Yersinia enterocolitica prosthesis infections are of hematogenous origin with a digestive entry point, occurring as a result of gastrointestinal pathology. Although extremely rare, they must be treated with the greatest vigilance. Antibiotic therapy and removal of the prosthesis must be carried out because mortality is high.
Dr. Ramy Samargandi, Université de Tours-Faculty of Medicine, de Tours-CHRU Trousseau Service d’Orthopédie Traumatologie, 37170 Chambray-les-Tours, France/Department of Orthopedic Surgery, Faculty of Medicine, University of Jeddah, Jeddah, Saudi Arabia. E-mail: ramy.samargandi@hotmail.com
Introduction: Yersinia enterocolitica (is a gram-negative bacillus found in pigs and transmitted orally. It can contaminate a joint prosthesis following bacteremia. It is a potentially fatal and extremely rare infection, with fewer than 10 cases reported in the literature.
Case Report: This article describes two cases of patients who had a total hip arthroplasty infection, managed in our department. Both patients underwent emergency surgery for resection arthroplasty antibiotic therapy. Despite early management, both patients were died.
Conclusion: It is crucial to consider Yersinia infection in the context of prosthetic joint infection, even years after the operation, especially if it occurs following a digestive pathology. Rapid diagnosis and prompt initiation of appropriate management are essential.
Keywords: Prosthetic joint infection, hip arthroplasty, Yersinia enterocolitica, joint infection, postoperative complications.
Hip arthroplasty is a common and effective treatment for managing hip osteoarthritis. The 21st century has seen a significant increase in the number of hip prosthesis replacements. However, prosthetic joint infections (PJIs) remain to be a serious complication for patients and a nightmare for surgeons. The management of PJIs is multidisciplinary, involving both medical and surgical approaches. The incidence of PJIs is estimated to be between 1% and 2% for primary arthroplasties and between 3% and 10% for revision arthroplasties [1-5]. The most common microorganisms identified are Staphylococci (Staphylococcus aureus and Staphylococcus epidermidis, accounting for about 60% of cases), Streptococci (10%), and Enterococci (10%). Gram-negative bacilli account for <10% of cases [2, 6]. Prosthetic infections caused by Yersinia are extremely rare, with fewer than 10 cases described worldwide. Yersinia enterocolitica, a Gram-negative bacillus bacterium, has several serotypes, with O3 and O9 being the most common. It is typically acquired orally and affects the digestive tract. This bacterium is found in porcine species, and undercooked pork-based charcuterie is a significant source of infection. It mainly causes digestive symptoms such as gastroenteritis, terminal ileitis, or symptoms mimicking appendicitis. In rare cases, it can lead to septic arthritis, osteomyelitis, or post-infectious reactive arthritis [7]. In this report, we present two cases of hip PJI due to Y. enterocolitica and discuss a review of the literature.
Case 1
A 75-year-old man with a history of rheumatoid arthritis treated with Methotrexate and hypertension managed with antihypertensive medications had THA placed in 1997. Fifteen years later, in 2012, he underwent revision surgery for prosthesis loosening, which included a unipolar acetabular cup revision with an acetabular cage and allograft (Fig. 1a and b).
