Despite advances in implants and techniques of internal fixation, tibia plafond fractures still pose a considerable challenge to the orthopedic surgeon due to the unforgiving nature of the soft tissue envelope, difficulties in achieving anatomical reduction of the articular surface and post-operative stiffness of the ankle.
Dr. Hardik Meisheri, Department of Orthopedics, Military Hospital Chennai, Defence Colony 1st Ave, Nandambakkam, Guindy, Chennai - 600032, Tamil Nadu, India. E-mail: meisherihardik@gmail.com
Introduction: Tibial pilon fractures, involving the weight-bearing surface of the distal tibia, present a formidable challenge for orthopedic surgeons due to their complex nature and the delicate soft tissue envelope surrounding the ankle joint.Early approaches to pilon fractures often resulted in poor outcomes, but modern principles of internal fixation and anatomical reconstruction have significantly improved patient prognosis. Despite advancements in surgical techniques and implants, achieving anatomical reduction of the articular surface remains a significant hurdle.
Case Report: This article presents a case report of a 27-year-old male soldier who sustained bilateral tibial pilon fractures following a fall from height. The patient underwent surgical intervention with differing approaches due to the complexity of the fractures. A combination of minimally invasive plate osteosynthesis (MIPPO) and external fixation was employed to address the fractures. The patient was followed up for 06 months post-op.
Conclusion: The importance of respecting the soft tissue envelope in surgical planning and timing, as well as the role of advanced imaging techniques such as CT scanning in preoperative assessment is crucial to achieving a successful outcome.While tibial pilon fractures remain complex injuries, advancements in surgical management have led to improved outcomes. However, ongoing research and innovation are necessary to address the multifaceted challenges associated with these fractures and optimize patient care.
Keywords: Pilon, MIPPO, ex-FIX
Fractures of the distal articular surface of the tibia are commonly referred to as pilon or plafond fractures. Tibial plafond fractures frequently present a challenge to the orthopedic surgeon [1]. First described by French radiologist Destot in 1911 [2]. Pilon fractures are defined as injuries that involve the articular weight-bearing surface of the distal tibia. The term “pilon” is derived from the French language, meaning pestle, resembling a pharmacist’s pestle when paralleled to the distal tibial metaphysis. Later termed “plafond” meaning “ceiling” in the French language, equating the distal tibial articular surface as the ceiling of the ankle joint [3]. Tibial pilon fractures are relatively infrequent, accounting for 5–7% of all fractures of the tibia [1]. These fractures are caused by axial loading in which the talus is driven into the plafond, resulting in articular impaction of the distal tibia. Intra-articular distal tibia fractures can also occur from a rotational force with minimal axial load. Despite advances in implants and techniques of internal fixation, tibia plafond fractures still pose a considerable challenge to the orthopedic surgeon due to the unforgiving nature of the soft tissue envelope, difficulties in achieving anatomical reduction of the articular surface and post-operative stiffness of the ankle (esp. if external fixator has been applied).
History
A 27-year-old male, general duty soldier sustained a vertical fall from a height (10 feet) after losing his balance. He landed on both his feet with a direct axial load. He was unable to walk and was taken to a nearby hospital. He was managed with bilateral above-knee POP posterior slab immobilization and transferred to our center 2 days later.
Examination
His physical examination revealed swollen ankles and ecchymosis bilaterally, with a blister over the lateral aspect distal 1/3rd leg. There were no open wounds and the neurovascular state was completely intact.
Pre-operative evaluation
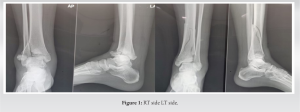
Plain radiographs of both ankles revealed comminuted tibial plafond fractures bilaterally (Fig. 1). Preoperatively, computed tomography (CT) scan was done for both ankles.
Intra-op findings
For the left side, an anterolateral minimally invasive approach was taken. The articular surface was visualized and the plate was inserted using minimally invasive percutaneous plate osteosynthesis technique. The fracture at the metaphysis was reduced and fixed with a lag screw through the plate. The articular surface reduced on its own once the fracture was reduced at the metaphysis.
The right side was more complicated and difficult to align. The fracture was approached through a medial and anterolateral approach, giving due respect to the surrounding soft tissue which was already compromised. On visualizing the articular surface, multiple small bony fragments were seen. The articular fragments were found to be impacted. Hence, an external fixator delta frame was applied to achieve distraction at the fracture site and help keep the fragments aligned. The fracture was further fixed with an anterolateral plate and a 03-hole 1/3rd tubular plate medially.
