cement and rod remains a major concern. Although not focusing specifically on IM infections, Capanna et al.’s [12] work sheds light on the lifespan of rods and cement. Following distal femur or proximal tibia tumor resection, 76 patients received an IM rod and cement spacer. During a 4.5-year follow-up, the researchers found that the implant outlived expectations, with only 12 cases (16%) of failure, including fractures, bending, or rod migration. Considering these findings, we deemed the application of the cement rod impregnated with antibiotics appropriate as it filled the empty space in the IM canal and delivered an adequate concentration of antibiotics. In the present case, the patient had a chronic infection that remained uncontrolled even after the initial antibiotic-coated cement rod and intravenous antibiotics. We carefully planned a surgical procedure that included burr-hole fenestration decompression of the lateral femoral cortex and thorough debridement to provide appropriate drainage. Following these procedures, the patient’s symptoms subsided over time, and the infections were completely eradicated.
It is rare for adults to have concomitant septic arthritis of the knee and femoral osteomyelitis. These cases underscore the importance of advanced imaging for timely diagnosis, which is crucial before proceeding with the extensive surgical debridement that is almost always required. Cement rods laced with antibiotics are useful for locally administering large doses of antibiotics while providing structural support to the bone. They have shown encouraging results in treating this ailment over the past 30 years, and due to their affordability, simplicity, and effectiveness, they continue to be an excellent treatment choice.
Septic arthritis of the knee with mid-shaft femur chronic osteomyelitis rarely occurs in the adult population. Early diagnosis, extensive debridement, local administration of antibiotics with bone cement, and long-term intravenous antibiotics are a key to eradicating infection.
References
- 1.Jeong WK, Park JH, Lee SH, Park JW, Han SB, Lee DH. Septic arthritis of the knee joint secondary to adjacent chronic osteomyelitis of the femur in an adult. Knee Surg Sports Traumatol Arthrosc 2010;18:790-3. [Google Scholar]
- 2.Goergens ED, McEvoy A, Watson M, Barrett IR. Acute osteomyelitis and septic arthritis in children. J Paediatr Child Health 2005;41:59-62. [Google Scholar]
- 3.Kaandorp CJ, Krijnen P, Moens HJ, Habbema JD, Van Schaardenburg D. The outcome of bacterial arthritis: A prospective community-based study. Arthritis Rheum 1997;40:884-92. [Google Scholar]
- 4.Marsh JL, Watson PA, Crouch CA. Septic arthritis caused by chronic osteomyelitis. Iowa Orthop J 1997;17:90-5. [Google Scholar]
- 5.Shyam AK, Sancheti PK, Patel SK, Rocha S, Pradhan C, Patil A. Use of antibiotic cement-impregnated intramedullary nail in treatment of infected non-union of long bones. Indian J Orthop 2009;43:396-402. [Google Scholar]
- 6.Zalavras CG, Dellamaggiora R, Patzakis MJ, Zachos V, Holtom PD. Recalcitrant septic knee arthritis due to adjacent osteomyelitis in adults. Clin Orthop Relat Res 2006;451:38-41. [Google Scholar]
- 7.Schmitt SK. Osteomyelitis. Infect Dis Clin North Am 2017;31:325-38. [Google Scholar]
- 8.Paley D, Herzenberg JE. Intramedullary infections treated with antibiotic cement rods: Preliminary results in nine cases. J Orthop Trauma 2002;16:723-9. [Google Scholar]
- 9.Kim JW, Cuellar DO, Hao J, Seligson D, Mauffrey C. Custom-made antibiotic cement nails: A comparative study of different fabrication techniques. Injury 2014;45:1179-84. [Google Scholar]
- 10.Mauffrey C, Chaus GW, Butler N, Young H. MR-compatible antibiotic interlocked nail fabrication for the management of long bone infections: First case report of a new technique. Patient Saf Surg 2014;8:14. [Google Scholar]
- 11.Thonse R, Conway J. Antibiotic cement-coated interlocking nail for the treatment of infected nonunions and segmental bone defects. J Orthop Trauma 2007;21:258-68. [Google Scholar]
- 12.Capanna R, Biagini R, Ruggieri P, Bettelli G, Casadei R, Campanacci M. Temporary resection-arthrodesis of the knee using an intramedullary rod and bone cement. Int Orthop 1989;13:253-8. [Google Scholar]