The Hartshill rectangle, with sublaminar wiring, offers enduring spinal stabilization for unstable thoracic fractures with spinal cord injuries, enabling early mobilization and reducing neurological risks. It is versatile application spans scoliosis corrections and trauma-related spinal stabilization, reflecting its widespread use in spinal surgery.
Dr. Tanmay Avhad, Department of Orthopaedics, TNMC, and BYL Nair Charitable Hospital, Mumbai, Maharashtra, India. E-mail: tanmayavhad@gmail.com
Introduction: Fractures in the upper thoracic spine pose technical challenges due to the transition from cervical to thoracic spine, often resulting in complete spinal cord injuries necessitating stabilization. Various posterior fixation techniques include Harrington rods, wired distraction rods, L-rods with sub-laminar wiring, and pedicle screw fixation. Luque pioneered sublaminar wiring (SLW), later enhanced by Dove’s Hartshill system for superior biomechanical stability. This case underscores the efficacy of the Hartshill system in stabilizing upper thoracic fractures with severe cord injuries, offering a cost-effective alternative to pedicle screw fixation.
Case Report: A 30-year-old female with polytrauma presented symptoms of lower limb paralysis, bladder and bowel dysfunction, and loss of sensation. Imaging showed a severe D4-D5 fracture with retrolisthesis and spinal cord compression, necessitating surgical stabilization using a Hartshill rectangle with SLW. Following surgery, early rehabilitation and physical therapy were initiated, demonstrating the effectiveness of proper fixation in facilitating early mobilization.
Conclusion: The Hartshill rectangle, with SLW, offers enduring spinal stabilization for unstable thoracic fractures with spinal cord injuries, enabling early mobilization and reducing neurological risks. Its versatile application spans scoliosis corrections and trauma-related spinal stabilization, reflecting its widespread use in spinal surgery.
Keywords: Hartshill rectangle, spinal cord injury, paraplegia, neurodeficit, thoracic fracture, posterior fixation.
The treatment of fractures occurring in the upper thoracic spine presents significant technical and biomechanical challenges owing to the anatomical transition from the flexible cervical spine to the relatively rigid thoracic spine [1]. Fractures that occur between the T1 and T6 vertebrae following trauma frequently result in complete spinal cord injuries and often require stabilization [2]. A variety of posterior instrumentation methods are utilized for fixation, including techniques such as Harrington distraction rods [3], wired distraction rods [4], sub-laminar wiring of L-rods [5], as well as more recent advancements such as pedicle screw fixation [6]. The posterior stabilization of the spine through sublaminar wiring (SLW) was initially pioneered by Luque [7] in 1984. Luque’s technique involved the utilization of wires in conjunction with two distinct rods. Subsequently, in 1986, Dove introduced the Hartshill system, which aimed to enhance rotational stability by integrating the two Luque rods into a rectangular configuration [8]. The rectangular configuration is affixed to the spine, utilizing two loops of wire at each level. This arrangement has demonstrated superior biomechanical performance compared to the original single-loop method, as evidenced by our biomechanical tests [9]. This case highlights the author’s utilization of the Hartshill system for the fixation of unstable fractures occurring in the upper thoracic spine accompanied by severe cord injury. The Hartshill system is regarded as a cost-effective alternative for stabilizing the posterior column, especially in light of recent advancements such as pedicle screws, which address all three columns simultaneously.
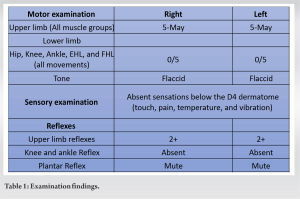
A 30-year-old female who had a history of road traffic accidents leading to polytrauma with injury to her back and face was brought to the emergency unit. The patient was stabilized as per ATLS protocol, and right-sided hemothorax was managed with a chest drain kept in situ. The patient complained of an inability to move both lower limbs associated with loss of bladder and bowel control since the injury. The patient also complained of complete loss of sensation from the chest till the heel of both lower limbs. A provisional diagnosis of a possible spinal cord injury was made and a thorough neurological examination was done to reveal the following findings (Table 1).
