Peritalar dislocations might be thought of in a rock-climbing foot accident. Understanding its mechanism is crucial to be able to correct reduce it as quickly as possible.
Dr. Sérgio Soares, Department of Orthopaedics, HFR Fribourg, Chem. Des Pensionnats 2/6, 1752 Villars-sur-Glâne, Switzerland. E-mail: sergiojbs@gmail.com
Introduction: Peritalar dislocations are rare and account for only 1% of all traumatic foot injuries. The talonavicular and the subtalar joints are dislocated; the tibiotalar and calcaneocuboid joints remain intact. Associated injuries are not uncommon. Sports related peritalar dislocations have been reported. However, there are no cases reported on rock climbers.
Case Report: We report the case of a healthy 38-year-old patient, seen after a climbing accident against the wall. He presented a severe varus deformity of the hindfoot and an ankle hematoma and the talar head was palpable laterally against the skin. The radiological assessment showed a medial peritalar dislocation of the left foot. The dislocation was successfully closed reduced in the emergency room under sedation using axial traction and external translation maneuver. Non-operative treatment with cast immobilization and non-weight-bearing was performed for 6 weeks. At 6 months, the patient walked physiologically, without limping. He returned climbing and the subtalar joint did not show any stiffness.
Conclusion: An understanding of the mechanism of injury is necessary to attempt a closed reduction which should be performed as quickly as possible to avoid skin necrosis. An open reduction might be necessary. After reduction, a complete radiological assessment is necessary to exclude associated fractures. The direction of the dislocation, the energy of the accident, the timing of the reduction, as well as the joint’s stability after reduction have a direct impact on the clinical and functional outcomes.
Keywords: Peritalar dislocation, sports, rock climber, subtalar joint, talonavicular joint.
Peritalar dislocations are rare and account for only 1% of all traumatic foot injuries [1]. It is named according to the direction of the foot in relation to the talus [1]. Medial dislocations are the most common type (85%), followed by lateral (15%) and anterior (<1%) [1]. Their common element is that as the talonavicular and the subtalar joints are dislocated, the tibiotalar and calcaneocuboid joints remain intact [2]. Associated osteochondral lesions and other fractures are not uncommon [3]. Sports-related peritalar dislocations have been reported. This injury is also known as basketball foot [4,5]. However, there are no cases reported on rock climbers. We report the case of a young 38-year-old climber, victim of a climbing accident and discuss its particularities.
A healthy 38-year-old patient, recreational climber, was seen in the emergency room after suffering a left foot monotraumatism. He hit his left foot against a climbing wall on a 5C graded track with the foot in equine, varus, and adduction position. He was complaining of a significant pain in his left foot.
On clinical examination, we noticed a locked foot in supination with a varus deformity of the hindfoot, an ankle hematoma, and skin scratches on its lateral aspect (Fig. 1 and 2). The talar head was palpable laterally; he had diffuse pain on palpation on the Chopart joint. Furthermore, the left lower extremity was neurovascularly intact.
The radiological assessment (Fig. 3) demonstrated a medial peritalar dislocation of the left foot and an avulsion-fracture of the base of the 5th metatarsal in zone I.
The left peritalar dislocation was successfully closed and reduced in the emergency room under sedation using axial traction and external translation maneuvers. After reduction, the left lower extremity was immobilized in an open cast boot.
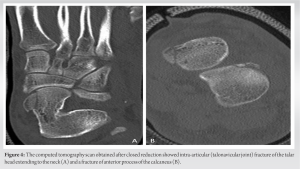
A post-reduction computed tomography (CT) scan of the left ankle and foot was performed to complete the assessment. It showed an optimal reduction of the subtalar and talonavicular joints as well as an intra-articular fracture of the head of the talus extending to the neck, to the medial and posterior process of the talus type I according to Marti classification (Fig. 4) and a fracture of the anterior process of the calcaneus (Fig. 4) [6].
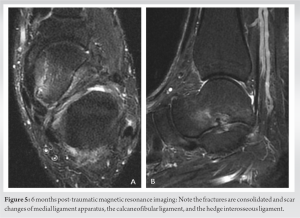
Non-operative treatment with cast immobilization and non-weight-bearing was performed for 6 weeks. At the 6-week follow-up, the cast was removed. The skin lesions had completely healed. No pain on palpation on the left foot was felt. The subtalar and talonavicular joints were stable and we allowed the patient to walk with progressive weight. At 6 months, the patient walked physiologically, without limping. He returned to climbing but not at the same level as before the trauma. The mobility of the ankle in dorsoplantar flexion was 10-0-50° and the subtalar joint was comparable to the right. The mid-foot did not show any stiffness. The magnetic resonance imaging (MRI) of the left foot and ankle showed full consolidation of the above-mentioned fractures and scar changes of the medial ligament apparatus, the calcaneofibular ligament, and the medial interosseous ligament (Fig. 5). However, the talus still had some bone marrow lesions.
