Vertebral artery variations can lead to severe complications during anterior cervical discectomy and fusion procedures if proper precaution is not taken.
Mr. Jacob Tiell, Ohio University Heritage College of Osteopathic Medicine, 6775 Bobcat Way, Dublin, Ohio, United States. E-mail: jt944316@ohio.edu
Introduction: Anterior cervical discectomy and fusion (ACDF) is a common cervical procedure with more than 137,000 cases in the United States (U.S.) each year. Historically, ACDF has been a relatively safe procedure despite encountering vital anatomical structures that can risk serious complications. One particularly dangerous sequela of ACDF is the risk of lacerating the vertebral artery (VA). While VA injuries are rare (0.5% of cases), it is crucial for surgeons to prevent this potentially deadly complication with thorough knowledge of VA anatomy. The VA is commonly protected within the transverse foreman; however, anomalies can exist with the artery potentially being found more medial or proximal within the surgical site than expected. The purpose of this article is to report an anomaly found in a cadaveric specimen, where the VA courses within 2 mm of an ACDF plate.
Case Report: A 66-year-old male with a past medical history of coronary artery disease passed away due to complications of a myocardial infarction. During cadaveric dissection, it was discovered that the donor had undergone a previous 3-level (C4-C7) ACDF procedure for an unknown reason. Under further examination, the left VA was observed to take an anomalous medially tracking course before eventually entering the transverse foramina of C5. Left anterior tubercles were absent at the level of C5 and C6 with prominent osteophytes found on the anterior tubercles/transverse foramina of the contralateral side.
Conclusion: There are no studies published on the anatomy of VA variants and their implications on ACDF procedures. ACDF was found to have complication rates in 13.2% of cases. VA variants are observed in up to 20% of the U.S. population and VA injury in ACDF procedures has a rate near 0.5%. With anatomic variations leading to a higher risk of injury, surgeons are required to take further precautionary steps before operating including ordering computed tomography angiography or magnetic resonance angiography films. Understanding the detailed anatomy of the VA and its variants is critical. Using the perspectives of orthopedic spine surgeons, this study supplements the literature on potential VA anomalies encountered in ACDF procedures.
Keywords: Anterior cervical discectomy and fusion, vertebral artery, anomaly, variation, spine.
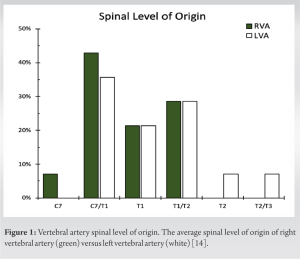
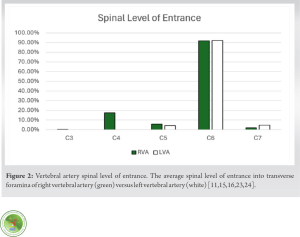
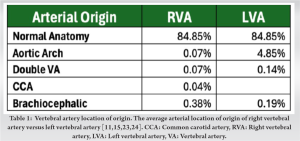
Anterior cervical discectomy and fusion (ACDF) is a common surgical technique used to treat a variety of cervical spinal pathologies including herniated discs and compressed nerves. Accounting for over 137,000 surgical operations in the United States each year [1], this is one of the most performed cervical procedures. The popularity of this procedure is largely due to its high success rate combined with its relatively low rate of complications. A recent study on the overall morbidity rates for ACDF procedures discovered an overall complication rate of 13.2–19.3% with the most common complications being dysphagia (1.7–9.5%), post-operative hematoma (0.4–5.6%), epidural hematoma (0.9%), and exacerbation of myelopathy (0.2–3.3%) [1]. While less likely to occur, vertebral artery (VA) injury is a life-threatening complication of the procedure leading to possible stroke and/or death. VA injury in ACDF procedures has been described in the literature with complication rates ranging from 0.09% to 0.5% [2,3] and incidence rates that increase as the number of levels fused increases [4]. While this rate of incidence is small, the deadly nature of this complication requires serious attention and care to detail. As described in “The Spine” by Rothman and Simeone, the junction of the transverse process and vertebral body marks the lateral cortical wall of the corresponding vertebral body [5]. The VA lies just lateral to this wall of cortical bone and, therefore, identification of these landmarks is critical to staying centered and avoiding VA injury. Using the anatomical borders of the longus colli muscles and uncinate processes, surgeons should be able to operate without putting the VA at risk [5]. However, when an aberrant VA is present, the landmarks may prove ineffective. The current literature describes several different VA anomalies such as variations in spinal level of origin (Fig. 1), arterial location of origin (Table 1), spinal level entering the transverse foramen (Fig. 2), as well as size differences. Out of 18,000+ subjects that have been studied, 84.85% have normal VA anatomy and branching [6-16]. That leaves about 15.15% of the population with one of the anomalies mentioned previously; with more research demonstrating variants may be more common in certain populations [17]. With aberrant VAs being more prevalent than anticipated, it is critical to examine the increased incidence of VA injury during ACDF procedures on patients with anomalous VAs [18-20]. The patient presented in this report demonstrates the level of risk in performing an ACDF on patients who have an anomalous VA. The perspectives of orthopedic spine surgeons were utilized to add to the literature about specific cases of VA anomalies encountered during ACDF procedures. The case report and investigation were approved by Ohio University’s Body Donation Program.