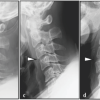
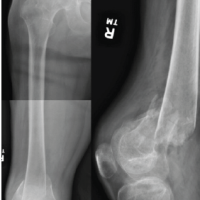
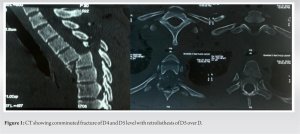
The patient was immediately started on intravenous methylprednisolone loading and maintenance dose as per weight based on the National Acute Spinal Cord Injury Study-2 Protocol [10]. Computed tomography (CT) of the whole spine was advised due to polytrauma, which revealed a comminuted fracture of D4 and D5 levels with retrolisthesis of D5 over D4 (Fig. 1).
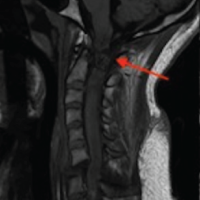
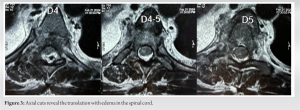
The rest of the spine did not reveal any abnormality. This warranted the need for urgent magnetic resonance imaging (MRI) along with CT cuts to assess the state of neural elements. Further imaging was done to reveal fractures of the inferior end plate of D4 and superior end plate of D5 with Grade-3 retrolisthesis of D5 over D4 with retro-pulsed D5 vertebral body with severe compression of the spinal cord with small fragments present in the canal severe cord edema was present around the listhesis thus correlating with the clinical picture (Fig. 2 and 3).
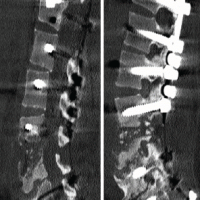
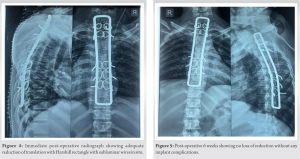
The above MRI findings deemed the neurological prognosis to be extremely poor and were explained to the patient and relatives; however, fixation of the spine was of utmost priority. Due to the level of lesion and presence of fracture subluxation – a plan for multi-level decompression along segmental spinal stabilization with the use of Hartshill rectangle with SLW was planned. The patient was operated on after 24 h under general anesthesia. The surgical procedure involves a posterior midline subperiosteal dissection from T1 to T9, removing spinous processes and interspinous ligaments while creating small windows in the ligamentum flavum at each level. A properly contoured rectangle spans from the leading edge of the uppermost lamina to the trailing edge of the lowermost lamina after the removal of facet joints and preparation of the fusion bed. Two loops of 20-gauge Hartshill wire are passed at each level, with thicker 18-gauge wires used at the ends of longer rectangles. The rectangle is then threaded onto the wires, ensuring proper wire positioning within its corners. Hartshill locators assist in positioning the rectangle against the spine, followed by sequential tightening of wires using a jet twister. Finally, wires are cut, leaving a 1 cm twist length, and confirmation is done through fluoroscopy [8]. Surgery was uneventful, with reduction and rigid fixation from T1 to T9 levels (Fig. 4) patient stabilized over the next few weeks. Signs of upper motor neuron paralysis were seen with spasticity, exaggerated reflexes, and extensor plantars in both lower limbs were noted. The patient was started on thromboprophylaxis along with aggressive physical therapy and rehabilitation using a wheelchair and passive range of motion exercises to prevent contractures. Upper limb strengthening was promoted. Post-operative 6 weeks (Fig. 5), the patient did not show any neurological recovery; however, the prognosis still remains guarded due to the extensive damage to the cord; however, there were no signs of loss of reduction or hardware failure on the radiographs, and the patient could be mobilized.