In November 2014, the patient was admitted to the hospital presenting with sepsis secondary to infectious diarrhea. Blood culture tests identified the causative agent as Y. enterocolitica. He was treated successfully with Cefotaxime and Gentamicin. Subsequent to his recovery from colitis, the patient was transferred to a rehabilitation center to continue his recovery. However, in February 2015, the patient was presented with hip pain and visible signs of inflammation around the scar of his left hip prosthesis, although he did not have a fever. At that time, he was able to ambulate with the aid of a crutch. Laboratory analyses revealed an inflammatory syndrome with a white blood cell count of 9.9 G/L, neutrophilic hyperpolynucleosis with PNN at 8.03 G/L (81%), and a C-reactive protein (CRP) level of 40.5 mg/L, indicating an active inflammatory process. Ultrasound imaging of the left hip revealed a deep collection measuring 7 × 1.5 × 3 cm. A computed tomography (CT) scan displayed a deep collection (size: 14 cm height, 11 cm width, 6 cm depth) in the left psoas muscle extending paravertebrally and in contact with the prosthesis, but no signs of prosthesis loosening were observed on the imaging studies (Fig. 1c and d). The patient was transferred to the orthopedic department, where he underwent surgical debridement, irrigation, and replacement of the mobile parts of the prosthesis through a posterolateral hip approach, along with an anterior iliac approach at the iliac crest to drain the intramuscular abscess around the psoas muscle. Postoperative empirical antibiotic therapy commenced with Tazocillin and Amikacin. Of the five intraoperative samples, only one tested positive for Y. enterocolitica. Following a multidisciplinary osteoarticular infection meeting, the antibiotic regimen was tailored to the identified pathogen, with Ciprofloxacin 750 mg administered twice daily for 6 weeks. Two weeks after surgery, the patient again showed signs of infection, both locally (wound dehiscence, purulent drainage, redness) and generally (fever of 38.8°C, increasing biological inflammatory syndrome. A new CT scan was requested, which revealed a significant periprosthetic collection. After further discussion with the infectious disease team and with the patient, it was decided to perform resection arthroplasty (Fig. 2). Treatment with Ciprofloxacin 750 mg twice daily was continued for another 6 weeks.
The post-operative follow-up was uncomplicated, with significant improvement of symptoms. He was discharged to a rehabilitation center 2 weeks later. At 2-month follow-up, Patients had no signs of infection. A progressive weight-bearing as tolerated was therefore decided and patient was able to walk around 20–30 steps using assistive walking device. The patient was died 3-month post-operatively under unknown circumstances.
Case 2
A 77-year-old man with a medical history of a pacemaker for atrial fibrillation, an abdominal aortic aneurysm, hypertension, and cemented THA on the left side in 1992 and on the right side in 2002 was on anticoagulant and antihypertensive medications. In September 2012, he presented to the emergency department with sudden onset left hip pain and functional impairment, with no history of falls. The left hip scar showed no signs of infection. He was febrile at 39°C and had inflammatory syndrome with leukocytes at 8 G/L and CRP at 280 mg/L. Urinary and blood cultures were negative. Radiographic X-rays of the pelvis and chest were normal. A pelvic CT scan showed no signs of loosening, osteolysis, or collection, and no extra-osteoarticular infectious cause was identified. A left hip aspiration under radiographic guidance yielded macroscopically purulent fluid. He was admitted to the orthopedic department and rapidly deteriorated into septic shock with respiratory distress 1 day after admission, with laboratory tests showing leukocytes at 15.8 G/L with 96% PNN, CRP at 331 mg/L, and hemoglobin at 13.6 g/dL. He was intubated and started empirical triple antibiotic therapy with Augmentin, Gentamicin, and Ofloxacin. An emergency debridement and irrigation were performed, revealing an abundant pus collection, and inflamed synovial tissues, with five culture samples taken. Due to prosthetic loosening, a total removal of the prosthesis (femoral stem, acetabular cup, and cement) was performed, and antibiotic therapy was switched to Vancomycin combined with an Aminoglycoside (Fig. 3).
Postoperatively, the left lower limb was placed in traction. All culture samples revealed the presence of YE. He was transferred to the surgical intensive care unit in septic shock. Upon arrival, the left popliteal pulse became unpalpable. An arterial Doppler ultrasound showed thrombosis of the left superficial femoral in the middle third and low permeability of the left iliofemoral. Vascular revascularization by embolectomy was organized, but he died from multi-organ failure the day after the vascular intervention.
PJIs remain a common complication that significantly affects patient outcomes, leading to major functional consequences and substantial economic impact [2]. In addition, it poses a difficult situation for surgeons regarding diagnosis and, crucially, treatment, particularly in choosing the appropriate therapeutic approach. The gold standard treatment for patients remains one-stage or two-stage prosthetic replacement. However, in cases where infection persists despite treatments, suppressive antibiotic therapy or resection is arthroplasty are indicated.