Post-operative
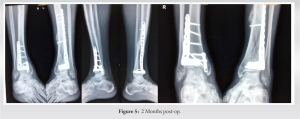
There were no soft-tissue complications or infections. The left side was mobilized immediately, while the external fixator on the right side was kept for 6 weeks. The patient was advised non-weight-bearing ambulation (wheelchair ambulation). After 6 weeks the external fixator was removed. There were no signs of any pin tract infections. The right ankle was mobilized.
Follow-up
At 2-month, post-operative patient started weight bearing. At present, patient is ambulant full weight bearing without support. The patient is able to dorsiflex his right ankle up to 100 and plantarflex up to 300, while his left ankle is able to dorsiflex up to 200 and plantarflex up to 450. At 6 months post-operative, his fracture had clinically and radiologically united. He was able to squat and was able to carry out his activities of daily living without any complaint.
Tibia pilon fractures were for many years considered as “not amenable to surgery” and the patients were forced to accept the usually poor late result as a matter of bad luck. And even in those instances where the open reduction was tried and some sort of mostly inadequate screw or wire fixation was attempted, the results were usually not encouraging [4]. The modern concept of fracture treatment by means of open, anatomical reconstruction, stable internal fixation, and functional aftercare has been able to change this rather fatalistic attitude dramatically. In 1968–1969 Reudi and Allgower [5] reported for the first time on a consecutive series of 84 pilon fractures exclusively treated by internal fixation. A good to excellent functional outcome in 74% of patients at 4 years of follow-up proved the success of this method.
Rüedi-Allgöwer classification was derived from the evaluation of rotational injuries sustained following skiing accidents [4, 6]. Three different fracture types based on comminution and displacement of the articular surface were proposed. Type I is intra-articular fractures without displacement, Type II is displaced fractures without comminution, and Type III are displaced fractures with impaction and comminution. The arbeitsgemeinschaft für osteosynthesefragen/orthopedic trauma association (AO/OTA) offers a more comprehensive classification system dividing up pilon fractures into Types A, B, and C with subsequent subtypes. Type A is extra-articular fractures, Type B is partial articular involving a single column, and Type C is complete articular fractures, all with subtypes differentiated on fracture pattern, amount of comminution, and presence or location of impacted articular fragments. Likely due to the nature and variability of the multitude of possible fracture patterns, this classification is very inclusive and descriptive but shows inconsistent inter-observer reliability [7-10].
AO/OTA and Ruedi-Allgower classification systems are based on plain radiographs and are not useful tools in terms of pre-operative planning or prognostic indicators. Given these limitations, Leonetti and Tigani proposed a new classification system based on displacement, the number of articular fragments, the plane of the main fracture line, and the degree of comminution as seen on a CT scan. This is the only CT-based classification system described. In an associated study of 71 pilon fractures, they demonstrated that this new classification system is not only reproducible but provides prognostic correlation [11]. Regardless of which classification system is used, it is important to recognize that there is a high degree of variation between individual fractures. For this reason, a pre-operative CT scan is vital in understanding the fracture and planning both surgical approaches and fixation.
Patients involved in high-energy trauma should be treated according to advanced trauma life support guidelines because they may have associated life- or limb-threatening injuries. Edema, pain, deformity, and functional impairment are the classic clinical signs of most fractures. The inability to sustain the weight of the body is particularly indicative. High-energy fractures are usually obvious on inspection, while tibial pilon fractures caused by a torsional mechanism often have less striking clinical signs. Extreme care should be taken in clinical examination to look for possible associated injuries, especially vascular or nerve injury, and compartment syndrome, requiring urgent intervention [12-15]. A thorough evaluation of the skin should be done at the time of the initial encounter, assessing for the degree of swelling, presence or absence of skin wrinkles, blistering, and open wounds [16]. The standard radiographic examination includes anteroposterior, mortise, and lateral projections and must include the entire tibia and fibula and the foot. CT scanning, with 3D reconstruction, has now become routine in many centers for the study and operative planning of these high-energy fractures, proving especially useful to identify the precise path of sagittal and coronal fracture lines [17, 18].