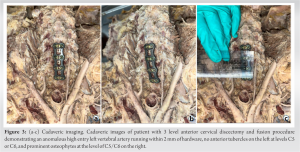
During routine dissection of the VA, an anomaly was discovered on a whole-body donor who had undergone a prior cervical procedure (Fig. 3). The donor was a 66-year-old Caucasian male who passed away due to myocardial infarction. The patient worked as a computer technician and had a known past medical history of coronary artery disease. To ensure the privacy of the family and the donor, medical and/or surgical records were not obtained.
The donor had undergone a 3-level ACDF procedure to fuse levels C4-C7 at some point in his lifetime for an unknown reason. As the procedure appears to have been successful, there are a few interesting anatomical findings to consider. First, there is an aberrant left VA (LVA) originating from the subclavian artery at the level of T1/T2. The LVA takes a slightly medial course before entering the transverse foramen at C5, an unusual high entrance level (Fig. 1). Second, there is an absence of left anterior tubercles at the levels of C5 and C6 with prominent osteophytes on the right anterior tubercles/transverse foramina. Third, the VA runs within 2 mm of the ACDF plate.
The right VA (RVA) originates from the subclavian artery at the level of C7/T1 before entering the transverse foramina of the C6 vertebrae. Therefore, the RVA has a common anatomical path (Fig. 1-3, Table 1).
This case report demonstrates an unusual case of an ACDF with an anomalous course of the LVA. The anterior tubercles appear to have been removed; a feat that would be extremely rare during this procedure. If a surgeon is near the anterior tubercles during ACDF, they are not following the intended protocol. The VA is located just posterior to the anterior tubercles and is at risk of laceration, which would result in a devastating complication of ACDF.
Possible reasons for anterior tubercle removal in this case report could be:
- Previous decompression due to VA stenosis
- The surgeon went too far laterally and removed the tubercles by mistake
- The tubercles were removed during cadaveric dissection.
The patient’s medical history demonstrates atherosclerosis and coronary artery disease as well as cervical osteophytes which were observed during dissection. Therefore, there is a possibility of acquired VA stenosis requiring surgical decompression. However, the medical history obtained was limited. As mentioned previously, it is rare for a surgeon to venture laterally to the anterior tubercles during ACDF; however, if anatomic landmarks are lost, it is possible. Finally, cadaveric dissection was completed with caution by anatomy professors who noted that the anterior tubercles were not removed due to dissection. Each of these hypotheses is a plausible explanation for why the anterior tubercles were removed; however, without the patient’s full medical information, there is no feasible way to delineate the exact causal mechanism.
Another procedure to mention is the increasingly popular artificial disc replacement (ADR). Cervical ADRs have similar, if not wider, exposures and dissections [21] as the ACDF procedure. This in turn leads to similar complications and intraoperative risk factors [22] making knowledge of presenting VA anatomy essential. Typically, the mechanism by which the VA is lacerated intra-operatively is when the surgeon is performing an aggressive decompression into the foramen and then ventures too far laterally. While VA injuries during surgery are rare with incidences up to 0.5% [2, 3], certainly, the risk may be higher in the setting of anomalous anatomy, especially if the surgeon is unaware of pre-operative planning. For this reason, pre-operative films need to be studied meticulously. The current protocol involves closely analyzing all available sequences of MRI, especially sagittal and axial cuts. If there are any concerns, a CT angiography (CTA) or MR angiography (MRA) of the neck should be obtained before surgery. Some surgeons choose to perform a CTA on all pre-operative ACDF and ADR procedures in an attempt to mitigate VA injury. The findings in this case report emphasize the importance of careful analysis of pre-operative imaging when planning an ACDF or cervical ADR. It is imperative that every surgeon has a low threshold for ordering angiographies if there is even the slightest concern for anomaly. The prevalence of these anomalies is far higher than previously reported and can lead to devastating complications intra-operatively.
This original case report uniquely demonstrates the dangers associated with performing ACDF or cervical ADR procedures on patients with VA anomalies and why further pre-operative imaging with CTA/MRA should be utilized in certain cases. ACDF and ADR involve an understanding of the intricate anatomy of the neck, yet it is one of the most frequently performed cervical procedures each year. Identification of anatomic landmarks intraoperatively will aid in the avoidance of VA injury, but the most important safety measure is pre-operative imaging. If a VA anomaly is present, anatomic landmarks may not be enough to prevent laceration.
At present, there are no studies published on the anatomy of VA variants and their implications on ACDF and ADR procedures. While the risk of VA injury is only 0.5%, this means one out of every 200 patients is affected. Further, pre-operative imaging with angiography can play a pivotal role in decreasing the incidence of injury.