Anatomy
The subtalar joint is a complex synovial joint in the hindfoot [7]. Functionally, it is a plane joint [8]. It is formed by the talus superiorly and the calcaneus and navicular inferiorly. The talus and the calcaneus share three articulating surfaces. The anterior small facet articulates between the talus head and the anterior calcaneus facet, the middle facet between medial facet of talus and the middle facet of the calcaneus, and finally the large posterior facet between the posterior facet of talus and the posterior facet of the calcaneus [9].
Anatomically, it consists of two groups of joints:
- The talocalcaneal navicular joint is formed by the anterior and middle facets, stabilized by the strong plantar calcaneo-navicular ligament (spring ligament) [9]. Its insufficiency can lead to a progressive collapsing foot deformity [7].
- The posterior talocalcaneal joint is formed by the posterior facet.
Both joints have a common single axis of motion and movement is dependent on the other, therefore working as one functional unit [10].
Mechanism of injury
The trauma causing a peritalar dislocation is often a fall from a considerable height (30–90%), and about 50% from a motor vehicle accident [11]. There are a significant number of patients who feature shock trauma after jumps during a basketball game [11]. The medial peritalar dislocation is a consequence of an inversion force applied to a plantar-flexed foot [12]. Our patient might have suffered these movements over his foot. However, this is an extremely unlikely combination on a rock climbing accident against the wall. This athletes most likely impact their feet in dorsiflexion, external rotation, and valgus of the hindfoot. The dorsal talonavicular ligament is the first to be injured, then the two bundles of the hedge interosseous ligament of the sinus tarsi, and finally the calcaneofibular ligament [13]. The sustentaculum tali is the fulcrum around which the neck of the talus hinges. Hence, the first joint to dislocate is the talonavicular followed by the subtalar joint. The calcaneus gets medially displaced and the talar head remains between the extensor hallucis longus and the extensor digitorum longus. Peritalar joint dislocation is a rare condition in rock climbers. To the best of our knowledge, there are no cases reported in the literature. Upper extremity trauma is usual during climbing (pulley injury, lumbrical shift syndrome, extensor tendon syndrome, and epiphyseal fatigue fractures). Lower extremity injuries are mostly a result of a fall from height (fractures of calcaneus, talus, and ankle joint) as well as an impact against the wall. Hindfoot sprain, ankle sprains, lateral process of the talus’ fractures, and soft-tissue injury are especially caused using by the soft and flexible shoes used for climbing [14]. Chronic foot problems (nail dystrophy and toes deformities) are in high skilled rock climbers [13].
Diagnosis
The diagnosis is clinical and must be confirmed by plain radiographs. Under suspicion of a peritalar dislocation, a closed reduction on an emergent basis should be tried in the emergency department even before plain radiographs are obtained to diminish pressure over the soft tissues and avoid skin necrosis by the talar head [15]. Adequate muscle relaxation must be required to achieve a closed reduction. If the radiological assessment does not delay the reduction, then it should be obtained to help directing the closed reduction. However, a post-reductional radiological assessment is necessary to confirm a good joint congruence. As fractures occur in 12–38% of peritalar dislocations, CT scan and a MRI of the foot are necessary to exclude associated osteoligamentous lesions [16].
Treatment
Closed reduction
A closed reduction is the preferred treatment for most of the peritalar dislocations. The gastrocnemius-soleus complex must be relaxed to decrease its pull on the calcaneus and this is achieved by flexing the knee to 90°. The most common reported cause of irreducibility for medial peritalar dislocations is button-holding of the talar head through the extensor retinaculum of the extensor digitorum brevis [17-19]. The deep peroneal neurovascular bundle might be also a cause of impingement impeding the reduction [2]. Multiple attempts are not recommended. Once the reduction is achieved, the joint is normally stable due to the shape and fit of the articular surfaces.
Open reduction
Open reduction is indicated for open injuries and when closed reduction fails or there is a tendency for redislocation. The literature reports the need for an open reduction in 2–38% [20, 21].
Rehabilitation protocol
A possible complication of peritalar dislocations is post-reduction instability. Hence, short-term immobilization is recommended [22]. To reduce the subtalar joint stiffness and other associated symptoms, the uncomplicated medial peritalar dislocation should not be immobilized longer than 4 weeks. If there are associated fractures, the immobilization should not exceed 6 weeks. Sixty percentages of patients immobilized in a long cast for 8 weeks were found to have developed subtalar arthrosis [23]. Physiotherapy with immediate mobilization a full-weight-bearing should follow [1, 5, 24].
Prognosis
The lower the trauma energy, the more favorable the long-term results are [25]. A mild degree of subtalar joint’s arthritis is well tolerated [12]. Dislocations with associated intra-articular fractures are more prone to result in arthritic changes causing stiffness of the subtalar joint [1, 3, 5]. Talar necrosis after peritalar dislocation is a quite rare finding despite talar’s susceptibility.
We report the first case of a peritalar dislocation occurring in a rock climber. Emergency management is required. An understanding of the mechanism of injury is necessary to attempt a closed reduction which should be performed as quickly as possible to avoid skin necrosis. An open reduction might be necessary. After reduction, a complete radiological assessment is necessary to exclude associated fractures. The direction of the dislocation, the energy of the accident, the timing of the reduction, as well as the joint’s stability after reduction have a direct impact on the clinical and functional outcomes.