The tibial plafond fracture pattern and soft-tissue injury are dictated by the positioning of the foot at the time of injury. Typically, the talus is driven into the plafond during a high-energy axial load. The position of the foot at the time of impact, in conjunction with the direction and amplitude of the force, results in varying fracture patterns and amount of comminution [16]. When the foot is plantar-flexed at the time of injury, forces are directed into the posterior portion of the articular surface leading to impaction and posterior talar displacement. The opposite is true when the foot is dorsiflexed, the energy is transmitted through the anterior region. Neutral foot positioning results in a purely vertical vector engaging the entire articular surface, resulting in both anterior and posterior column fractures with variable varus and valgus angulation. When the force is predominantly midline or medial to the ankle, the fracture will result in a varus deformity. Similarly, when exerted lateral to the center of the ankle, valgus configuration results. Evaluation of the fibula can provide further information on the stability of the injury. For example, an intact fibula can necessitate medial column instability and varus deformity while the opposite is true when the fibula is involved [14, 19, 20]. The most common fracture pattern usually splits the articular surface into three variable yet predictable fragments: The medial fragment consisting of the medial malleolus and adjacent weight-bearing segment, the anterolateral or Chaput fragment, and the posterolateral or Volkman fragment usually with their ligamentous attachments intact [21]. The location of where these fracture lines exit the cortex, the position of articular segments, and if those fragments lie in continuity with the intact tibial shaft dictate the location of implant placement and subsequently, the surgical approach(es) used. In 1968–1969 Reudi and Allgower [5] treated 84 pilon fractures exclusively by internal fixation following the four principles: (1) Reconstruction of the correct length of the fibula. (2) Reconstruction of the articular surface of the tibia. (3) Introduction of a cancellous autograft to fill in the bone defect in the metaphysis of the tibia. (4) Stabilization of the medial aspect of the tibia by a plate. Even after more than 50 years, since Reudi and Allgower published their findings, these principles are still used to guide the management of tibial pilon fractures. Given the unforgiving soft tissue envelope about the distal tibia, it is the state of the soft tissues that dictates the timing of surgery and the degree of surgical insult. Staged protocols were introduced in which fractures were temporized in calcaneal traction, splints, or external fixators until the soft tissue envelope was amenable to surgery. Unfortunately, no definitive clinical signs exist to determine the timing for definitive fixation. Surgeons frequently use the presence of wrinkles or epithelialization of fracture blisters, but often it is a general “gestalt” [16]. Staged protocols resulted in decreased wound complications; however, they have recently been challenged with a resurgence of early fixation. Concerns regarding quality of reduction, operative time, increased healthcare costs, and pin site infection with the use of external fixators have led a number of surgeons to proceed with definitive internal fixation acutely. Multiple recent studies have shown that fractures treated within 72 h of surgery have comparable outcomes to staged fixation [22-24]. However, it is our general practice to determine the timing of surgery and the need for staging based on the quality of the soft tissue envelope, with the presence of soft tissue wrinkles as our primary determining factor. AO principles dictate anatomic reduction and absolute stability of the articular surface for any intra-articular fracture. It is believed that restoration of the articular surface decreases the risk of post-traumatic arthritis, ultimately leading to improved outcomes. However, while the quality of articular reduction has been shown to affect radiographic arthrosis, studies have been unable to demonstrate a link between the quality of articular reduction and outcomes [25]. While a more recent prospective study by Sommer et al. demonstrated a link between restorations of fibular length with functional outcomes, there was no correlation found between articular step-off and articular gap [26]. However, the mean step-off in this series was 0.03 mm, and the mean gap was 0.13 mm, which may represent good to excellent articular reductions in the majority of patients. In this case, we used an external fixator to achieve distraction at the fracture site, which helped in reducing the impacted fracture fragments at the articular surface. It remains our belief that the articular reduction is still a valuable piece of the puzzle, and we must continue to strive for an anatomic reduction whenever feasible.
Tibial pilon fractures are complicated injuries that are difficult to manage for even experienced orthopedic surgeons. The articular cartilage injury, metaphyseal comminution, and soft tissue insult are responsible for poor outcomes. Respect for the soft tissue envelope is the first step in minimizing complications. While open reduction and internal fixation remains the mainstay for the treatment of the majority of these fractures, additional treatment modalities, such as external fixation and primary arthrodesis, are emerging and should be considered for more complex cases. Advances in surgical techniques and implants have resulted in improved outcomes, but the overall prognosis for these injuries frequently remains poor. Further study and research are required to improve results as well as the quality of life of patients affected by pilon fractures.
Tibial pilon fractures still remain a challenge to the orthopedic surgeon. The articular cartilage injury, metaphyseal comminution, and soft tissue insult are responsible for poor outcomes. Respect for the soft tissue envelope is the first step in minimizing complications. Advances in surgical techniques and implants have resulted in improved outcomes, but the overall prognosis for these injuries frequently remains poor.