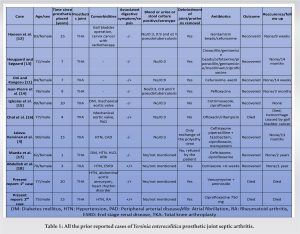
- enterocolitica is a well-known cause of reactive arthritis and is exceptionally a cause of septic arthritis. According to previous publications, nine cases of hip or knee prosthesis infection with Yersinia have been found. Furthermore, 36% of the report cases had a blood culture or urine culture or stool culture positive. However, a minority (2/11 cases) were presented with digestive symptoms in the weeks preceding the infection (Table 1). However, gastrointestinal disorders can be diverse and varied in intensity and duration, which could explain their reported low frequency. In our two cases, only case 1 presented a positive blood culture, he had also mentioned digestive problems in the weeks preceding his hospitalization. Prosthesis infections are most often early infections, occurring within 2 years after the intervention, of per-operative origin. Yersinia infections are late infections. Indeed, among the 8 patients (including our two patients presented here), the average latency between the intervention and infection was 10 years (ranging between 1 and 20 years). It might seem that the infection is not caused by per-operative contamination but is rather of hematogenous origin.
Concerning the physiology of Y. enterocolitica infection, after review of the literature, it appears that Y. enterocolitica infection has hematogenous origin. The entry point would be digestive, linked to a gastrointestinal pathology in the weeks preceding the infection of the material. This is what the following two studies report. Delaunay et al. [8] report the case of a 74-year-old patient presenting with an infection of an aortic bioprosthesis following infectious diarrhea with YE. She mentioned having eaten pork in the days preceding her infectious diarrhea. Giamarellou et al. [9] report the case of a 45-year-old patient with a mechanical mitral valve prosthesis that became infected with Y. enterocolitica within 3 months following appendicitis. Thus, according to previous scientific studies, infections of material with Y. enterocolitica are of hematogenous origin, with a digestive entry point.
- enterocolitica infection is a serious pathology, although rare, mortality is high. Concerning the proportion of deaths, from the nine cases that we found in the literature, only one died (mortality 11%), our two patients died (overall mortality 27%). However, this ratio of 27% is most likely underestimated because the average patient follow-up is <1 year. Indeed, of the nine studies mentioned, the average follow-up was 10 months, and one study did not specify the duration of follow-up.
Regarding the characteristics of the patients, the male/female ratio is 1:1 and the average age is 77 years (62–90). The proportion of THA compared to total knee arthroplasty (TKA) is 6 THA for 5 TKA. Apart from advanced age, the patients did not generally have any particular cause of immunosuppression. However, two patients had type II diabetes, one had rheumatoid arthritis treated with Methotrexate and another one had end stage renal disease. The characteristics of reported cases are summarized in Table 1. Iglesias et al. and Hougaard and Søgaard mention that Y. enterocolitica is a siderophore and that a high tissue concentration of iron would constitute a risk factor for infection. Tissue iron deposits can be caused by hemarthroses, common on knee prostheses, iron supplementation (in elderly and anemic patients), or the use of anticoagulants. Regarding the previous cases, some patients were taking anticoagulants or iron supplementation. Contrary to the literature, it does not appear that knee prostheses are riskier than hip prostheses. Simmonds et al. [10] have shown that patients with infectious diarrhea were 3 times more likely to have a positive stool culture for Y. enterocolitica than healthy subjects (4–5% versus 1.5%). Oni and Kangesu [11] then suggested treating all prosthetic carriers with infectious diarrhea and a positive stool culture for Y. enterocolitica with prophylactic antibiotic therapy.
We presented two case reports of patients who were treated at our center for a hip prosthesis infection caused by Y. enterocolitica, a very rare infection. The prosthesis had been in place for over 10 years. The existing prosthesis was removed, and the patients were placed on appropriate antibiotic therapy; however, they died as a result of this condition.