As third-generation spinal implants have made a resurgence, the relevance of spinal loop rectangle and SLW has been deemed obsolete [11]. The Hartshill rectangle and SLW represent a semi-rigid construct characterized by “cold-cured” dual wires secured to the cortices of both laminae and tightened onto contoured stainless-steel dual rods. Particularly in osteoporotic spines, the cortices of the laminae exhibit greater strength in comparison to the marrow within pedicles and vertebral bodies; hence, from a biomechanical perspective, this construct provides sagittal plane stability through contoured dual rods, along with rotational and/or translational stability facilitated by the cold-cured dual SLWs [12]. However, the disadvantage of this implant is due to its semirigid nature and limited axial stability, this construct permits vertebral collapse to occur, particularly in the absence of anterior column reconstruction [13]. According to the study conducted by Patil et al. [14] involving 50 patients with osteoporotic vertebral fractures treated using the Hartshill system, the method proves its dependability by leveraging the strength of the lamina, which is the sturdier portion of the vertebrae. This reinforces fixation in osteoporotic spine fractures. Moreover, the study underscores its cost-effectiveness, being merely one-tenth of the cost of imported third-generation titanium implants like pedicle screws and rods. In addition, the Hartshill system offers easier instrumentation, a smoother learning curve, and a safer technique, making it suitable for broader societal adoption, particularly in developing nations. In a study conducted by Singh et al. [15] involving 30 adult patients with a mean age of 32 years who suffered from thoracolumbar fractures accompanied by complete or incomplete neurological injuries, management with the Hartshill rectangle resulted in early mobilization starting from the 3rd day post-operation. The study makes us aware of the cost-effectiveness of this approach and emphasizes the minimal equipment required for the implant. Ward et al. [16] investigated the effectiveness of the Hartshill rectangle in stabilizing the spine in 43 patients with complete spinal cord injuries. They found that 19 patients (40%) experienced complications such as painful prominent wires, wire breakage, painful gibbus, infections, and neurological deterioration due to the wires, thus underscoring the importance of accurately implementing the techniques described by Dove [8], as well as the high risk of failure if the procedure is not performed correctly. In their investigation, Mandal et al. [17] conducted a study focusing on the neurological outcomes of posterior stabilization utilizing the Hartshill system for thoracolumbar spine fractures at a rural tertiary care center. They employed Frankel grading to evaluate 35 patients with both complete and incomplete spinal cord injuries. The results indicated neurological improvement in 71% of patients. Moreover, they observed that the presence of dislocation at the injury site correlated with more severe neural deficits. Furthermore, stable fixation of thoracolumbar spine fractures contributed to a reduction in hospital stay and recumbency period, thus facilitating early rehabilitation for patients with spine injuries. Hence spinal stabilization using the Harshill system is an effective treatment modality in managing thoracic fractures and promoting prompt rehabilitation and a cost-effective alternative to the current use of titanium pedicle screws, especially in patients from developing countries and low socioeconomic status.
The use of the Hartshill rectangle with SLW has stood the test of time by providing sufficient spinal stabilization for the management of unstable thoracic fractures accompanied by spinal cord injuries. Its effectiveness ensures early mobilization and rehabilitation, thereby mitigating the risk of further neurological deterioration and secondary complications. In addition, this case underscores the system’s efficacy not only in scoliosis corrections but also in spinal stabilization after trauma, highlighting its widespread adoption in spinal surgery.
The Hartshill rectangle, coupled with SLW, emerges as a pivotal technique in stabilizing unstable thoracic fractures with concurrent spinal cord injuries. This approach not only facilitates early mobilization but also mitigates neurological risks secondary to loss of reduction and hardware complications. Its adaptability extends beyond trauma cases to deformity corrections, being inexpensive and readily available, thus solidifying its status as a cornerstone in spinal surgery.
