Post-total knee arthroplasty, varus collapse, and bone defects are not rare and careful pre-operative assessment, careful implant removal, re-implantation with thicker stems, and adequate cementing are noteworthy operative strategies to be kept in mind to achieve successful outcome
Dr. Karun Jain, Department of Orthopaedics, Pushpanjali Medical Centre, New Delhi - 110092, India. E-mail: karunjain@live.com
Introduction: The failure of total knee arthroplasties (TKA) due to aseptic implant loosening is now the most common cause of long-term failure. Patients with varus alignment of the tibial or femoral component with additional bone collapse are a specific subset. It is unclear, however, whether implant fixation fails first or if bone collapse occurs first.
Case Report: A 70-year-old lady with 12-year post-primary total knee arthroplasty presented with limping gate with radiological evidence of medial femoral bone collapse and implant loosening. After appropriate pre-operative planning, intraoperatively, after the removal of loose femoral implant which had additional bone loss and careful removal of a well-fixed tibial implant and to prevent collapse due to bone loss, Stryker LCCK implant with long stems on both sides was used. Additional screws on the medial femoral end, along with cement to fill the gap. After 5 years of follow-up, the patient is doing well with a painless full range of movement of the knee joint.
Conclusion: Preoperatively one should always evaluate for bone loss and infection and compare with the other side. In case of aseptic collapse of bones, the use of thicker stems is a good way as these act as weight-sharing implants, and proper cementation during revision TKA is essential.
Keywords: Varus collapse, bone defects, revision total knee arthroplasty.
The failure of total knee arthroplasties (TKA) due to aseptic implant loosening is now the most common cause of long-term failure [1]. Patients with varus alignment of the tibial or femoral component with additional bone collapse are a specific subset. It is unclear, however, whether implant fixation fails first or if bone collapse occurs first. Our case is noteworthy as it involves medial femoral bone collapse (rather than the tibial side) and implant loosening [1, 2]. To ensure appropriate pre-operative planning for such cases, a comprehensive clinical examination is crucial. This includes an assessment of painful joints post-TKA, X-rays to check alignment changes that may indicate loosening, investigation of signs of infection (local skin markers of inflammation, complete blood count, C-reactive protein, serum pro-calcitonin level), and a comparison with the other side. Beforehand, bone loss must also be evaluated (X-rays and computed tomography [CT]) to ensure that the surgeon is well prepared for revision TKA.
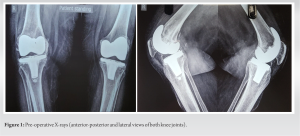
A 70-year-old lady with 12-year post-primary total knee arthroplasty presented with a limping gate with radiological evidence of medial femoral bone collapse and implant loosening. Appropriate pre-operative workup of the case was done along with the counseling for the revision surgery (Fig. 1).
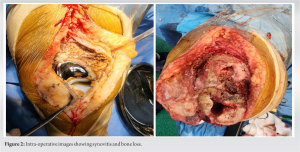
Intraoperatively, we discovered that the femoral implant was loose, but bone loss was still present (Fig. 2) Implant loosening does not always indicate that bone is preserved. Removing the well-fixed tibial implant was a challenge, and we used a thin saw blade meticulously and patiently around the stem to avoid any bone loss. It is essential to clear the tibial canal using a thin saw blade with curettage and ensure proper cementation of the new implant.
To prevent collapse due to bone loss, we utilized stems (Stryker LCCK implant) on both sides and additional screws on the medial femoral end, along with cement to fill the gap (Fig. 3). Ideally, appropriate cones and wedges should be used, but due to economic constraints, we were unable to do so but clinically constrict was very stable. We opted for a semi-constrained type of implant to improve stability, which can be avoided if stability is good intra-operatively. Thicker stems were used in our case for additional stability. The post-operative period was uneventful and periodic follow-up was done. After 5 years of follow-up, the patient is doing well with a painless full range of movement of the knee joint (Fig. 4).
Cox et al. [1] stated that the most frequent mechanism of failure identified was the failure of the implant-cement interface followed by subsequent medial tibial varus collapse in their 88 cases. Improving implant fixation may decrease the incidence of this unique failure mechanism. They advocated the use of supplemental stem fixation in high-risk patients and optimal cementing for all patients as methods of potentially avoiding tibial varus collapse, one of the most frequent modes of long-term failure [1]. Thicker stems should always be used as they function as un-cemented stems, as there is no cement around the stem in our case as well.