PJIs due to Y. enterocolitica infection is extremely rare, and it is crucial to consider Yersinia infection in the context of PJIs, especially if it occurs following a digestive pathology. Rapid diagnosis and prompt initiation of appropriate management are essential due to high mortality rate.
References
- 1.Chung AS, Niesen MC, Graber TJ, Schwartz AJ, Beauchamp CP, Clarke HD, et al. Two-stage debridement with prosthesis retention for acute periprosthetic joint infections. J Arthroplasty 2019;34:1207 13. [Google Scholar]
- 2.Lopez D, Leach I, Moore E, Norrish AR. Management of the infected total hip arthroplasty. Indian J Orthop 2017;51:397 404. [Google Scholar]
- 3.Del Pozo JL, Patel R. Clinical practice. Infection associated with prosthetic joints. N Engl J Med 2009;361:787 94. [Google Scholar]
- 4.Jalava-Karvinen P, Oksi J, Rantakokko-Jalava K, Virolainen P, Kotilainen P. Yersinia enterocolitica infection of a prosthetic knee joint. Case report and review of the literature on deep sited infections caused by Y. enterocolitica. Adv Infect Dis 2013;3:95 9. [Google Scholar]
- 5.Phillips JE, Crane TP, Noy M, Elliott TS, Grimer RJ. The incidence of deep prosthetic infections in a specialist orthopaedic hospital: A 15-year prospective survey. J Bone Joint Surg Br 2006;88:943 8. [Google Scholar]
- 6.Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev 2014;27:302 45. [Google Scholar]
- 7.Bottone EJ. Yersinia enterocolitica: The charisma continues. Clin Microbiol Rev 1997;10:257-76. [Google Scholar]
- 8.Delaunay M, Laterza F, Verdon R. Yersinia enterocolitica endocarditis on aortic bioprosthesis: A case report. IDCases 2022;30:e01617. [Google Scholar]
- 9.Giamarellou H, Antoniadou A, Kanavos K, Papaioannou C, Kanatakis S, Papadaki K. Yersinia enterocolitica endocarditis: Case report and literature review. Eur J Clin Microbiol Infect Dis 1995;14:126 30. [Google Scholar]
- 10.Simmonds SD, Noble MA, Freeman HJ. Gastrointestinal features of culture-positive Yersinia enterocolitica infection. Gastroenterology 1987;92:112 7. [Google Scholar]
- 11.Oni JA, Kangesu T. Yersinia enterocolitica infection of a prosthetic knee joint. Br J Clin Pract 1991;45:225. [Google Scholar]
- 12.Hansen W, El Doualy M, Putz P, Glupczynski Y. Infection de prothese de hanche a Yersinia enterocolitica. Méd Mal Infect 1989;19:459 61. [Google Scholar]
- 13.Hougaard K, Søgaard P. Yersinia enterocolitica coxitis after hip replacement. A case report. Acta Orthop Scand 1990;61:364 6. [Google Scholar]
- 14.Jean-Pierre H, Darbas H, Boyer G, Carriere C. Infection d’une prothèse de hanche à Yersinia enterocolitica : Deuxième cas. Méd Mal Infect 1992;22:941 2. [Google Scholar]
- 15.Iglesias L, García-Arenzana JM, Valiente A, Gomariz M, Pérez-Trallero E. Yersinia enterocolitica O:3 Infection of a prosthetic knee joint related to recurrent hemarthrosis. Scand J Infect Dis 2002;34:132 3. [Google Scholar]
- 16.Chol C, Blanc PL, Forel C. Arthrite septique à Yersinia enterocolitica sur prothèse de genou. Méd Mal Infect 2008;38:403 5. [Google Scholar]
- 17.Maeda T, Tanaka C, Shirai T. Yersinia enterocolitica arthritis after total hip arthroplasty-a case report. J Orthop Case Rep 2018;8:24. [Google Scholar]
- 18.Abdullah HM, Oberoi M, Abdalla A, Narayana Gowda S, Ellithi M. Yersinia enterocolitica prosthetic joint septic arthritis successfully treated with ceftriaxone. Case Rep Infect Dis 2021;2021:5547577. [Google Scholar]