Understanding peritalar dislocation’s mechanism of injury is essential to be able to correct and reduce it as quickly as possible.
References
- 1.Freund KG. Subtalar dislocations: A review of the literature. J Foot Surg 1989;28:429-32. [Google Scholar]
- 2.Heck BE, Ebraheim NA, Jackson WT. Anatomical considerations of irreducible medial subtalar dislocation. Foot Ankle Int 1996;17:103-6. [Google Scholar]
- 3.Bohay DR, Manoli A 2nd. Occult fractures following subtalar joint injuries. Foot Ankle Int 1996 Mar;17:17(3)164-9. [Google Scholar]
- 4.Grantham SA. Medical subtalar dislocation: Five cases with a common etiology. J Trauma Inj Infect Cri Care 1964 Nov;4(6):845-9. [Google Scholar]
- 5.Merianos P, Papagiannakos K, Hatzis A, Tsafantakis E. Peritalar dislocation: A follow-up report of 21 cases. Injury 1988 Nov;19(6):439-42. [Google Scholar]
- 6.Marti R. Talus and Calcaneus frakturen Frakturbehandlung bei Kindern und Jugendlichen. Weber B, Brunner C, Freuler F, editors. New York, Berlin, Heidelberg: Springer; [Google Scholar]
- 7.Krähenbühl N, Horn-Lang T, Hintermann B, Knupp M. The subtalar joint: A complex mechanism. EFORT Open Rev 2017 Jul;2(7):309-16. [Google Scholar]
- 8.Rockar PA Jr. The subtalar joint: Anatomy and joint motion. J Orthop Sport Phys Ther 1995 Jun;21(6):361-72. [Google Scholar]
- 9.Turner AJ, Hick PE. Inhibition of aldehyde reductase by acidic metabolites of the biogenic amines. Biochem Pharmacol 1975 Sept;24(18):1731-3. [Google Scholar]
- 10.Lapidus PW. Subtalar joint, its anatomy and mechanics. Bull Hosp Joint Dis 1955 Oct;16(2):179-95. [Google Scholar]
- 11.Wagner R, Blattert TR, Weckbach A. Talar dislocations. Injury 2004 Sep;35(2):36-45. [Google Scholar]
- 12.Saltzman C, Marsh JL. Hindfoot dislocations: When are they not benign? J Am Acad Orthop Surg 1997 Jul ;5(4):192-8. [Google Scholar]
- 13.Schöffl V, Küpper T. Feet injuries in rock climbers. World J Orthop 2013;4(4):218. [Google Scholar]
- 14.Neuhof A, Hennig FF, Schöffl I, Schöffl V. Injury risk evaluation in sport climbing. Int J Sports Med 2011 Oct 12;32(10):794-800. [Google Scholar]
- 15.Ruhlmann F, Poujardieu C, Vernois J, Gayet LE. Isolated acute traumatic subtalar dislocations: Review of 13 cases at a mean follow-up of 6 years and literature review. J Foot Ankle Surg 2017 Jan;56(1):201-7. [Google Scholar]
- 16.Melenevsky Y, Mackey RA, Abrahams RB, Thomson NB 3rd. Talar fractures and dislocations: A radiologist’s Guide to timely diagnosis and classification. Radiographics 2015 May;35(3):765-79. [Google Scholar]
- 17.Cohen MG, Garcia JF, Worrell RV. Imaging rounds #106. Medial subtalar dislocation. Orthop Rev 1991;20(5):466, 468, 470-2. [Google Scholar]
- 18.Leitner B. Obstacles to reduction in subtalar dislocations. J Bone Joint Surg Am 1954;36(A:2):299-306. [Google Scholar]
- 19.Pehlivan O, Akmaz I, Solakoglu C, Rodop O. Medial peritalar dislocation. Arch Orthop Trauma Surg 2002 Jan;122(9):541-3. [Google Scholar]
- 20.DeLee JC, Curtis R. Subtalar dislocation of the foot. J Bone Joint Surg Am 1982;64(3):433-7. [Google Scholar]
- 21.Valdivieso TR, de Miguel Vielba JA, Garcia CH, Castrillo AV, Posadas JI, Martin MM. Subtalar dislocation. A study of nineteen cases. Int Orthop 1996 Apr 24;20(2):83-6. [Google Scholar]
- 22.Zimmer TJ, Johnson KA. Subtalar dislocations. Clin Orthop Relat Res 1989;238:190-4. [Google Scholar]
- 23.Christensen SB, Lorentzen JE, Krogsøe O, Sneppen O. Subtalar dislocation. Acta Orthop Scand 1977 Jan 8;48 (6):707-11. [Google Scholar]
- 24.Marcinko DE, Zenker CC. Peritalar dislocation without fracture. J Foot Surg 1991;30(5):489-93. [Google Scholar]
- 25.Perugia D, Basile A, Massoni C, Gumina S, Rossi F, Ferretti A. Conservative treatment of subtalar dislocations. Int Orthop 2002 Feb;24:26(1):56-60. [Google Scholar]