References
- 1.Epstein NE. A review of complication rates for anterior cervical diskectomy and fusion (ACDF). Surg Neurol Int 2019;10:100. [Google Scholar]
- 2.Molinari R, Bessette M, Raich AL, Dettori JR, Molinari C. Vertebral artery anomaly and injury in spinal surgery. Evid Based Spine Care J 2014;5:16-27. [Google Scholar]
- 3.Peng CW, Chou BT, Bendo JA, Spivak JM. Vertebral artery injury in cervical spine surgery: Anatomical considerations, management, and preventive measures. Spine J 2009;9:70-6. [Google Scholar]
- 4.Yee TJ, Swong K, Park P. Complications of anterior cervical spine surgery: A systematic review of the literature. J Spine Surg Hong Kong 2020;6:302-22. [Google Scholar]
- 5.Simeone RH, Rothman FA, Herkowitz HN. Rothman-Simeone the Spine. 5th ed. Netherlands: Saunders Elsevier; 2006. p. 830-56. [Google Scholar]
- 6.Berko NS, Jain VR, Godelman A, Stein EG, Ghosh S, Haramati LB. Variants and anomalies of thoracic vasculature on computed tomographic angiography in adults. J Comput Assist Tomogr 2009;33:523-8. [Google Scholar]
- 7.Budhiraja V, Rastogi R, Jain V, Bankwar V, Raghuwanshi S. Anatomical variations in the branching pattern of human aortic arch: A cadaveric study from central India. ISRN Anat 2013;2013:828969. [Google Scholar]
- 8.Komiyama M, Morikawa T, Nakajima H, Nishikawa M, Yasui T. High incidence of arterial dissection associated with left vertebral artery of aortic origin. Neurol Med Chir (Tokyo) 2001;41:8-11. [Google Scholar]
- 9.Lazaridis N, Piagkou M, Loukas M, Piperaki ET, Totlis T, Noussios G, et al. A systematic classification of the vertebral artery variable origin: Clinical and surgical implications. Surg Radiol Anat 2018;40:779-97. [Google Scholar]
- 10.Li X, Guan L, Zilundu PL, Chen J, Chen Z, Ma M, et al. The applied anatomy and clinical significance of the proximal, V1 segment of vertebral artery. Folia Morphol (Warsz) 2019;78:710-9. [Google Scholar]
- 11.Meila D, Tysiac M, Petersen M, Theisen O, Wetter A, Mangold A, et al. Origin and course of the extracranial vertebral artery: CTA findings and embryologic considerations. Clin Neuroradiol 2012;22:327-33. [Google Scholar]
- 12.O’Malley AM, El Kininy WH, Debebe H, Burukan AB, Davy SW. A cadaveric study of aortic arch variation in an Irish population. Ir J Med Sci 2018;187:853-8. [Google Scholar]
- 13.Patil ST, Meshram MM, Kamdi NY, Kasote AP, Parchand MP. Study on branching pattern of aortic arch in Indian. Anat Cell Biol 2012;45:203-6. [Google Scholar]
- 14.Shin IY, Chung YG, Shin WH, Im SB, Hwang SC, Kim BT. A morphometric study on cadaveric aortic arch and its major branches in 25 Korean adults : The perspective of endovascular surgery. J Korean Neurosurg Soc 2008;44:78-83. [Google Scholar]
- 15.Tasdemir R, Cihan OF. Multidetector computed tomography evaluation of origin, V2 segment variations and morphology of vertebral artery. Folia Morphol (Warsz) 2022;82:274-81. [Google Scholar]
- 16.Tetiker H, Çimen M, Kosar MI. Evaluation of the vertebral artery by 3D digital subtraction angiography. Int J Morphol 2014;32:798-802. [Google Scholar]
- 17.Tiell J, Foster J, Mueller C. Vertebral artery variation in the United States: A cadaveric study. Dev Dyn 2023;252:799-800. [Google Scholar]
- 18.Busch G. Anterior fusion for cervical spondylosis. J Neurol 1978;219:117-26. [Google Scholar]
- 19.Khan SA, Coulter I, Marks SM. Iatrogenic vertebral artery injury secondary to vessel tortuosity in a grossly degenerate cervical spine. Br J Neurosurg 2014;28:423-5. [Google Scholar]
- 20.Rosenthal P, Latchaw RE, Kim KD. Anomalous vertebral artery injured during anterior cervical discectomy: A case report. Spine 2013;38:E1567-70. [Google Scholar]
- 21.Leven D, Meaike J, Radcliff K, Qureshi S. Cervical disc replacement surgery: Indications, technique, and technical pearls. Curr Rev Musculoskelet Med 2017;10:160-9. [Google Scholar]
- 22.Turkov D, Job A, Iturriaga C, Verma RB. Current concepts of cervical disc arthroplasty. Int J Spine Surg 2021;15:1174-83. [Google Scholar]
- 23.Yamaki KI, Saga T, Hirata T, Sakaino M, Nohno M, Kobayashi S, et al. Anatomical study of the vertebral artery in Japanese adults. Anat Sci Int 2006;81:100-6. [Google Scholar]
- 24.Uchino A, Saito N, Takahashi M, Okada Y, Kozawa E, Nishi N, et al. Variations in the origin of the vertebral artery and its level of entry into the transverse foramen diagnosed by CT angiography. Neuroradiology 2013;55:585-94. [Google Scholar]