References
- 1.Fisher C, Singh S, Boyd M, Kingwell S, Kwon B, Li MJ, et al. Clinical and radiographic outcomes of pedicle screw fixation for upper thoracic spine (T1-5) fractures: A retrospective cohort study of 27 cases. J Neurosurg Spine 2009;10:207-13. [Google Scholar | PubMed]
- 2.Quinlan JF, Harty JA, O’Byrne JM. The need for multidisciplinary management of patients with upper thoracic spine fractures caused by high-velocity impact: A review of 32 surgically stabilised cases. J Orthop Surg (Hong Kong) 2005;13:34-9. [Google Scholar | PubMed]
- 3.Böstman OM, Myllynen PJ, Riska EB. Unstable fractures of the thoracic and lumbar spine: The audit of an 8-year series with early reduction using Harrington instrumentation. Injury 1987;18:190-5. [Google Scholar | PubMed]
- 4.Sullivan JA. Sublaminar wiring of Harrington distraction rods for unstable thoracolumbar spine fractures. Clin Orthop Relat Res 1984;189:178-85. [Google Scholar | PubMed]
- 5.Ferguson RL, Allen BL Jr. A mechanistic classification of thoracolumbar spine fracture. Clin Orthop Relat Res 1984;189:77-88. [Google Scholar | PubMed]
- 6.Chang KW. A reduction-fixation system for unstable thoracolumbar burst fractures. Spine (Phila Pa 1976) 1992;17:879-86. [Google Scholar | PubMed]
- 7.Luque ER, editor. Segmental Spinal Instrumentation. Thorofare, NJ: Slack; 1984. [Google Scholar | PubMed]
- 8.Dove J. Internal fixation of the lumbar spine. The Hartshill rectangle. Clin Orthop Relat Res 1986;203:135-90. [Google Scholar | PubMed]
- 9.Dove J, Bottenburg H, Arnold P, Carter SR, Conway J. Biomechanical Aspects of Luque Scgmcntal Spinal Instrumentation. In: Presented at the First European Congress on Scoliosis and Kyphosis. Dubrovnik; 1983. [Google Scholar | PubMed]
- 10.Bracken MB, Shepard MJ, Collins WF, Holford TR, Young W, Baskin DS, et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. N Engl J Med 1990;322:1405-11. [Google Scholar | PubMed]
- 11.Wilber RG, Thompson GH, Shaffer JW, Brown RH, Nash CL Jr. Postoperative neurological deficits in segmental spinal instrumentation. A study using spinal cord monitoring. J Bone Joint Surg Am 1984;66:1178-87. [Google Scholar | PubMed]
- 12.Coe JD, Warden KE, Herzig MA, McAfee PC. Influence of bone mineral density on the fixation of thoracolumbar implants. A comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine (Phila Pa 1976) 1990;15:902-7. [Google Scholar | PubMed]
- 13.Mohan AL, Das K. History of surgery for the correction of spinal deformity. Neurosurg Focus 2003;14:e1. [Google Scholar | PubMed]
- 14.Patil SS, Bhojaraj SY, Nene AM. Safety and efficacy of spinal loop rectangle and sublaminar wires for osteoporotic vertebral compression fracture fixation. Asian J Neurosurg 2017;12:436-40. [Google Scholar | PubMed]
- 15.Singh AM, Waikhom S, Vupru V, Chongthu J. Segmental spinal instrumentation with Hartshill rectangle in thoracolumbar spine trauma. J Med Soc 2010;24:20-2. [Google Scholar | PubMed]
- 16.Ward P, Harvey AR, Ramos J, Carvell JE, Grundy DJ. Hartshill rectangle: Failure of spinal stabilisation in acute spinal cord injury. Eur Spine J 2000;9:152-5. [Google Scholar | PubMed]
- 17.Mandal PK, Ray D, Majhi FR, Tirkey S, Ray MK. Outcome analysis of posterior stabilization of thoracolumbar spine fractures in a rural tertiary care centre--an experience. J Evol Med Dent Sci 2013;2:3104-9. [Google Scholar | PubMed]