Martin et al. [2, 3] studied 1106 revision TKAs performed from 2004 to 2017. Of these, 35 patients were revised secondary to tibial varus collapse. They stated that risk factors for tibial collapse include pre-operative varus deformity, post-operative medial tibial bone loss, and obesity. Therefore, increased tibial stem lengths should be considered in patients with a pre-operative varus deformity, small tibial implant size, and a body mass index ≥35 kg/m2 undergoing primary TKA [2, 3]. Stotter and Von Roth [4] stated that the diagnosis of aseptic loosening poses a great challenge and requires a structured diagnostic algorithm. After the exclusion of infection, conventional radiography is the basic examination, which should be supplemented by CT and nuclear medicine examinations according to the clinical symptoms and the time course [4]. Hampton et al. [5] studied 61 TKAs with aseptic implant loosening and collapse. They concluded that poor cement mantle quality is associated with later aseptic loosening and emphasized the need for surgeons to perform careful cement techniques to reduce the risk of future TKA failure [4-6]. In our case, adequate cementing is done during surgery. Van Otten and Van Loon [7] stated that about 11% of revision TKAs within 1 year of primary TKA is the result of aseptic loosening of the tibial component at the cement-implant interface. A narrative literature review based on publications identified through PubMed and CINAHL databases. Twelve studies were identified, which describe a total of 299 cases of early aseptic loosening of the tibia component at the cement-implant interface. The main associated factors reported were cementation factors. These factors included the use of high-viscosity cement [8], cement application methods, and cement thickness. Other main reported associated factors related to implant design factors included component shape and surface roughness [7-10].
Pre-operative evaluation should always include assessments for bone loss and infection, as well as comparisons with the contralateral side. Intra-operatively, the removal of well-fixed implants and previous bone cement, especially in cases of collapse, presents a significant challenge. A thin saw blade should be used meticulously and patiently to avoid further bone loss. It is also imperative to have a full complement of supportive implants such as screws, plates, bone blocks, cones, wedges, and stems available in the operating room to address any unforeseen issues. Proper cementation is crucial during total knee replacement. Employing thicker stems is advantageous as they function as weight-sharing implants, providing enhanced stability and support.
Post-total knee arthroplasty, varus collapse, and bone defects are common complications. To achieve optimal outcomes, it is essential to employ a comprehensive approach that includes thorough pre-operative assessment, meticulous removal of existing implants, re-implantation with thicker stems, and precise cementing techniques. These operative strategies are critical for addressing these challenges effectively and ensuring the stability and longevity of the prosthesis.
References
- 1.Cox ZC, Green CC, Otero JE, Mason JB, Martin JR. Varus collapse in total knee arthroplasty: Does fixation or bone fail first? J Arthroplasty 2022;37:162-7. [Google Scholar]
- 2.Martin JR, Fehring KA, Watts CD, Springer BD, Fehring TK. Radiographic findings in patients with catastrophic varus collapse after total knee arthroplasty. J Arthroplasty 2018;33:241-4. [Google Scholar]
- 3.Martin JR, Otero JE, Mason JB, Fehring TK. Where is the “Weak Link” of fixation in contemporary cemented total knee replacements? J Arthroplasty 2021;36:2497-501. [Google Scholar]
- 4.Stotter C, Von Roth P. Lockerungsdiagnostik in der Knieendoprothetik [Diagnosis of loosening after knee arthroplasty]. Orthopade 2021;50:972-8. [Google Scholar]
- 5.Hampton CB, Berliner ZP, Nguyen JT, Mendez L, Smith SS, Joseph AD, et al. Aseptic loosening at the tibia in total knee arthroplasty: A function of cement mantle quality? J Arthroplasty 2020;35:S190-6. [Google Scholar]
- 6.Humez M, Fröschen FS, Wirtz DC, Kühn KD. Moderne Zementiertechnik der dritten Generation in der Knie-und hüftendoprothetik [The third-generation modern cementing technique in hip and knee arthroplasty]. Orthopadie (Heidelb) 2023;52:968-80. [Google Scholar]
- 7.Van Otten TJ, Van Loon CJ. Early aseptic loosening of the tibial component at the cement-implant interface in total knee arthroplasty: A narrative overview of potentially associated factors. Acta Orthop Belg 2022;88:103-11. [Google Scholar]
- 8.Kopinski JE, Aggarwal A, Nunley RM, Barrack RL, Nam D. Failure at the tibial cement-implant interface with the use of high-viscosity cement in total knee arthroplasty. J Arthroplasty 2016;31:2579-82. [Google Scholar]
- 9.Cawley DT, Kelly N, McGarry JP, Shannon FJ. Cementing techniques for the tibial component in primary total knee replacement. Bone Joint J 2013;95:295-300. [Google Scholar]
- 10.Hampton M, Balachandar V, Charalambous CP, Sutton PM; CeTIKS study group. Cementing Techniques In Knee Surgery (CeTIKS): a UK expert consensus study. Bone Jt Open 2023;4(9):682-8. [Google Scholar]