References
- 1.Mauffrey C, Vasario G, Battiston B, Lewis C, Beazley J, Seligson D. Tibial pilon fractures: A review of incidence, diagnosis, treatment, and complications. Acta Orthop Belg 2011;77:432-40. [Google Scholar]
- 2.Destot E. Traumatismes du Pied et Rayons x Malleoles, Astragale, Calcaneum, Avant-Pied. Paris: Masson; 1911. p. 1-10. [Google Scholar]
- 3.Saad BN, Yingling JM, Liporace FA, Yoon RS. Pilon fractures: Challenges and solutions. Orthop Res Rev 2019;11:149-57. [Google Scholar]
- 4.Rüedi TP, Allgöwer M. The operative treatment of intra-articular fractures of the lower end of the tibia. Clin Orthop Relat Res 1979;138:105-10. [Google Scholar]
- 5.Reudi TP, Allgower M. Fractures of the lower end of the tibia into the ankle joint: Results 9 years after open reduction and internal fixation. Injury 1969;2:92-9. [Google Scholar]
- 6.Rüedi T, Matter P, Allgöwer M. Intra-articular fractures of the distal tibial end. Helv Chir Acta 1968;35:556-82. [Google Scholar]
- 7.Dirschl DR, Adams GL. A critical assessment of factors influencing reliability in the classification of fractures, using fractures of the tibial plafond as a model. J Orthop Trauma 1997;11:471-6. [Google Scholar]
- 8.Martin JS, Marsh JL, Bonar SK, DeCoster TA, Found EM, Brandser EA. Assessment of the AO/ASIF fracture classification for the distal tibia. J Orthop Trauma 1997;11:477-83. [Google Scholar]
- 9.Ramappa M, Bajwa A, Singh A, Mackenney P, Hui A, Port A. Interobserver and intraobserver variations in tibial pilon fracture classification systems. Foot (Edinb) 210;20:61-3. [Google Scholar]
- 10.Swiontkowski MF, Sands AK, Agel J, Diab M, Schwappach JR, Kreder HJ. Interobserver variation in the AO/OTA fracture classification system for pilon fractures: Is there a problem? J Orthop Trauma 1997;11:467-70. [Google Scholar]
- 11.Leonetti D, Tigani D. Pilon fractures: A new classification system based on CT-scan. Injury 2017;48:2311-7. [Google Scholar]
- 12.Bhattacharyya T, Crichlow R, Gobezie R, Kim E, Vraha MS. Complications associated with the posterolateral approach for pilon fractures. J Orthop Trauma 2006;20:104-7. [Google Scholar]
- 13.Kline AJ, Gruen GS, Pape HC, Tarkin IS, Irrgang JJ, Wukich DK, et al. Early complications following the operative treatment of pilon fractures with and without diabetes. Foot Ankle Int 2009;30:10421047. [Google Scholar]
- 14.Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma 1999;13:78-84. [Google Scholar]
- 15.Tarkin IS, Clare MP, Marcantonio A, Pape HC. An update on the management of high-energy pilon fractures. Injury 2008;39:142-154. [Google Scholar]
- 16.Bear J, Rollick N, Helfet.D. Evolution in management of tibial pilon fractures. Curr Rev Musculoskelet Med 2018;11:537-45. [Google Scholar]
- 17.Topliss CJ, Jackson M, Atkins RM. Anatomy of pilon fractures of the distal tibia. J Bone Joint Surg Br 2005;87:692-7. [Google Scholar]
- 18.Tornetta P 3rd, Gorup J. Axial computed tomography of pilon fractures. Clin Orthop Relat Res 1996;323:273-6. [Google Scholar]
- 19.Teeny SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res 1993;292:108-17. [Google Scholar]
- 20.McFerran MA, Smith SW, Boulas HJ, Schwartz HS. Complications encountered in the treatment of pilon fractures. J Orthop Trauma 1992;6:195-200. [Google Scholar]
- 21.Cole PA, Mehrle RK, Bhandari M, Zlowodzki M. The pilon map: Fracture lines and comminution zones in OTA/AO type 43C3 Pilon fractures. J Orthop Trauma 2013;27:e152-6. [Google Scholar]
- 22.White TO, Guy P, Cooke CJ, Kennedy SA, Droll KP, Blachut PA, et al. The results of early primary open reduction and internal fixation for treatment of OTA 43.C-type tibial pilon fractures: A cohort study. J Orthop Trauma 2010;24:757-63. [Google Scholar]
- 23.Tang X, Liu L, Tu CQ, Li J, Li Q, Pei FX. Comparison of early and delayed open reduction and internal fixation for treating closed tibial pilon fractures. Foot Ankle Int 2014;35:657-64. [Google Scholar]
- 24.Liporace FA, Yoon RS. Decisions and staging leading to definitive open management of Pilon fractures: Where have we come from and where are we now? J Orthop Trauma 2012;26:488-98. [Google Scholar]
- 25.Williams TM, Nepola JV, DeCoster TA, Hurwitz SR, Dirschl DR, Marsh JL. Factors affecting outcome in tibial plafond fractures. Clin Orthop Relat Res 2004;423:93-8. [Google Scholar]
- 26.Sommer C, Nork SE, Graves M, Blauth M, Rudin M, Stoffel K. Quality of fracture reduction assessed by radiological parameters and its influence on functional results in patients with pilon fractures-a prospective multicentre study. Injury 2017;48:2853-63. [Google Scholar]